Correlation of serum 25 OH vitamin D levels in myopic and non myopic young adults along with its association with grades of myopia
Received: 04-Feb-2021 Accepted Date: Feb 18, 2021; Published: 25-Feb-2021
Citation: Singh L, Alpana, Chandra A. Correlation of serum 25-OH vitamin D levels in myopic and non-myopic young adults along with its association with grades of myopia. Opth Clin Ther. 2021;5(2):1-5.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Purpose: To study the levels of serum 25-OH vitamin D in myopic young adults and to compare the results in different grades of myopia.
Methods: 200 subjects aged between 13 to 28 years, participated in this hospital-based case control study. All myopes (n=100) and non-myopes (n=100) underwent a comprehensive ophthalmic examination, including post-cycloplegic refraction after taking consent and ethical clearance. The participants provided data about age, education, outdoor activity, and urbanization. Myopia was graded into pre-myopia, low myopia and high myopia as per international myopia institute grading 2019. Fasting blood samples were taken and analyzed for 25-OH vitamin D levels, using vitros immunoassay analyzer. Serum 25-OH vitamin D concentrations levels were compared and association between myopia and its severity grades was determined.
Results: In the myopic study group (n=100), 30% had pre-myopia, 40% had low-myopia and 30% had high myopia. Serum 25-OH vitamin D levels were significantly different between cases and controls, with lower levels measured in myopia (p<0.01). Age and gender correlation were not significant in this study with 25-OH vitamin D levels in myopia. Status of insufficiency and deficiency of 25-OH vitamin D levels was significantly higher in high myopes.
Conclusion: Low serum 25-(OH) vitamin D levels were found to be associated with myopia in young adults. The fall in levels of 25-OH vitamin D level was directly proportional to the increasing severity of myopia.
Keywords
Myopia; 25-Hydroxyvitamin D; Young adults
Introduction
Myopia is one of the most common ocular disorders worldwide [1], particularly in East Asia. Myopia is defined in various ways, in order to form a relation to the retinal image formation. The current version of the World Health Organization’s (WHO) International Classification of Disease (ICD-10) provides the following definition for myopia:
A refractive error in which rays of light entering the eye parallel to the optic axis are brought to a focus in front of the retina when accommodation (accommodation, ocular) is relaxed. This results from an overly curved cornea or from the eyeball being too long from front to back. It is also called near sightedness” [2].
The recently released ICD-11 for mortality and morbidity statistics (2018) includes the same definition [2].
Myopia is a common and a considerably benign disorder, and vision can be corrected with spectacles, contact lenses, or laser refractive surgery. In certain individuals, presenting with severe myopia, however are at increased risk of vision threatening conditions and blindness due to associated conditions such as retinal detachment, macular and retinal degeneration, foveoschisis, rhegmatogenous retinal detachment and choroidal neovascularization [3,4].
To stop the rate of progression of myopia is the current goal. It is important to focus on studies that are targeted on preventing the onset of myopia. This requires identification of risk factors and treats the eyes before they become myopic.
Longitudinal observational studies, such as the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) study, have demonstrated that eyes destined to become myopic show an accelerated pattern of axial elongation several years before the onset of myopia [5].
Genetic and environmental factors play a role in contribution of its development, the cause of myopia is as yet unclear [6,7]. Numerous studies have shown that certain environmental factors such as parental myopia, duration of near work, academic performance, time spent outdoors and urbanization have been associated with the development of myopia [8-10]. There is also adequate evidence through animal studies, clinical trials and population studies that there is a link between myopia and insufficient time spent outdoors.
Two main theories have been put forward to explain the relationship. Firstly, the bright light from the sun is beneficial in releasing enhanced levels of dopamine in the retina [11,12] and secondly that its beneficial effect results from increased serum 25-hydroxyvitamin D (25(OH)D) [13].
Hence, a possible risk factor for development of myopia which has recently received a lot of attention is 25-OH vitamin D levels. Vitamin D3 (Cholecalciferol) is cutaneously synthesized in the skin, which is enhanced on exposure to sunlight. The 25-hydroxy vitamin D [25(OH)D] is an essential hormone that controls calcium and bone metabolism [14]. It also has effects on immune system, cardiovascular system, inflammatory disorders and ocular disorders viz glaucoma, cataract, age-related macular degeneration [15,16].
Materials and Methods
200 young adult subjects aged between 13 to 28 years, participated in this hospital-based case control study carried out in the department of ophthalmology in a tertiary care hospital in north India. Informed consent was obtained from all the patients, along with the consent of their parents/ guardians for patients aged less than 18, including its risks and benefits, as per the adherence to the tenets of declaration of Helsinki.
The study was carried out in three parts, i.e. demographic evaluation and history taking/questionnaire, clinical/ophthalmological evaluation and blood investigation. The participants provided data about age, parental myopia, education status, outdoor activity, and urbanization.
Patients with systemic illness associated with myopia such as diabetes mellitus, glaucoma, marfans syndrome, downs syndrome were excluded from the study. Also, patients with ocular media opacities obscuring fundus evaluation, strabismus, history of refractive surgery, were excluded.
The subjects underwent Best Corrected Visual Acuity (BCVA) testing using snellen’s chart, slit lamp bio microscopy, fundus evaluation using +90D lens. The intraocular pressure was measured using an applanation tonometer. Myopia was graded into pre-myopia, low myopia and high myopia as per international myopia institute grading 2019 [17].
Myopia is a condition in which the spherical equivalent refractive error of an eye is ≤--0.5 D when ocular accommodation is relaxed.
Pre-myopia is refractive state of an eye of <0 D and >--0.50 D in children where a combination of baseline refraction, age, and other quantifiable risk factors provide a sufficient likelihood of the future development of myopia to merit preventative interventions.
Low myopia is a condition in which the spherical equivalent refractive error of an eye is ≤--0.50 and >--6.00 D when ocular accommodation is relaxed.
High myopia is a condition in which the spherical equivalent refractive error of an eye is ≤--6.00 D when ocular accommodation is relaxed.
The diagnosis of myopia was made after post-cycloplegic auto refraction. Tropicamide 1% was instilled into both eyes for a period of 30 min at 10 min interval. Mean Spherical Equivalent (MSE) was used to define myopia [18].
5 ml blood peripheral fasting venous blood samples were collected from each participant in an EDTA vial, which were subsequently sent to department of biochemistry. Samples were analyzed for 25-OH vitamin D levels, using vitros immunoassay analyzer. Serum 25-OH vitamin D concentrations levels were compared and association between myopia and its severity grades was determined. As per the Institute of Medicine (IOM) and the endocrine society, 25-(OH) vitamin D values for classification were as follows [19].
• Vitamin D deficiency is defined as a deaseasonalized serum 25-(OH)D3 concentration below 50 nmol/L.
• Vitamin D insufficiency as serum 25-(OH)D3 concentration of 50 to 74.9 nmol/L.
• Vitamin D deficiency as a 25-(OH) D less than 20 ng/mL (50 nmol/L).
Sufficient/Optimal=>50 Nmol/L
Insufficient=30-50 Nmol/L
Deficient=<30 Nmol/L
• The Institute of Medicine (IOM) and the endocrine society have also defined vitamin D deficiency as a 25-(OH) D less than 20 ng/mL (50 nmol/L) in the year 2010.
• 0-5 ng/ml-Severe Hypovitaminosis[12.5 nmol/l]
• 5-10 ng/ml-Moderate Hypovitaminosis[12.5-25 nmol/l]
• 10-20 ng/ml-Mild Hypovitaminosis[25-50 nmol/l]
Statistical analysis
The statistical analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0 statistical analysis software. The values were represented in number (%) and mean±Standard Deviation (SD). The level of significance “p” was defined being<0.05 as significant, p<0.01 as highly significant and p<0.001 as very highly significant.
Observation and Results
In our study, we compared the data of patients with myopia and those without it. The number of males was found to be higher in both the study groups i.e. 54% in myopes and 59% in non-myopes. This gender based demographic profile was not statistically significant (p=0.117) (Table 1).
| Gender | Total (N=100) |
Myopes (N=100) |
Non-myopes (N=100) |
|||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Male | 113 | 56.5 | 54 | 54 | 59 | 59 |
| Female | 87 | 43.5 | 46 | 46 | 41 | 41 |
| Chi-Square value (c2) | 2.462 | |||||
| Level of significance (p) | 0.117 | |||||
Table 1: Demographic profile of study groups
Age of patients ranged from 13-28 years. Young adults of both the groups were divided in different age groups in years. Maximum myopes were found between the age group of 19-21 years (27%), followed by between 22-24 years (22%) whereas, maximum non myopes were found in age group of 16-18 years (22%). This demographic distribution of data based on age did not show any significance (p=0.561) (Table 2).
| Age in years | Total | Group I myopes (N=100) | Group II non myopes (N=100) | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No | % | |
| 13-15 | 32 | 16 | 14 | 14 | 18 | 18 |
| 16-18 | 39 | 19.5 | 17 | 17 | 22 | 22 |
| 19-21 | 43 | 21.5 | 27 | 27 | 16 | 16 |
| 22-24 | 40 | 20 | 22 | 22 | 18 | 18 |
| 25-27 | 26 | 13 | 12 | 12 | 14 | 14 |
| >28 | 20 | 10 | 8 | 8 | 12 | 12 |
| Chi-Square value (c2) | 0.338 | |||||
| Level of significance (p) | 0.561 | |||||
Table 2: Age distribution of the study groups
It was important to include in the status of education between the myopic and non-myopic patients, to account for adequate sun exposure and time spent indoors. As the study is done in a tertiary hospital, we found the percentage of studying young adults were higher in both groups. 67% myopes and 59% non-myopes were currently undergoing formal education. This relation was statistically insignificant (p=0.028) (Table 3).
| Education Status |
Total(N=200) | Myopes(N=100) | Non- myopes(N=100) | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Studying | 126 | 63 | 67 | 67 | 59 | 59 |
| Not- studying | 74 | 37 | 33 | 33 | 41 | 41 |
| Chi-Square value (c2) | 9.065 | |||||
| Level of significance (p) | 0.028 | |||||
Table 3: Education status of study groups
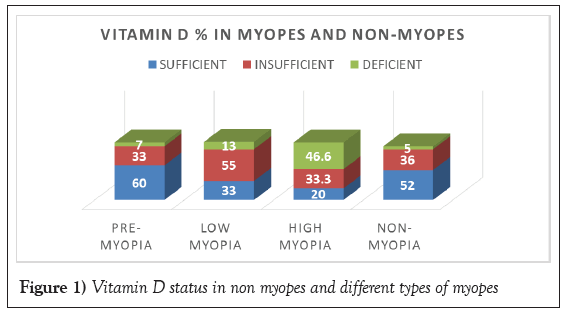
Comparison of the socio-economic status is essential to take into consideration the dietary requirement and supplementation. Based on the housing and demographic data, 52% of myopes and 64% of non-myopes belonged to a rural locality, as compared to 48% myopes and 36% non- myopes belonging to urban setting. This data was statistically significant (p=0.016) (Table 4). Table 5 and Table 6 show the 25-OH vitamin D status with different grading of myopia.
| Locality | Total (N=200) | Myopes (N=100) | Non- myopes (N=100) | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Rural | 116 | 58 | 52 | 52 | 64 | 64 |
| Urban | 84 | 42 | 48 | 48 | 36 | 36 |
| Chi-Square value (c2) | 18.8 | |||||
| Level of significance (p) | 0.016 | |||||
Table 4: Demographic distribution of the study groups
| 25-OH-vitamin D levels (N=200) | Total (N=200) | Pre myopia (N=30) | Low myopia (N=40) | High myopia (N=30) | Non myopia (N=100) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No | % | No | % | No | % | No | % | |
| Sufficient | 89 | 44.5 | 18 | 60% | 13 | 33% | 6 | 20% | 52 | 52 |
| Insufficient | 78 | 39 | 10 | 33% | 22 | 55% | 10 | 33.30% | 36 | 36 |
| Deficient | 33 | 16.5 | 2 | 7% | 5 | 13% | 14 | 46.60% | 12 | 12 |
| Level of significance (p) | ≤ 0.01 | |||||||||
Table 5: Association of vitamin D3 values with different types of myopia
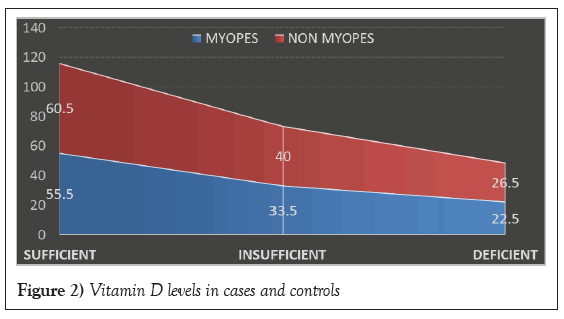
| 25-OH-vitamin D levels (n=200) | Myopia (N=100) | Non myopia (N=100) | ||
|---|---|---|---|---|
| No. | Mean vitamin D value (nmol/l) | No. | Mean vitamin D value (nmol/l) | |
| Sufficien | 37 | 55.5 | 52 | 60.5 |
| Insufficient | d>33.5 | 36 | 40 | |
| Deficient | 21 | 22.5 | 12 | 26.5 |
| p Level of significance (p) | 0.01 | |||
Table 6: Mean vitamin D values with status of sufficiency
Myopia(n=100) was divided into 3 groups pre-myopia(n=30), low-myopia(n=40), high myopia(n=30), non-myopes were 100 in number.
Out of the 3 divisions of myopia, 60% pre-myopes showed sufficient vitamin D levels, 33% had insufficient and the lowest number of deficient was seen with 7%.
In low-myopes, 33% has sufficient vitamin D values highest percent of insufficiency with 55% and 13% had deficient status.
High myopic adults had the highest number of deficient values 46.6%, 33% had insufficient value and lowest number with only 20% sufficient vitamin D values.
On assessing the correlation, the 25-OH vitamin D values with the non- myopic patients, highest number showed sufficiency with 52%, 36% had insufficiency and the lowest number of patients showed deficient status 12%.
This analysis was found to be statistically highly significant (p ≤ 0.01).
Sufficient levels (>50 nmol/l) in myopes was 55.5 nmol/L and 60.5 nmol/L in non-myopes. Insufficient levels (30-50 nmol/l) in myopes were 33.5 nmol/L and 40 nmol/L in non-myopes. Deficient levels (<50 nmol/l) in myopes was 22.5 nmol/L and 26.5 nmol/L in non-myopes. An area pattern graph is used to represent the same (Figures 1 and 2).
Discussion
Myopia is a complex eye disease, in which both genetic and environmental factors contribute to its development [17], predominantly affecting East Asia and Pacific, and South Asia
Myopia is the most common refractive error globally, and it is estimated that there are 1.44 billion people affected, equal to 22.6% of the world’s population. Outdoor activity was recently shown to be another major environmental factor, it is possible that increased outdoor activity may protect against myopia [13]. Possible risk factor for myopia that has received attention is vitamin D, which is cutaneously synthesized during exposure to sunlight. The 25 hydroxy vitamin D [25-(OH)D] is an essential hormone that controls calcium and bone metabolism. [19] It is now clear that 25-(OH) D has diverse effects on the immune system, cardiovascular system, obesity, diabetes, and oncogenesis.
Longitudinal studies have found an association between more time spent in outdoor/sports activity and a reduction in the risk of the onset of juvenile myopia [20]. These results are consistent with several cross-sectional studies that have also reported that myopes spend fewer hours in outdoor/sport activity than other refractive error groups [20-22] in university students.
Progression of myopia is more common in young adults than the school going children. Time spent outdoor was found to be a protective factor for myopia.
However, older age, having myopic parents, higher education level, more time spent reading, nearer reading distance, and higher urbanization level all were risk factors associated with high myopia. [23-24].
Modern techniques have been able to quantify personal environmental light levels using wearable photo detectors [20-21] and physical activity levels using accelerometers [21-22] providing the ability to give objective measures of outdoor exposure times in children. Some recent studies examining the relationship between myopia and outdoor activities have employed a range of different objective devices to estimate outdoor exposure, including wearable light sensors affixed. These wearable sensors provide detailed objective assessments of light exposure patterns.
There is evidence in support of the stereotype; myopic children spend more time in reading and other close work than non-myopic children [23-24].
Time spent outdoors has recently become a variable of interest in myopia research. Like near work, many cross-sectional studies find an association between myopia and time outdoors; myopic children spend less time outdoors than non-myopic children [25-27]. Several theories have been proposed as the physiological basis of a protective effect on myopia of time spent outdoors. Among these has been a better quality retinal image during distance fixation outdoors [28].
Some researchers suggest that a deficiency in 25-(OH)D affects myopia development. One hypothesis posits that lower 25-(OH)D levels induce alterations in intracellular calcium and impaired contraction and relaxation of the ciliary muscles, thereby leading to myopia development [29-30].
The present study was an attempt to understand the relationship between serum vitamin D and myopia in young adults. This assessment was made with a detailed questionnaire and relating the time spent indoors and sun exposure along with status of education. The severity of vitamin D deficiency was directly correlated with severity of myopia. Lower vitamin D levels were found in subjects with higher grade of myopia. The impact of education on vitamin D status has been acknowledged in previous research, although only winter results have been reported [28].
Conclusion
In conclusion, adequate sun exposure, time spent indoors, urbanization and education play a role in progression of myopia. Measurement of vitamin D is one of the many parameters to measure the risk associated with myopia in young adults.
The present study showed that lower serum 25-(OH) vitamin D levels is associated with a high prevalence of myopia in young adults. It also showed that lower vitamin D levels in myopes were associated with higher grade of myopia. These data suggest a role of vitamin D as a risk factor for myopia. Further longitudinal studies need to be carried out for the implementation of role of vitamin D supplementation in young myopes.
Policy Issues
All statements and opinions are the responsibility of the authors. All authors have participated in the research, and have reviewed and agree with the content of the article.
Conflict of Interest
No conflict of interests.
Ethics of Human and Animal Experiments
Informed consent was obtained. Protocol was approved by the institutional review committee.
REFERENCES
- Saw SM, Katz J, Schein OD, et al. Epidemiology of myopia. Epidemiol Rev. 1996;18(2):175-187.
- Flitcroft DI, He M, Jonas JB, et al. Imi-defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Invest Ophthalmol Vis Sci. 2019;60(3):M20-M30.
- Ogawa A, Tanaka M. The relationship between refractive errors and retinal detachment-analysis of 1,166 retinal detachment cases. Jpn J Ophthalmol. 1988;32(3):310-315.
- Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology. 2002;109(4):704-711.
- Mutti OD, Hayes JR, Mitchell GL, et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007;48(6):2510-2519.
- Li YT, Xie MK, Wu J. Association between ocular axial length-related genes and high myopia in a han Chinese population. Ophthalmologica. 2016;235:57-60.
- Saw SM, Carkeet A, Chia KS, et al. Component dependent risk factors for ocular parameters in Singapore Chinese children. Ophthalmology. 2002;109(11):2065-2071.
- Mutti DO, Mitchell GL, Moeschberger ML, et al. Parental myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci. 2002;43(12):3633-3640.
- Lee YY, Lo CT, Sheu SJ, et al. What factors are associated with myopia in young adults? A survey study in Taiwan military conscripts. Invest Ophthalmol Vis Sci. 2013;54(2):1026-1033.
- Guo Y, Liu LJ, Xu L, et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology. 2013;120:277-283.
- Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115(8):1279-1285.
- Feldkaemper M, Schaeffel F. An updated view on the role of dopamine in myopia. Exp Eye Res. 2013;114:106-119.
- Mutti DO, Marks AR. Blood levels of vitamin D in teens and young adults with myopia. Optom Vis Sci. 2011;88(3):377-382.
- Kim SH, Oh MK, Namgung R, et al. Prevalence of 25-hydroxyvitamin D deficiency in Korean adolescents: Association with age, season and parental vitamin D status. Public Health Nutr. 2014;17(1):122-130.
- Brown NA, Hill AR. Cataract: The relation between myopia and cataract morphology. Br J Ophthalmol. 1987;71(6):405-414.
- Mitchell P, Hourihan F, Sandbach J, et al. The relationship between glaucoma and myopia: The Blue Mountains eye study. Ophthalmology. 1999;106(10):2010-2015.
- Flitcroft DI, He M, Jonas JB, et al. Defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Invest Opthalmol Vis Sci. 2019;60(3):M20-M30.
- Luo HD, Gazzard G, Liang Y, et al. Defining myopia using refractive error and uncorrected logMAR visual acuity >0.3 from 1334 Singapore school children ages 7-9 years. Br J Ophthalmol. 2006;90(3):362-366.
- Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington, DC: National Academies Press, 2010.
- Dharani R, Lee CF, Theng ZX, et al. Comparison of measurements of time outdoors and light levels as risk factors for myopia in young Singapore children. Eye. 2012;26:911-918.
- Read SA, Collins MJ, Vincent SJ. Light exposure and physical activity in myopic and emmetropic children. Optom Vis Sci. 2014;91(3):330-341.
- Cooper AR, Page AS, Wheeler BW, et al. Patterns of GPS measured time outdoors after school and objective physical activity in English children: The PEACH project. Int J Behav Nutr Phys Act. 2010;7:31.
- Hepsen IF, Evereklioglu C, Bayramlar H. The effect of reading and near-work on the development of myopia in emmetropic boys: A prospective, controlled, three-year follow-up study. Vision Res. 2001;41(19):2511-2520.
- Mutti DO, Mitchell GL, Moeschberger ML, et al. Parental myopia, near work, school achievement, and children's refractive error. Invest Ophthalmol Vis Sci. 2002;43(12):3633-3640.
- Onal S, Toker E, Akingol Z, et al. Refractive errors of medical students in Turkey: One year follow-up of refraction and biometry. Optom Vis Sci 2007;84(3):175-180.
- Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115(8):1279-1285.
- Dirani M, Tong L, Gazzard G, et al. Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol. 2009;93(8):997-1000.
- Shinkov A, Borissova AM, Dakovska L, et al. Winter 25-hydroxyvitamin D levels in young urban adults are affected by smoking, body mass index and educational level. Eur J Clin Nutr. 2014;69:355-360.
- Annamaneni S, Bindu CH, Reddy KP, et al. Association of vitamin D receptor gene start codon (Fok1) polymorphism with high myopia. Oman J Ophthalmol. 2011;4(2):57-62.
- Lepple-Wienhues A, Stahl F, Willner U, et al. Endothelin-evoked contractions in bovine ciliary muscle and trabecular meshwork: Interaction with calcium, nifedipine and nickel. Curr Eye Res. 1991;10(10):983-989.