COVID-19 and developmental psycho-affective consequences
2 SOD Pronto Soccorso e Medicina d’accettazione e d’urgenza, Azienda Ospedaliero Universitaria delle M, Dipartimento Materno Infantile “G. Salesi”, 60123 Ancona, Italy
3 SOD Anestesia e Rianimazione Pediatrica, Azienda Ospedaliero Universitaria delle Marche,, Dipartimento Materno Infantile “G. Salesi”, 60123 Ancona, Italy
Received: 03-Nov-2022, Manuscript No. PULJCP-22-5534; Editor assigned: 06-Nov-2022, Pre QC No. PULJCP-22-5534 (PQ); Accepted Date: Nov 16, 2022; Reviewed: 10-Nov-2022 QC No. PULJCP-22-5534 (Q); Revised: 14-Nov-2022, Manuscript No. PULJCP-22-5534 (R); Published: 20-Nov-2022, DOI: 10.37532/PULJCP.2023.7(1):9-19
Citation: Oriana P, Margherita P, Alberto V et al. COVID-19 and developmental psycho-affective consequences. J Child Psychol. 2023;7(1):9-19
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
This study examines all the children and adolescents who have sought help, without an organic objective cause, from the Emergency Room in the “G. Salesi” Maternal and Child Health Department at the Azienda Ospedaliero Universitaria delle Marche of Ancona (Italy), between March and December 2020, when COVID-19 spread. Retrospectively, questions were asked about the internal dynamics and the potential increase on developmental mental illnesses in our region (Marche). The total sample, of 765 patients between the ages of 3 years to 15 years of age, was divided into 2 sub-samples for the year 2019 and 2020. During the two lockdowns of 2020, a 13.10% increase in access due to anxiety-depression and a 6.38% increase due to selfharming was found compared to 2019. There was also a 11.79% decrease in access due to externalising symptoms, a 1.86% decrease due to abuse and a 7.84% decrease due to mistreatment. A constellation of somatoform symptoms also emerged, which were probably reflecting the syndromic presentation of COVID-19 in adults. In fact the following increased: abdominal pain (7.26%); breathing difficulties (1.79%); coughing (1.02%); chest pain (0.95%); itching (0.17%).
Keywords
COVID-19, Lockdown, Developmental age, Psychopathology, Affective disorders, Somatoform symptomatology
Introduction
The COVID-19 pandemic has had an impact worldwide, most of all on physical health but also on psycho-affective health, in both adults and children and adolescents.
We have long talked about the risk of contracting the illness and studies on this have found that children have generally contracted COVID-19 in a light, moderate and asymptomatic form. They have only rarely suffered from acute respiratory symptoms, generally among a select population of paediatric patients with often chronic comorbidities [1,2], or when in children a previous infection was detected upon diagnosis of Multisystem Inflammatory Syndrome[3,4].
The psychological effects of the spread of COVID-19 on the population of developmental age have been vitally important, effects which have continued over time, demonstrating the serious nature of their impact.
There is, in fact, a risk that distress and malaise that were previously silent in the interior world of children, pre-adolescents and adolescents have brought about a rapid change to their lives. Among those of developmental age, the phenomenon was so sudden that there was no time to think about what was happening, and therefore no time to psycho-affectively adapt to it. They did not have a chance to make sense of the new way of living, feeling and relating to the outside world, as asked of them so suddenly out of necessity.
There were no longer environmental certainties, including a consolidated school routine that fulfilled the role of mental, physical and affective container and space, where they could interact with their peers. This was in addition to the changes in their home life with their parents, who were mostly deeply concerned and disturbed by such sudden, unprecedented and dangerous external events.
Existing literature has shown the psychological consequences of the pandemic in various countries around the world. It has been revealed that children, pre-adolescents and adolescents experience intense fear for themselves and their family members [5,6], and thus fear the spread of news about how infectious the virus is and the risk of transmitting it accidentally and asymptomatically. A number of affective symptoms became apparent over the months. These included [7,8], fear of what is happening, anxiety-depression, sometimes to the point of clinical depression or full-blown anxiety disorders; anger and feeling of loneliness; mood swings and disorders; post-traumatic stress disorder; over or under eating and sleeping, also accompanied by nightmares; fear of dying and psychosomatic problems. Irritability and carelessness were also noted [6,9,10], which in the developmental stage are the equivalent to behavioural symptoms signalling emotions that have not been fully expressed and processed, and depression.
It must also be taken into account that some children may seem to adapt well, but suffer underlying, below-threshold symptoms, or psychological distress [11].
Over the months, dependency on Internet and mobile phone [12], also developed, which is associated with the fact that less time is dedicated to physical exercise [9]. Some children manifested regressive behaviour, including requests to sleep in their parents’ bed, and becoming much more “clingy”. There has sometimes been a return to bed-wetting [6,10]. There have been self-harming and suicidal thoughts among adolescents, at times becoming actual fullblown attempted suicide [13]. Some studies focused on the effects of lockdown in children and adolescents with an Attention Deficit Hyperactive Disorder (ADHD) diagnosis. Bobo et al. [14], have reported that, in parents’ opinion, most children have manifested a deterioration in their overall emotional well-being, with increased oppositional behaviour and outbursts of emotion, difficulty in sleeping and anxiety. Despite this, a large group of children or adolescents diagnosed with ADHD have conversely shown improvements in their emotions and behaviour, probably due to reduced internal conflict about attending school and social contact, in addition to negative environmental feedback. This went hand in hand with an increase in self-esteem. The study by Gatell-Carbó et al. [15], reported that at the start of the 2020-2021 academic year, 9.8% of Catalan children and adolescents aged between 5 years to 14 years showed probably psychopathological outcomes, including: emotional and behavioural symptoms, sleep disorders and excessive screen use. The group most affected was the 5 years to 8 years age group. Stephenson [16], took the data from a release from the Kaiser Family Foundation (KFF) regarding the United States population, in which young children, black children, adolescents and young LGBTQ may show particular vulnerability to psycho-affective consequences of the pandemic, which are predominantly anxiety and depression. To the contrary, the reduction in a number of Attention Deficit/Hyperactive Disorder medical manifestations was noted, in line with what other authors named above also reported. Panda et al. [8], conducted a broad meta-analysis on psychological studies performed in several countries around the world during the COVID-19 pandemic, which showed how most Asian authors reported a higher prevalence of psychological morbidity compared to countries such as Italy or Spain. Orgilés et al. [9], conducted a study on the Italian and Spanish populations, from which it emerged that parents noticed sizeable changed in their children's emotional state and behaviour, with the onset of symptoms such as: difficulty in concentration, boredom, irritability, feelings of loneliness, agitation and worry. The authors point out that they expect children's behavioural problems to have a negative effect on the family atmosphere and that, on the other hand, parents with high stress levels may apply less effective educational methods to their children, creating a dysfunctional circle. Cusinato et al. [17], conducted a study in Italy on the psychological impact of quarantine rules on children aged 5 years of age to 17 years of age and on their parents, highlighting an increase in hyperactivity levels in children that could be linked to ingravescent negative emotions that resulted in externalising symptoms rather than posttraumatic symptoms. With regard to the parents’ well-being, it appeared that mothers showed more symptoms of anxiety. High levels of stress can affect the parental role and lead to an increase in the risk of abuse and mistreatment [18,19], although there are also protection factors in families that can help the group to manage stress. Shen et al. [20], have stated that the pandemic could continue to have longterm adverse consequences on children and adolescents. Singh et al. [21], emphasised the fact that children aged 3-6 years followed rules more and feared infection, while children and adolescents aged 6 years of age to 18 years of age showed lack of concentration and asked persistent questions. Other studies found high stress levels in the parents of children with special needs, those with atypical behaviour patterns, due to disabilities or chronic medical conditions [22-24]. It was also shown how parental distress can have a negative influence on the ability to manage one's own children in the home, with them adopting suitable disciplinary measures. [25].
The research conducted by Petrocchi et al. [26], discovered that mothers with high distress levels tended to attribute more negative emotions to their children, with consequences on the children’s adaptive abilities [27]. Polizzi et al. [28] showed that, in the period March-May 2020, children with atypical development were perceived by their parents to have more work memory, shifting and attention process problems. However, these children have actual difficulties in performing functions [29].
Overall, a significant correlation was found between parental distress and the parents’ perception of their children’s cognitive skills. In 2022, Werling et al. [30, published a Swiss study on the impact of the COVID-19 pandemic on children’s and adolescents’ mental well-being, as well as that of their families, from the viewpoint of mental health professionals during the first year of the pandemic. Research has shown how that there has been a notable increase in treatment for depression and anxiety, behavioural crises, psychosomatic disorders, attempted suicides and dependencies, such as the excessive use of electronic games.
To the contrary, referrals or spontaneous requests for help regarding Autism Spectrum Disorder or Psychotic Disorders did not undergo substantial changes, and in some cases even decreased slightly.
Within the group of Neuro-development Disorders, there was an increase in the people treated for learning and behavioural disorders. With regard to behavioural dysregulation, anger and aggressiveness in children and adolescents increased during the pandemic, often concurrently with parental stress [31,32].
Treatment for Obsessive-Compulsive Disorder, Eating Disorders and Addictions also increased. The most frequent family problems detected by this study include: parents’ concern about their children's loneliness or isolation, children’s education or educational future, an increase in the use of media due to restrictions on recreational activities and several stressors experienced by mothers.
Again in Switzerland, Berger et al. [33], reported a marked increase in appointments for children and adolescents at mental health emergency services during the pandemic. The same data had already been highlighted in Italy [34], Canada [35 ], and in the United States of America [36]. In their study, Berger et al. [33], compared the frequency of contact with the emergency service KANT (Krisen-Abklärungs-, Notfall-und Triagezentrum), at the Child and Adolescent Psychiatry and Psychotherapy Department of the Zurich’s Psychiatric University Hospital in the period 1st January 2019 to 30 June 2021. The authors also compared patient clinical trends in the period from 1st March to 30th April in the years 2019, 2020 and 2021. The study found that, after an initial drop in requests for help at the start of the first lockdown, use of the emergency service then increased constantly, until it plateaued off at a much higher level than the pre-pandemic period. By comparing the first six months of 2019 and the first six months of 2021, it was possible to see how emergency telephone contacts almost doubled, outpatients assessments increased by 40%, short emergency interventions increased by 230% and admission of children to the adult psychiatric wards more than doubled, due to the number of beds not being able to meet requirements in the child and adolescent psychiatry department.
Overall, this study states a 15% increase in adolescents who reported suicidal idea and a 17% increase in adolescents who reported acts of self-harming.
Werling et al. [30], underlined the fact that the period of adolescence, being a female, the lack of a daily routine and overexposure to information about the pandemic are all risk factors for an increase in psychological problems [37-42].
In particular, the authors stated that for adolescents with previous mental health problems, the advice to stick to strict hygiene measures and to maintain social distancing seems to have sparked or intensified obsessive-compulsive symptoms. They then asked whether the high increase in mental issues was actually caused by the pandemic itself, or whether it is due to the general condition experienced during this period, namely stressful and with a sense of permanent uncertainty in those with pre-existing vulnerabilities and low resilience. On this regard, Correale et al. [21], investigated the psychological impact and the emotional-affective consequences during the pandemic, and discovered a rise of anxiety and depression.
In a study conducted in Argentina, Andrés et al. [31], declared that a large proportion of parents with children between the age of 3 and 18 years of age noticed a change in their children's emotions and behaviours compared to the pre-pandemic period. Particular note was taken of high levels of: aggressiveness-irritability, dependencywithdrawal, carelessness-impulsiveness and anxiety-depression. Changes to sleep and eating patterns, and a drop in positive emotions were also reported. With regard to age groups, children aged 3 year to 8 years seemed to be the ones most affected by an increase in aggressiveness-irritability, dependency-withdrawal and inattention-impulsiveness, while older children, aged 9 years of age to 11 years of age, suffered an increase in anxiety-depression. Older children and adolescents recorded the sharpest decline in positive emotions. The mental health of parents and caregivers was found to be linked to the mental states investigated in patients in the developmental age category. Overall, depression in parents and caregivers was found to be associated with a higher level of dependency-withdrawal in all age groups, but markedly in the 9 years of age to 11 year age group.
In addition to the fact that children in the 9-11 years age group were found to have higher average anxiety-depression values than other age groups, this result also highlights this group's increased vulnerability with regard to the COVID-19 pandemic. Wirkner et al. [42], conducted a systemic revision of a number of longitudinal studies published up to June 2021, in order to investigate the impact of the COVID-19 pandemic on the European population’s mental health, and stated that a young age was considered to be a risk fact for depression, anxiety and feelings of loneliness.
Based on the revision that they conduct, Wirkner et al. [42], speak of the lack of studies on child samples, adding that in most cases, the young age risk factor is linked to the young-adult group, starting from the age of 18 years. All the studies reported here show what has happened and is presumably still happening nationally and internationally as a result of the COVID-19 pandemic.
This paper aims to dwell on children and adolescents who entered the Paediatric Emergency Room (PS) at the Maternal and Child Health Department “G. Salesi” unit at the Azienda Ospedaliero Universitaria delle Marche of Ancona (Italy) without an actual organic triggering cause in the period March-December 2020, coinciding with the spread of COVID-19.
In reference to the Italian context, with specific attention paid to paediatric hospital, it was decided to investigate the psychological and affective consequences in children and adolescents during the pandemic, studying them by comparing them to treatments provided in the same months in 2019.
Materials and Methods
This study arises from the need to understand what has happened in the age group 3 years of age to 15 years of age during the COVID-19 pandemic in a hospital setting, in particular during the two lockdown periods in 2020. A comparison sample was chosen from the same period in the year 2019 as the one affected by the two 2020 lockdowns (March to December). This work is limited to a specifically paediatric reality and is intended as a retrospective epidemiological observation, given the limit that the pandemic itself placed initially on the ability to meet patients several times in order to carry out further psychological evaluations.
The total sample considered is taken from the clinical population at the Paediatric Emergency Room (PS) at the “G. Salesi” Maternal and Child Health Department at the Azienda Ospedaliero Universitaria delle Marche of Ancona in the months March-December 2019 and in the months March-December 2020. The patient catchment basin is the entire Marche (Italy) region. All participants in the total sample were selected from the Paediatric Emergency Room (PS) database, in observance of the current privacy laws, based on a specific inclusion criterion:
• Lack of organic causes triggering symptoms, as confirmed by clinical/instrumental tests.
Patients of a developmental age were therefore selected whose symptoms seemed to have a mainly psychological (somatoform and affective) aetiology.
The following variables are taken into consideration:
• Gender.
• Chronological age on access.
• Type of symptomatology: Internalising; Externalising; Selfharming; Psychosis; Eating Disorders; Mistreatment; Abuse; Mistreatment/Abuse (cases with doubts about the cause of the hospitalisation); Somatoform.
• Type of Somatoform Symptomatology: Asthenia;Headaches; Respiratory difficulties; Dysphagia; Abdominal pain; Chest pain; Lipothymia; Itching; Fainting; Tachycardia; Cough.
• Hospitalisation.
The total sample comprised 765 (N) patients aged 3 years to 15 years, divided into two sub-samples (n):
Patients with access in 2019
n=431 (Average age: 9.8 years; Standard Deviation by age: 3.3).
Patients with access in 2020
n=294 (Average age: 10.8 years; Standard Deviation by age: 3.2)
Each of the two selected sub-samples was in turn divided into two groups based on the “Type of symptomatology” variable:
• Affective Disorders (including the categories: Internalising; Externalising; Self-harming; Psychosis; Eating Disorders; Mistreatment; Abuse; Mistreatment/Abuse);
• Somatoform Symptomatology
The statistical analyses were carried out using the SPSS programme with both parametric and non-parametric tests (Tables 1-3).
TABLE 1: Division of patients with access in 2019 by gender
| Gender (2019) | Variable frequency Gender | Percentage |
|---|---|---|
| F | 221 | 51.28 |
| M | 210 | 48.72 |
| Total (n) | 431 | 100 |
TABLE 2: Division of patients with access in 2020 by gender
| Gender (2020) |
Variable frequency Gender |
Percentage |
|---|---|---|
| F | 171 | 58.16 |
| M | 123 | 41.84 |
| Total (n) | 294 | 100 |
TABLE 3: Type of symptomatology 2019 (n=431)
| Type of symptom (2019) | Frequency of Type of symptomatology (2019) | Percentage |
|---|---|---|
| A | 1 | 0.23 |
| Ab | 3 | 0.7 |
| DA | 18 | 4.18 |
| E | 27 | 6.26 |
| I | 34 | 7.89 |
| M | 8 | 1.86 |
| M/Ab | 2 | 0.46 |
| P | 4 | 0.93 |
| S | 334 | 77.49 |
| Total (n) | 431 | 100 |
The comparison of the variables of interest between the study groups was therefore carried out by:
• The Student T test for the sample distribution of the difference between the two averages.
• The Mann-Whitney test for the positional parameters on the two independent samples.
• The Chi-squared functional test to check the adaptation between the theoretical distribution and the expected distribution of frequencies.
• The precise Fisher test for very low expected frequencies or very small samples.
A significance level of α = 0.05 or α = 0.01 has been set
The objectives that the study set are as follows:
• A comparison of data regarding entries to the Emergency Room (PS) of the “G. Salesi” Maternal and Child Health Unit at the Azienda Ospedaliero Universitaria delle Marche of Ancona in the months March-December 2019 and 2020, considering symptoms that were presumably somatoform or affective.
• Inclusion criterion for the study sample: lack of organic causes triggering the symptoms as confirmed by clinical/instrumental tests.
• Study of the variable. “Age” of the patients accessing the Emergency Room (sample average; standard deviation of the sample).
• Study of the trend, and therefore potential increase/decrease, of “Affective Disorders” and “Somatoform Symptomatology” in total number of entries due to presumably psycho-affective symptoms in the abovestated periods in the years 2019 and 2020.
• Further examination of the study hypothesis regarding a psychopathological somatoform trajectory including symptomatic categories such as: “Headache”, “Asthenia”, “Breathing Difficulties”, “Dysphagia”, “Abdominal Pain”, “Chest Pain”, “Lipothymia”, “Fainting”, “Tachycardia”, “Cough”, “Itching”, that may be associated with each other and combine in a constellation of symptoms.
Result
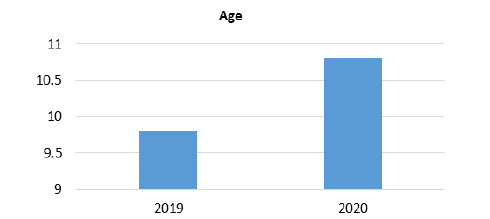
Data analysis first of all concerned the “Age” variable, compared to which comparison with the T test between the two 2019 and 2020 sub-samples was found to be statistically significant: t(645,746) = - 4.21, p< 0,01.
In this sense, there is an average rise of one year of age in patients who came to the Emergency Room once or more times in the year 2020 (Average age: 10.8 years) compared to those patients attending the Paediatric PS during the previous year (Average age: 9.8 years) (Figure 1).
On a descriptive level, in the 2020 sub-sample, there is a 16.32% difference between female and male entrances, the former being respectively greater than the latter.
The “Type of symptomatology” presented by children and adolescents was significantly different to the Pearson Chi-squared test between 2019 and 2020: χ 2 = 17.07; df = 8; p< 0.05.
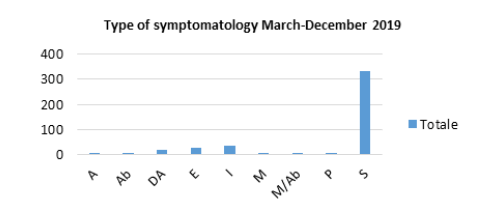
Below are the total patient symptoms, as frequency, in the months March-December 2019 and March-December 2020 respectively.
Legend to type of symptom: Self-harming=A; Abuse=Ab; Eating Disorders=DA; Externalising=E; Internalising=I; Mistreatment/Abuse=M/Ab (cases in which there was doubt as to the cause of hospital access); Psychosis=P; Somatoform=S.
The categories A, Ab, DA, E, I, M, M/Ab are included in the subgroup “Affective Disorders”
The sub-group “Somatoform Symptomatology” includes the following sub-categories: Asthenia=As; Headache=Cef; Breathing Difficulties=DRes; Dysphagia=Dis; Abdominal Pain=DAd; Chest Pain=DTor; Lipothymia=L; Itching=Pr; Fainting=Sin; Tachycardia=Ta; Cough=Tos
Table 3 and Figure 2 show the symptoms that emerged overall during visits that had a mainly psychological aetiology during the months March-December 2019, specifying the categories included in “Affective Disorders” (A, Ab, DA, E, I, M, M/Ab, P, S) and “Somatoform Symptomatology” (S).
The two sub-groups “Affective Disorders” and “Somatoform Symptomatology” were then examined.
With regard to “Affective Disorders”, Table 4 shows the frequencies and percentages with which this symptomatology presented it-self in males and females in the year 2019.
TABLE 4: Affective disorders in the year 2019 divided by gender
| Gender | Variable frequency Gender | Percentage |
|---|---|---|
| F | 65 | 67.01 |
| M | 32 | 32.99 |
| Total | 97 | 100 |
Below is an illustration of how the categories included in this subgroup appeared in patients who were treated in the same year (Table 5)
TABLE 5: Categories of affective disorders manifested in 2019
| Affective Disorders (2019) | Frequency of Affective Disorders (2019) | Percentage |
|---|---|---|
| A | 1 | 1.03 |
| Ab | 3 | 3.09 |
| DA | 18 | 18.56 |
| E | 27 | 27.84 |
| I | 34 | 35.05 |
| M | 8 | 8.25 |
| M/Ab | 2 | 2.06 |
| P | 4 | 4.12 |
| Total | 97 | 100 |
Affective Disorders 2019 (Average age=12.3 years)
Based on the same criteria, and again in reference to 2019, the sub-group “Somatoform Symptomatology” (Table 6).
TABLE 6: Somatoform Symptomatology in 2019 divided by gender
| Gender | Variable frequency Gender | Percentage |
|---|---|---|
| F | 156 | 46.71 |
| M | 178 | 53.29 |
| Total | 334 | 100 |
Somatoform Symptomatology 2019 (Average age=9.1 years)
The data regarding “Somatoform Symptomatology” are shown in detail in Table 7, with the addition of the "Associated" (Assoc) category, including cases in which several somatoform symptoms presented themselves together in the same patient .
TABLE 7: Categories of Somatoform Symptoms occurring in 2019
| Somatoform Symptomatology (2019) | Frequency of Somatoform Symptomatology (2019) | Percentage |
|---|---|---|
| As | 7 | 2.1 |
| Assoc | 8 | 2.4 |
| Cef | 83 | 24.85 |
| DAd | 131 | 39.22 |
| DRes | 5 | 1.5 |
| DTor | 47 | 14.07 |
| L | 19 | 5.69 |
| Pr | 1 | 0.3 |
| Sin | 6 | 1.8 |
| Ta | 21 | 6.29 |
| Tos | 6 | 1.8 |
| Total | 334 | 100 |
Legend to type of symptoms: Self-harming=A; Abuse=Ab; Eating Disorders=DA; Externalising=E; Internalising=I; Mistreatment=M; Psychosis=P; Somatoform=S
The categories A, Ab, DA, E, I, M are included in the sub-group “Affective Disorders”
The sub-group “Somatoform Symptomatology” includes the following sub-categories: Asthenia=As; Headache=Cef; Breathing Difficulties=DRes; Dysphagia=Dis; Abdominal Pain=DAd; Chest Pain=DTor; Lipothymia=L; Itching=Pr; Fainting=Sin; Tachycardia=Ta; Cough=Tos.
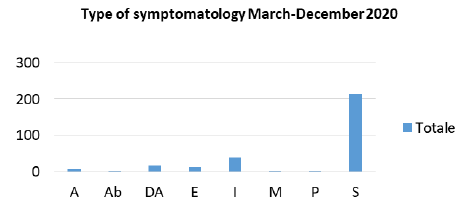
As already conducted for entries to the Paediatric Emergency Room (PS) in the months March-December 2019, at this point the two sub-groups “Affective Disorders” and “Somatoform Symptomatology” for the year 2020 were investigated (Figure 3 and (Table 8).
TABLE 8:Type of symptomatology 2020 (n=294)
| Type of Symptomatology (2020) | Frequency of Type of Symptomatology (2020) | Percentage |
|---|---|---|
| A | 6 | 2.04 |
| Ab | 1 | 0.034 |
| DA | 17 | 5.78 |
| E | 13 | 4.42 |
| I | 39 | 13.27 |
| M | 2 | 0.68 |
| P | 3 | 1.02 |
| S | 213 | 72.45 |
| Total (n) | 294 | 100 |
Table 9 shows the frequencies and percentages of “Affective Disorders” symptoms that occurred in males and females in 2020. Below we see how the categories contained in this sub-group were found in patients who accessed the PS in 2020 (Table 10).
TABLE 9: Affective disorders in 2020 divided by gender
| Gender | Variable frequency Gender | Percentage |
|---|---|---|
| F | 57 | 70.37 |
| M | 24 | 29.63 |
| Total | 81 | 100 |
TABLE 10: Categories of affective disorders manifested in 2020
| Affective Disorders (2020) | Frequency of Affective Disorders (2020) | Percentage |
|---|---|---|
| A | 6 | 7.41 |
| Ab | 1 | 1.23 |
| DA | 17 | 20.99 |
| E | 13 | 16.05 |
| I | 39 | 48.15 |
| M | 2 | 2.47 |
| P | 3 | 3.7 |
| Total | 81 | 100 |
The sub-group “Somatoform Symptomatology” is described according to the same criteria and again in reference to 2020 (Tables 11 and 12).
TABLE 11: Somatoform symptomatology in 2020 divided by gender
| Gender | Variable frequency Gender | Percentage |
|---|---|---|
| F | 114 | 53.52 |
| M | 99 | 46.48 |
| Total | 213 | 100 |
TABLE 12: Categories of somatoform symptoms occurring in 2020
| Somatoform Symptomatology (2020) | Frequency of Somatoform Symptomatology (2020) | Percentage |
|---|---|---|
| As | 4 | 1.88 |
| Assoc | 3 | 1.41 |
| Cef | 26 | 12.21 |
| DAd | 99 | 46.48 |
| Dis | 9 | 4.23 |
| DRes | 7 | 3.29 |
| DTor | 32 | 15.02 |
| L | 7 | 3.29 |
| Pr | 1 | 0.47 |
| Sin | 6 | 2.82 |
| Ta | 13 | 6.1 |
| Tos | 6 | 2.82 |
| Total | 213 | 100 |
Somatoform Symptomatology 2020 (Average age=9.8 years)
The data regarding “Somatoform Symptomatology” are shown in detail in Table 12, with the addition of the "Associated" (Assoc) category, including cases in which several somatoform symptoms presented themselves together in the same patient.
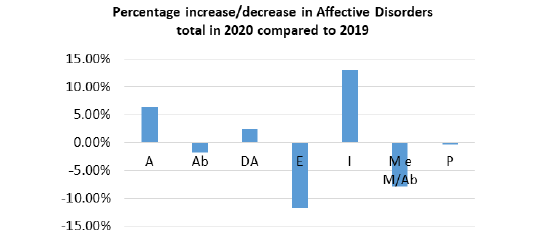
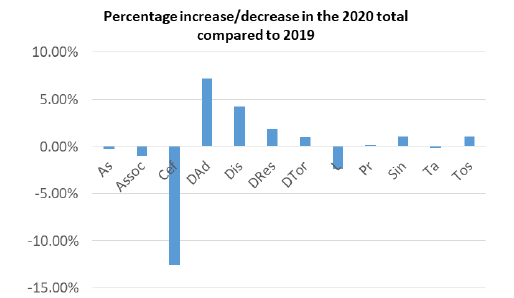
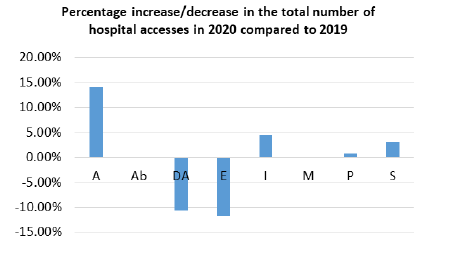
The data showing the percentage increase or decrease in 2020, compared to the 2019 total of the symptoms triggering entry to the Paediatric PS, are therefore shown for both the sub-group “Affective Disorders” and for the sub-group “Somatoform Symptomatology”. Please note that the relative differences between the “Type of symptomatology” in 2019 and in 2020, and therefore referring to the sub-groups “Affective Disorders” and “Somatoform Symptomatology” considered overall, were found to be significant for the Pearson Chisquared test (χ²=17.07; df=8; p< 0.05). The differences concerning the various types of “Somatoform Symptomatology”, intended as separate manifestations, are also significant (χ²=33.71; df=12; p< 0.01).
Comparison of the sub-group Affective Disorders in the years 2019- 2020
Table 13 and Figure 4 show the high percentage increase (13.10%) in internalising disorders, and therefore mainly regarding anxiety and depression, compared to an 11.79% decrease in accesses due to externalising symptomatology, characterised by behavioural disorders and psychomotor agitation crises that are not caused by delirium episodes or substance use/abuse/abstinence. Self-harming shows an increase of 6.38%.
TABLE 13: Percentage increase/decrease in affective disorders in the 2020 total compared to 2019
| Affective Disorders | Percentage increase/decrease in the 2020 total compared to 2019 |
|---|---|
| A | 6.38 |
| Ab | -1.86 |
| DA | 2.43 |
| E | -11.79 |
| I | 13.1 |
| M and M/Ab | -7.84 |
| P | -0.42 |
Accesses due to Eating and Nutrition Disorders have increased by 2.43%, while those due to abuse or mistreatment have fallen by 1.86% and 7.84% respectively [13].
Comparison of sub-group Somatoform Symptomatology in the years 2019-2020
Table 14 and Figure 5 unexpectedly highlight a large overall increase of a psychic symptomatological constellation with somatoform expression; to this regard, during the 2020 lockdown due to COVID19 there probably was a situation of somatoform symptomatology in the children who visited the PS. This symptomatology was similar to COVID-19 illness in adults.
TABLE 14: Percentage increase/decrease in Somatoform Symptomatology in the 2020 total compared to 2019
| Somatoform Symptomatology | Percentage increase/decrease in the 2020 total compared to 2019 |
|---|---|
| As | -0.22 |
| Assoc | -0.99 |
| Cef | -12.64 |
| DAd | 7.26 |
| Dis | 4.23 |
| DRes | 1.79 |
| DTor | 0.95 |
| L | -2.40 |
| Pr | 0.17 |
| Sin | 1.02 |
| Ta | -0.19 |
| Tos | 1.02 |
Increases were found in: abdominal pain (7.26%); breathing difficulty (1.79%); cough (1.02%); chest pain (0.95%), itching (0.17%). There was an increase of 4.23% in visits due to dysphagia and a 1.02% increase in fainting.
To the contrary, entries due to headache without an organic cause decreased by 12.54% on 2019, as visits due to lipothymia decreased by 2.40%.
The difference between 2019 and 2020 is also significant for the Pearson Chi-squared test for the variable “Hospitalisation” (χ²=7.72; df=1; p< 0.01).
Compared to the latter, frequency data are shown in Table 15 and the total percentage of hospitalisations in the months of MarchDecember of the two compared sub-samples.
TABLE 15: Comparison of the frequency of hospitalisation variables
| Hospitalisation (2019) | Frequency of Hospitalisation variable (2019) | Percentage |
|---|---|---|
| NO | 407 | 94.43 |
| YES | 24 | 5.57 |
| Total | 431 | 100 |
| Hospitalisation (2020) | Frequency of Hospitalisation variable (2020) | Percentage |
| NO | 261 | 88.78 |
| YES | 33 | 11.22 |
| Total | 294 | 100 |
Overall in 2020, there was a 5.65% increase in hospitalisations in the various specialised departments on the total accesses due to symptoms that have a presumably psychological aetiology (somatoform and affective) compared to the year 2019.
Table 16 and Figure 6 below show the increase or decrease in detail of hospitalisations in each of the categories belonging to the “Affective Disorders” group and regarding “Somatoform Symptomatology”.
TABLE 16: Percentage increase/decrease in hospitalisations in the 2020 total compared to 2019
| Reason for Hospitalisation | Percentage increase/decrease in the 2020 total compared to 2019 |
|---|---|
| A | 14.01 |
| Ab | 0 |
| DA | -10.61 |
| E | -11.74 |
| I | 4.54 |
| M | 0 |
| P | 0.76 |
| S | 3.03 |
This study therefore highlights the fact that in 2020, there was a 14.01% increase in hospitalisations due to self-harming and a 4.54% increase due to internalising disorders compared with an 11.74% increase in hospitalisations due to externalising disorders.
Admissions due to Eating and Nutrition Disorders [13], diagnosed as such further to a first visit to the Emergency Room, fell by 10.64%. Hospitalisations due to Psychotic disorders increased by 0.76%, considering the fact that these included two patients with the onset of acute psychotic episodes and a case of the return of an acute disorder that had already been diagnosed [13].
Somatoform disorders saw an increase of 3.03%.
Discussion
This epidemiological study found as follows:
• Regarding the 1st objective (par. 2), during the two lockdowns in 2020, in the accesses to the Paediatric PS there was a transformation of psycho-affective symptoms during the developmental age range. Specifically, the data will be discussed in reference to the 3rd objective.
• In the 2nd objective, study of the “Age” variable in patients accessing the Paediatric PS showed an average increase of one year in those who visited once or more times in 2020 (Average age: 10.8 years) compared to patients in 2019 (Average age: 9.8 years). This result may indicate that the latency age has been affected in socioenvironmental aspects that specifically allow children to experiment their development according to what is required by their age. In this sense, with COVID-19, there was a loss of the possibility to gain experiences in contexts other than the family environment, such as school, peer groups and extra-scholastic activities. The potential psychopathological psycho-affective outcomes may be associated with this.
• With regard to the 3rd objective, 2020 saw a large percentage increase (13.10%) in hospital accesses due to internalising disorders and thus mainly anxiety-depression, while there was an 11.79% fall in entries due to externalising symptomatology, characterised by behavioural disorders and psychomotor agitation crises that are not due to delirium or substance use/abuse/abstinence. With regard to externalising disorders, we can hypothesise thatthe greater presence of adults provided greater containment on behaviour, also due to the fact more time was spent with their children. However, the increase in internalising anxiety-depression disorders may be an indication of the mobility of emotions in children and adolescents that have changed from behavioural manifestations to intrapsychic manifestations, also due to circulating family concerns. There should be an investigation of whether there are psychopathological nuclei that react to environmental and family situations that may justify the transformation of affective symptoms. This hypothesis must be studied further in subsequent clinical studies.
• The decrease of visits for abuse and mistreatment in 2020, 1.86% and 7.84% respectively, creates attention and interest. This data must be understood and studied further, as it is totally new and contrary to what we would have expected based on our current knowledge from existing literature.
• Regarding visits due to Nutrition and Eating Disorders, in 2020 there was a 2.43% increase, although investigation is required to know whether this was due to new onsets or relapses, in order to attribute a clearer psychopathological meaning to it. This, however, falls outside the objectives of this paper.
• In the 4th objective, a large overall increase in a constellation of psychic symptoms with somatoform expression was found among the children and adolescents entering the Paediatric PS during the two COVID-19 lockdown in 2020 (months March-December), with the likelihood of that mirroring the symptoms of COVID-19 itself in adults.
The following symptoms showed an increase: abdominal pain (7.26%); breathing difficulty (1.79%); cough (1.02%); chest pain (0.95%); itching (0.17%).
In relation to the specific COVID-19 pandemic, this result appears to be especially significant for clinical/descriptive purposes. It would, in fact, appear to differ from current international literature and be of a potential psychopathological nature. The evolution of this data should be further investigated in a future perspective, asking questions about the internal dynamics activated in children and adolescents by mass media information and social networks that seem to have contributed to building internal experiences circulating in this historical period.
Conclusion
This descriptive and epidemiological study examines all children and adolescents who entering the Emergency Room of the “G. Salesi” Maternal and Child Health Department at the Azienda Ospedaliero Universitaria delle Marche of Ancona (Italy), between March and December 2020, at the time of the diffusion of COVID-19. The sample was compared with a corresponding sample in 2019. The internal dynamics and potential increase in psychopathologies in children, pre-adolescents and adolescents in our region were examined. The total sample of 765 patients aged 3 years to 15 years was then divided into two sub-samples with reference to the years 2019 and 2020.
Results showed an increase in anxiety-depression disorders and selfharming among the developmental age range which is in line with existing literature. A decrease in externalising disorders was also found in the study sample during the COVID-19 pandemic. With regard to this last data, we can hypothesize that the greater presence of adults in the family provided a higher containment on behaviour and more listening to needs, also due to the fact parents spent more time with their children. The increase in internalising anxiety-depression disorders, which occurred at the same time, may be an indication of the mobility of developmental-age emotions, changing from behavioural manifestations to intrapsychic manifestations, also further to concerns circulating in the family. There should be an investigation of whether there are psychopathological nuclei that react to environmental and family situation that may justify the transformation of affective symptoms. This hypothesis must be studied further in subsequent clinical studies.
Two results that have not been described by the literature have characterised this study in particular.
These concern:
• The fall in visits to the Paediatric Emergency Room due to mistreatment and/or abuse;
• A constellation of somatoform symptoms similar to COVID-19 illness in adults. In relation to the COVID-19 pandemic, this result appears to be especially significant at a clinical/descriptive level, in accordance with psychopathological criteria in the developmental age.
What we discovered brings us to ask some questions:
• In psychological clinical practice, what expression could the emerging data take on?
• With regard to the COVID-19 somatoform constellation highlighted, could its onset have been influenced by the concern, fears, confusion and bewilderment circulating among adults?
• How much could the somatoform symptomatology itself have been further affected by the continuous amount of information from mass media and social networks?
These results should be observed while also taking into consideration the intrapsychic organisation that is still evolving in children and adolescents. Their emotive regulation and thought largely depend on the adult’s psycho-affective stability, according to their age range.
For more information and in order to search for answers to the questions asked, it would be necessary to continue with clinical investigations and be able to build a network of national and international paediatric centres in order form them to cooperate.
References
- Parri N, Magistà AM, Marchetti F, et al. Characteristic of COVID-19 infection in pediatric patients: early findings from two Italian Pediatric Research Networks. Eur J Pediatr. 2020;179(8):1315-23.
- Parri N, Lenge M, Cantoni B, et al. COVID-19 in 17 Italian Pediatric Emergency Departments. Pediatrics. 2020;146(6):e20201235.
- Bu F, Steptoe A, Fancourt D. Loneliness during a strict lockdown: Trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc Sci Med. 2020;265.
- Fang Y, Aravamudan VM, Sridharan GK, et al. Kawasaki like illness due to COVID-19: a review of the literature. J Infect Dev Ctries. 2021;15(5):630-8.
- D’Annunzio G, Maffeis C, Cherubini V, et al. Caring for children and adolescents with type 1 diabetes mellitus: Italian Society for Pediatric Endocrinology and Diabetology (ISPED) statements during COVID-19 pandemia. Diabetes Res Clin Pract. 2020;168:108372.
- Jiao WY, Wang LN, Liu J, et al. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J Pediatr. 2020;221:264-6.
- Brunelli A, Silvestrini G, Palestini L, et al. Impact of the lockdown on children and families: a survey of family pediatricians within a community. Recenti Prog Med. 2021;112(3):207-15.
[Google Scholar] [CrossRef]
- Panda PK, Gupta J, Chowdhury SR, et al. Psychological and Behavioral Impact of Lockdown and Quarantine Measures for COVID-19 Pandemic on Children, Adolescents and Caregivers: A Systematic Review and Meta-Analysis. J trop pediatr. 2021;67(1):fmaa122.
- Orgilés M, Morales A, Delvecchio E, et al. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. Front Psychol. 2020;11:2986.
- Pisano L, Galimi D, Cerniglia L. A qualitative report on exploratory data on the possible emotional/behavioral correlates of Covid-19 lockdown in, 4-10 years children in Italy. PsyArXiv. 2020.
[Google Scholar] [CrossRef]
- Ammaniti M, Cerniglia L. I passi della crescita. La sicurezza degli affetti e dei legami. 2019. [Google Scholar] [CrossRef]
- Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect Disord. 2020;275:112-8.
- American Psychiatric Association. Manuale diagnostic e statistic dei disturbi mentali. Quinta Edizione (DSM-5). Raffaello Cortina Ed. 2014. [Google Scholar] [CrossRef]
- Bobo E, Lin L, Acquaviva E, et al. How do children and adolescents with Attention Deficit Hyperactivity Disorder (ADHD) experience lockdown during the COVID-19 outbreak? Encephale. 2020;46(3):S85-S92.
[Google Scholar] [CrossRef]
- Correale C. Depressive Anxiety Symptoms in hospitalized children with chronic illness during the first Italian COVID-19 Lockdown. Children. 2022;9(8):1156.
- Stephenson J. Children and Teens Struggling with Mental Health During COVID-19 Pandemic. JAMA Health Forum. 2021;2(6):e211701.
- Cusinato M, Iannattone S, Spoto A, et al. Stress, Resilience, and Well-Being in Italian Children and Their Parents during the COVID-19 Pandemic. Int J Environ Res Public Health. 2020;17(22):8297.
- Clément ME, Bérubé A, Chamberland C. Prevalence and risk factors of child neglect in the general population. Public Health. 2016;138:86-92.
- Stith SM, Liu T, Davies LC, et al. Risk factors in child maltreatment: A meta-analytic review of the literature. Aggress Violent Behav. 2009;14:13-29.
- Shen K, Yang Y, Wang T, et al. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: Experts’ consensus statement. World J Pediatr. 2020;16(3):223-31.
- Singh S, Roy D, Sinha K, et al. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020;293:113429.
- Estes A, Olson E, Sullivan K, et al. Parenting-related distress and psychological didistress in mothers of toddlers with autism spectrum disorders. Brain Dev. 2013;35(2):133-8.
- Hayes SA, Watson SL. The impact of parenting distress: A meta-analysis of studies comparing the experience of parenting distress in parents of children with and without autism spectrum disorder. J Autism Dev Disord. 2013;43(3):629-42.
- Theule J, Wiener J, Tannock R, et al. Parenting distress in families of children with ADHD: A meta-analysis. J Emot Behav Disord. 2013;21:3-17.
- Cusinato M, Iannattone S, Spoto A, et al. Stress, Resilience, and Well-Being in Italian Children and Their Parents during the COVID-19 Pandemic. Int J Environ Res Public Health. 2020;17(22):8297.
- Petrocchi S, Levante A, Bianco F, et al. Maternal Didistress/Coping and Children’s Adaptive Behaviors during the COVID-19 Lockdown: Mediation Through Children’s Emotional Experience. Front Public Health. 2020;8:587833.
- Haleemunnissa S, Didel S, Swami MK, et al. Children and COVID-19: Understanding impact on the growth trajectory of an evolving generation. Child Youth Serv Rev. 2021;120:105754.
- Polizzi C, Burgio S, Lavanco G, et al. Parental Distress and Perception of Children's Executive Functioning after the First COVID-19 Lockdown in Italy. J Clin Med. 2021;10(18):4170.
- Lindström C, Aman J, Norberg AL. Parental burnout in relation to sociodemographic, psychosocial and personality factors as well as disease duration and glycaemic control in children with Type 1 diabetes mellitus. Acta Paediatr. 2011;100:1011-7.
- Werling AM, Walitza S, Eliez S, et al. Impact of the COVID-19 pandemic on mental health and family situation of clinically referred children and adolescents in Switzerland: results of a survey among mental health care professionals after 1 year of COVID-19. J Neural Transm. 2022;129(5-6):675-88.
- Andres ML, Galli JI, del Valle M, et al. Parental perceptions of child and adolescent mental health during the COVID-19 pandemic in Argentina. Child Youth Care Forum. 2022.
- Montirosso R, Mascheroni E, Guida E, et al. Stress symptoms and resilience factors in children with neurodevelopmental disabilities and their parents during the COVID-19 pandemic. Health Psychol. 2021;40(7):428-38.
- Berger G, Haberling I, Lustenberger A, et al. The mental distress of our youth in the context of the corona pandemic. Swiss Med Wkly. 2022;152:30142.
- Vicari S, Pontillo M. Developmental psychopathology in the COVID-19 period. COVID-19 pandemic impact on children and adolescents’ mental health. Psychiatr Danub. 2021;33(11):33-5.
[Google Scholar] [CrossRef]
- Chadi N, Spinoso-Di Piano C, Osmanlliu E, et al. Mental health-related emergency department visits in adolescents before and during the COVID-19 pandemic: a multicentric retrospective study. J Adolesc Health. 2021;69(5):847-50.
- Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health–related emergency department visits among children aged<18 years during the COVID-19 pandemic—United States, January 1-October 17, 2020. Morb Mortal Wkly Rep. 2020;69(45):1675.
- Bhatia R. Effects of the COVID-19 pandemic on child and adolescent mental health. Curr Opin Psychiatry. 2020;33(6):568-70.
- Kazi F, Mushtaq A. Adolescents navigating the COVID-19 pandemic. Lancet Child Adolesc Health. 2021;5(10):692.
- Mohler-Kuo M, Dzemaili S, Foster S, et al. Stress and mental health among children/adolescents, their parents, and young adults during the first COVID-19 lockdown in Switzerland. Int J Environ Res Public Health. 2021;18(9):4668.
- Qin Z, Shi L, Xue Y, et al. Prevalence and risk factors associated with self-reported psychological distress among children and adolescents during the COVID-19 pandemic in China. JAMA Netw Open. 2021;4(1):e2035487.
- Wang G, Zhang Y, Zhao J. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945-7.
- Wirkner J, Christiansen H, Knaevelsrud C, et al. Mental health in times of the covid-19 pandemic. Eur Psychol. 2022;26:310-22.