Crohn’s disease with pulmonary involvement: A rare localization
2 Department of Medicine A, Louis Pasteur Hospital, Colmar, France, Email: Laurianne90@yahoo.com
Received: 05-Aug-2018 Accepted Date: Sep 10, 2018; Published: 25-Sep-2018
Citation: Kpossou AR, Plastaras L, Samuel-Dodo LR, et al. CrohnĂƒÂ¢Ă‚â‚¬Ă‚â„¢s disease with pulmonary involvement: A rare localization. J Hepato Gastroenterol. 2018;2(2):40-3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
INTRODUCTION: Although joint, skin and ophthalmological involvement remain the most reported extra-digestive manifestations of Crohn’s disease, pulmonary localization is rare. We report a case of Crohn’s disease with early pulmonary involvement. CASE REPORT: This was a 24-year-old smoking patient who had consulted for multiple chest pains in a recent Crohn’s disease context. A chest CT scan showed pulmonary hypodense, lobulated nodular structures in the left and right lower lobes. The left lung nodule biopsied, revealed subacute inflammatory changes with giant cell granuloma and necrosis foci related to the Crohn’s disease after excluding tuberculosis and sarcoidosis. After initiation of anti-TNFα (adalimumab), the evolution was favorable with regression of clinical symptoms and lung lesions but at the cost of a severe psoriasis outbreak that required a change in treatment with ustekimab. CONCLUSION: The hypothesis of pulmonay localization should be mentioned in case of pulmonary symptoms from a patient followed for Crohn’s disease.
Keywords
Crohn’s disease; Pulmonary involvement; Anti-TNF α ; Ustekimab; Psoriasis
Introduction
Crohn’s disease (CD) is a chronic inflammatory disease that usually affects the gastrointestinal tract and which etiology remains unknown [1]. The extradigestive attacks of this inflammatory bowel disease are mainly represented by articular, dermatological and ophthalmological manifestations [2,3]. Respiratory disease is rare and poorly described with an estimated prevalence of 0.2% [4]. Among these respiratory disorders, the upper respiratory tract is classically separated from the parenchymal pulmonary lesions [5]. These pulmonary disorders appear several years after the onset of the digestive disease and evolve in parallel with the degree of activity of the intestinal disease [1,6]. We report a case of early nodular pulmonary involvement concomitant with gastrointestinal involvement during CD. This case sensitizes the clinician to have in mind, the possibility of early pulmonary involvement in a patient followed for a CD and who consults for common respiratory symptoms. These attacks are an expression of the progressive nature of the disease and require more aggressive therapy to induce remission.
Case Presentation and Observations
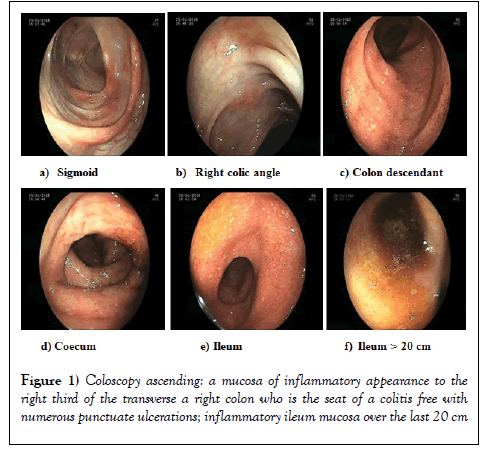
A 24-year-old female patient with known smoking status (5 cigarettes per day for 3 years, -1 package-year) presented an inaugural episode of acute left anterior uveitis that favorably evolved under treatment with local corticosteroid (dexamethasone eye drops) mydriatic eye drops (Atropine eye drops). It followed two months later, articular ankle pain and rectorragia that gave way to abdominal pain with diarrheal tendency (20 episodes/ day). On examination of the general condition, the patient weighed 63 kg for a height of 167 cm (BMI: 22.5 kg/m2). On physical examination, the abdomen was painful soft in the right iliac fossa without defense, without palpable mass, without hepatosplenomegaly. The examination of the anal margin and digital rectal examination were without particularity (absence of fistula or ano-perineal fissure). The ganglionic areas were free, the pleuropulmonary, neurological and cardiovascular examinations were without particularity. In biology, there was a biological inflammatory syndrome with a C-reactive protein at 23 mg/l and an acceleration of the speed; a blood count and a normal liver test. The combination of uveitis, digestive and articular symptoms and inflammatory syndrome suggested the hypothesis of a chronic inflammatory bowel disease. Gastroscopy did not show any lesions, and duodenal biopsies showed no villous atrophy. The colonoscopy showed a normal-looking mucosa to the right third of the transverse; the right colon was the site of frank colitis with numerous punctate ulcerations; a very fragile inflammatory mucosa with edema of the wall and an inflammatory state of the ileal mucosa over the last 20 centimeters (CDEIS = 7) (Figure 1).
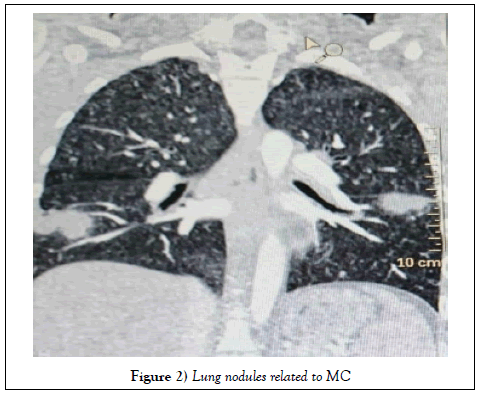
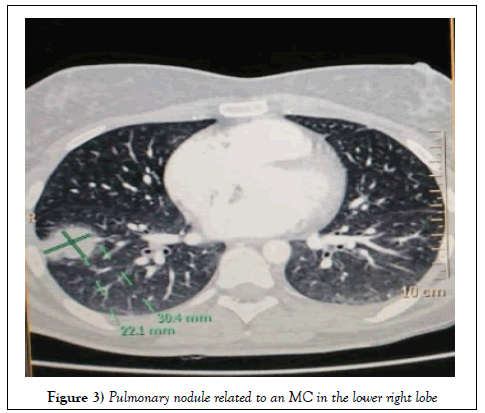
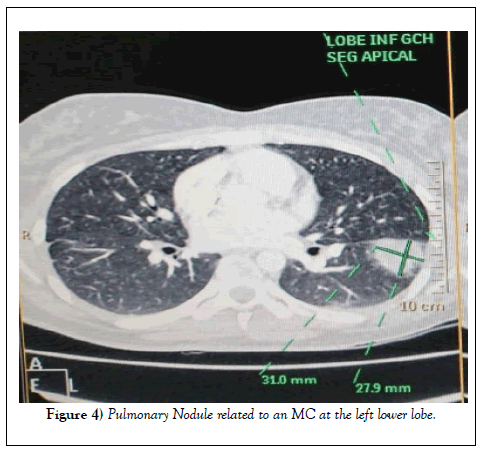
The biopsies showed moderate chronic inflammatory status with presence of epithelioid granulomas compatible with active and severe Crohn’s disease (score of 25 according to the Harvey-Bradshaw index (HBI)). The patient was put on initial treatment with corticosteroid and azathioprine. The evolution was marked 3 months later by a chart of disabling left bas-thoracic pains without notion of cough or other associated respiratory sign. A chest CT scan then performed noted lobed hypodense nodular structures in the left and right lower lobes (Figures 2 - 4).
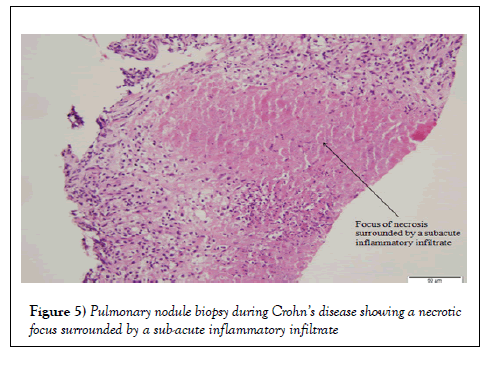
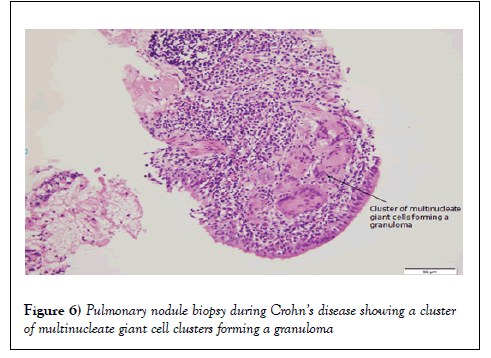
Without mediastinal lymphadenopathy, left-wing biospace lesion revealed subacute inflammatory changes with giant cell epithelioid granulomas and foci of necrosis (Figures 5 and 6).
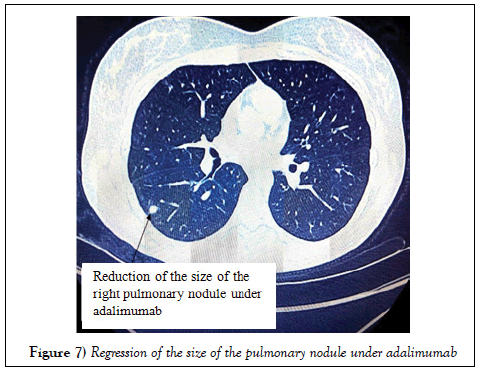
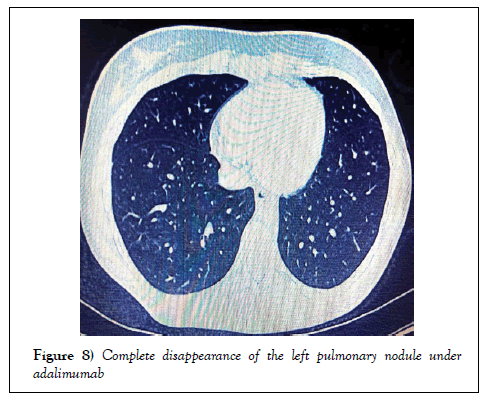
The hypotheses of sarcoidosis and tuberculosis have been mentioned. The quantion was negative and the angiotensin converting enzyme was normal. A pulmonary localization of Crohn’s disease was therefore retained. Initial treatment was changed to HIMURA® (adalimumab). Evolution under this treatment was favorable with regression of the clinical symptoms (digestive and articular disorders and basi-thoracic pains) and a regression of the size of the pulmonary nodules (Figures 7 and 8).
This good evolution was at the cost of an inaugural outbreak of cutaneous psoriasis. Topical local treatment of psoriasis was not enough. Stopping the treatment allowed the disappearance of psoriasis. It is currently under ustekimab (Stelara®) and has a good clinical and biological evolution.
Results
Extra-digestive manifestations of inflammatory diseases of the digestive tract concern 25 - 35% of patients and mainly affect the osteoarticular, dermatological and ophthalmic system [7,8]. Specific pulmonary involvement of CD has been described since 1976 but is rare [9]. According to several authors, the prevalence of these pulmonary disorders is less than 0.4% of all these extra-digestive manifestations [4,7,8]. This unusual location of CD in our case was about a female subject; as it was described in the literature [2,3,7,8]. The only known antecedent was active smoking at the time of diagnosis, a recognized risk factor for CD. Clinically, most attacks are often subclinical [1,4,10-13]. These pulmonary lesions associated with CD are divided into two major groups: the attacks occurring as complications of the treatment and those related to the CD proper. When the diagnosis is later, the treatment may be incriminated including sulfasalazine, methotrexate or derivatives of mesalazine [5,7], responsible for eosinophilic pneumonia, interstitial lung disease, alveolitis or bronchiolitis obliterans. In these cases, the lesions do not include epithelioid granuloma [7]. The actual lesions associated with CD are granulomatous infiltrations or even necrotic pulmonary nodules [1,3,4]. In primary CM lesions, radiological images are not specific [14,15] only the presence of a gigantocellular epithelioid granuloma without caseous necrosis may make the diagnosis evoke while evoking the other pathologies associated with granulomas. To explore the differential diagnosis, we chose to do a surgical biopsy to look for infectious agents and to have a histological study of quality. In histology the lesion was a gigantocellular epithelioid granuloma with foci of necrosis. This lesion is unusual during Crohn’s disease and therefore posed a problem of differential diagnosis with tuberculosis. Given the fact that the patient had never resided in a tuberculous endemic country, the absence of tuberculous contagion, the negativity of quantification, the diagnosis of tuberculosis seemed not very certain. Lack of mediastinal lymphadenopathy; the assay of the normal conversion enzyme and the necrotic nature of the lesion eliminated the differential diagnosis of sarcoidosis. In sum, the regression of the size of these nodules under anti-TNFα was the strongest argument supporting us in this diagnosis of pulmonary localization of CD. This case seems even more interesting for two reasons. The first reason is the summary mode of clinical presentation with isolated disabling chest pain due to isolated pulmonary parenchymal involvement. However, according to the cases described in the literature, the clinical picture was still dominated by dyspnoea, disabling productive cough and haemoptysis. This mode of presentation was related to the most frequent tracheal and bronchial locations of the disease, which can lead to stenosis, bronchiectasis or chronic bronchitis [2,3,7,8]. The second reason is the early character of this pulmonary involvement, whereas it is reported that these pulmonary disorders occur several years after the onset of the digestive disease and evolve in parallel with the degree of activity of intestinal disease [1,6]. A pulmonary localization of CD should therefore be mentioned in case of any respiratory symptoms from a patient followed for MC regardless of the duration of the disease. Therapeutically there was an evolution of the disease with new visceral involvement including pulmonary azathioprine prescribed first intention. In the literature it is recommended to treat any case of moderate-to-severe IBD with TNFα antagonist in patients who have not responded adequately to conventional treatment including corticosteroids and Azathioprine or 6-mercaptopurine, or in whom this treatment is poorly tolerated or contraindicated [14]. The use of anti-TNFα (adalimumab) allowed a regression of digestive, articular and pulmonary symptoms. The advent of this anti-TNFα has revolutionized the management of several inflammatory diseases, particularly inflammatory bowel diseases. It is a more aggressive therapy that induces earlier remission of the disease. However, these anti-TNFα have side effects that can lead to discontinuation of therapy. The increasingly frequent use of anti-TNFα agents has revealed the existence of initially unrecognized cutaneous side effects, some of which are described as “paradoxical effects”. The “paradoxical” side effect induced by these treatments is defined by the appearance of a pathology, itself usually treated with anti-TNFα such as psoriasis [16,17]. This condition is more often reported, with an incidence of 10% in patients treated with anti-TNFα and predominant in women in (70%) of cases [17]. The induction of de novo psoriasis is more frequent than its aggravation under treatment, it can occur with all the molecules, but the risk seems higher for adalimumab [18] which was used for our patient. The replacement of an anti-TNFα by another anti- TNFα does not seem to bring a benefit on the cutaneous level because of the important risk of cross-reactions [17]. This is why the therapeutic line has been changed by ustekimab (Stelara®) which is an inhibitor of interleukins IL-12 and -23 with a good evolution.
Conclusion
Crohn’s disease is a pathology of the young subject. Its expression is primarily digestive but extra-digestive manifestations are possible. Among them, pulmonary involvement is rare and is an expression of the progressive nature of the disease. This localization may cause a diagnostic problem with tuberculosis, sarcoidosis and other granulomatous pulmonary pathologies.
REFERENCES
- Aydin Y, Nilgum YD, Derya H, et al. Pulmonary involvement in inflammatory bowel disease. World J Gastroenterol. 2010;16:4952-4957.
- Levraut M, Martis N, Leroy S, et al. Atteinte pulmonaire associée à la MICI: une manifestation extra digestive mal connue. À propos de 2 cas. Rev Med Int. 2017;38:A110–A225.
- Montembault S, Le gall C, Balian A, et al. Atteinte trachéo-bronchique ulcéro-nécrotique au cours d’une maladie de Crohn. Gastroenterol Clin Biol. 2001;25:197-199.
- Bouchentouf R. Les manifestations respiratoires des maladies inflammatoires chroniques de l’intestin. J Fran Viet Pneu. 2012;03:1-45.
- Camus P, Piard F, Ashcroft T, et al. The lung in inflammatory bowel disease. Medicine (Baltimore). 1993;72:151-183.
- Casey MB, Tazelaar HD, Myers JL, et al. Non-infectious lung pathology in patients with Crohn’s disease. Am J Surg Pathol. 2003;27:213-219.
- Roblin E, Pecciarini N, Yantren H, et al. Atteinte granulomateuse pulmonaire précédant le diagnostic de maladie de Crohn: à propos d’un cas pédiatrique. Arch Pédiatr. 2010;17:1308-1312.
- Lu DG, Ji XQ, Zhao Q, et al. Tracheobronchial nodules and pulmonary infiltrates in a patient with Crohn's disease. World J Gastroenterol. 2012;18:5653-5657.
- Kraft SC, Earle RH, Roesler M, et al. Unexplained bronchopulmonary disease with inflammatory bowel disease. Arch Intern Med 1976;136:454-459.
- Louis E, Louis R, Drion V, et al. Increased frequency of bronchial hyperresponsiveness in patients with inflammatory bowel disease. Allergy. 1995;50:729-733
- Fireman Z, Osipov A, Kivity S, et al. The use of induced sputum in the assessment of pulmonary involvement in Crohn's disease. Am J Gastroenterol. 2000;95:730-734.
- Kuzela L, Vavrecka A, Prikazska M, et al. Pulmonary complications in patients with inflammatory bowel disease. Hepato-Gastroenterol. 1999;46:1714-1719.
- Majewski S, Piotrowski W. Pulmonary manifestations of inflammatory bowel disease Arch Med Sci. 2015;11:1179-1188.
- Camus P, Colby TV. The lung in inflammatory bowel disease. Eur Respir J. 2000;15:5-10.
- Krishnan S, Banquet A, Newman L, et al. Lung lesions in children with Crohn’s disease presenting as non-resolving pneumonias and response to infliximab therapy. Pediatrics. 2006;117:1440-1443.
- Bouhnik Y. Place des anti-TNF dans le traitement d’entretien de la rectocolite hémorragique. Hépato-Gastro et Oncologie digestive. 2014;21:249-253.
- Faure P, Rahier JF, Buche S. Lésions cutanées induites par les anti-TNF-alphaSkin lesions induced by anti-TNF-alpha agents. Acta endoscopica. 2011;41:292.
- Harrison MJ, Dixon WG, Watson KD, et al. Rates of new-onset psoriasis in patients with rheumatoid arthritis receiving anti convient tumour necrosis factor a therapy: results from the British Society for Rheumatology Biologics Register Control. Ann Rheum Dis. 2009;68:209-221.