Cryotherapy in the treatment of small renal tumors over the recent years: A review of the literature and update
Received: 10-Sep-2018 Accepted Date: Oct 30, 2018; Published: 20-Nov-2018
Citation: Venyo AKG. Cryotherapy in the treatment of small renal tumors over the recent years: A review of the literature and update. Pulsus J Surg Res. 2018;2(2):69-75.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Surgical excision, either by means of radical nephrectomy or by partial nephrectomy is the accepted gold-standard treatment of curative intent for localized carcinomas of the kidney (Stage T1 Renal carcinomas). Nevertheless, recent advances in medical technology has enabled the development of new minimally invasive treatment options for localized carcinomas of the kidney and one of these options is cryotherapy of localized renal carcinoma which have been used to treat these tumors in some specialized centres sporadically. Sporadic publications have illustrated that cryotherapy of small kidney tumors can be undertaken safely and with short hospital stay as well as near 100 percent destruction of tumour tissue. Cryotherapy of small renal tumors can be undertaken under radiological imaging control (contrast ultrasound scan, contrast CT scan, contrast MRI scan). Cryotherapy of small localized renal tumors can be undertaken by means of percutaneous cryotherapy of the kidney lesion, laparoscopic cryotherapy of the small renal lesion, or open surgical cryotherapy of the small renal lesion. Biopsies tend to be taken prior to the cryotherapy to confirm diagnosis of renal cell carcinoma or the cell type of tumour. Cryotherapy of small localized renal lesions can be undertaken in old patients and in patients with comorbidities without any significant complications. The short- and medium-term outcome, is similar to the gold standard laparoscopic/open partial nephrectomy, but the advantage of cryotherapy is that the procedure is less expensive and associated with short hospital stay and in the event of the occasional finding of residual disease this can be treated by further cryotherapy or surgical excision without jeopardizing the life of the patient. The renal function of patients who undergo cryotherapy of kidney tumors tends to be maintained in all cases. There is however, paucity of literature on cryotherapy of renal tumors with long follow-up. Summations related to cryotherapy of renal tumors would include the ensuing: Cryotherapy of small localized renal tumors tends to be associated with destruction of the renal tumors with hardly any residual disease and with similar short-term and medium-term oncologic and survival outcome as the gold standard surgical excisions and with short hospital stay and less cost. A multi-centre global trial of cryotherapy of small renal tumors with a long period of follow-up would be recommended to illustrate that cryotherapy of small renal tumors would be a strong competitive gold standard primary treatment option associated with minimal cost.
Keywords
Cryotherapy; cryo-ablation; renal carcinomas; renal lesions; kidney lesions; percutaneous; laparoscopic; RENAL score; estimated glomerular filtration rate; residual disease; contrast CT scan; contrastenhanced MRI scan; ultrasonography
Introduction
Cryotherapy is an ablative treatment option for the management of various malignancies which tends to be associated with less morbidity in comparison with conventional extirpative surgical excision procedures. Over recent years cryotherapy has been successfully utilized in some centres in the treatment of carcinomas of the kidney and carcinomas of the prostate gland [1]. Because cryotherapy of carcinomas of the kidney do not tend to be undertaken in the majority of hospitals globally many clinicians could be unaware of the potential usefulness of cryotherapy of kidney tumors as an option of treatment in certain situations. The ensuing article contains a review of the literature on cryotherapy of tumors that have been recently undertaken globally and this has been divided into (A) overview and (B) miscellaneous narrations from reported cases and studies.
Results
Overview
Cryotherapy is a terminology which refers to the local or general use of low temperatures in medical therapy. Cryotherapy is utilized to treat various benign and malignant lesions of the body [2] Cryotherapy is a medical terminology which was derived from Greek; “Cryo” which means cold and “therapy” which means a cure.
Other terminologies: Other terminologies that tend to be used instead of cryotherapy include: [2]
• Cryoablation
• Cryosurgery
Mechanism of action: The mechanism of cryotherapy could be divided into 3 phases: (1) Heat transfer, (2) Cell injury, and (3) Inflammation [2].
Treatment modalities using cryotherapy: Treatment modalities that are utilized in cryotherapy to treat lesions include: [2]
• Spray freeze technique
• The applicator technique
• The cryoprobe method
• The thermo-coupler method
Clinical applications: Cryotherapy can be used in the treatment of various conditions and some of these include:
• Treatment of a pigmented lesion
• Treatment of a vascular lesion
• Treatment of cysts and tumors
• Treatment of other lesions
• Keloids
• Rhinophyma
• Actinic keratosis
• Cryolipolisis
Complications: Some complications can occur with the utilization of cryotherapy to treat different lesions and in general irrespective of which lesion or lesions are being treated the complications of cryotherapy can be divided into (1) acute complications; (2) delayed complications; (3) prolonged-temporary complications; (4) permanent complications [2].
• Acute complications: Some of the acute complications that could ensue cryotherapy in general include (A) development of a headache. (B) pain, and (C) development of blister at the ablation site
• Delayed complications: Some of the delayed complications that could be associated with cryotherapy, in general, include (A) hemorrhage, (B) infection/abscess formation, (C) formation of excessive granulation tissue
• Prolonged-temporary complications: Some of the prolonged but temporary complications associated with the utilization of cryotherapy, in general, include (A) milia; (B) hyper-pigmentation; (C) development of change in sensation
• Permanent Complications: Some of the permanent complications that can ensue cryotherapy, in general, depending upon the site and organ of the body that has been treated include (A) alopecia, (B) atrophy, (C) keloid formation; (D) scarring; (E) hypopigmentation; (f) ectropion formation
Outcome: The possible outcomes that can ensue cryotherapy of a lesion or lesions include:
• Complete treatment and resolution of the lesion without any residual disease
• Treatment of the lesion with partial resolution of the residual lesion but presence/persistence of residual disease
• Initial apparent resolution of the lesion but subsequent development of local recurrence and or subsequent development of the same lesion at a distant site which in the case of a malignancy would be the development of metastasis or loco-regional disease
With regards to treatment of carcinoma of the kidney by cryotherapy it is important to establish at the end of the cryotherapy procedure whether there has been complete resolution of the lesion at the end of the procedure or there is residual disease or there will subsequently be development of local recurrence or distant metastasis and for this reason radiological imaging tends to be undertaken at the end of the procedure, and subsequent radiological imaging at 1 month, 6 months, one year and yearly after that in some cases.
Contraindications: Contraindications to cryotherapy can be divided into two groups as (a) relative contraindications; and (b) absolute contraindications [2].
Relative contraindications: Relative contraindications for the utilization of cryotherapy include (a) cold intolerance; (b) cold urticaria; (c) cryoglobulinemia; (d) previous history of pyoderma gangrenosum; and (e) Raynaud disease [2].
Absolute contraindications: The use of cryotherapy near the margin of the eye is an absolute contraindication [2].
Recent use of cryotherapy in urology: Cryotherapy is sporadically being used to treat some selected cases of kidney tumors and carcinomas of the prostate gland but because cryotherapy of kidney cancer is not available in the majority of hospitals clinicians may not be very familiar with treating kidney tumors with cryotherapy
Miscellaneous narrations and discussions from some reported cases and studies
Aboumarzouk et al., [3] undertook a systematic review and meta-analysis that included studies which had compared laparoscopic and percutaneous cryotherapy for kidney tumors. The outcome of the study did include incomplete tumor ablation, local recurrence of a tumour, cancer-specific survival, procedure time, transfusion rates, hospital stay, as well as complications associated with the procedures. With regards to the results, Aboumarzouk et al., [3] reported that they had included in the study, a total of 1,475 patients of which 788 of the patients had undergone laparoscopic cryotherapy of a renal tumor and 687 patients had undergone percutaneous cryotherapy of their renal tumors. Aboumarzouk et al., [3] summated the findings of their study as follows:
• A statistical difference existed that favored the laparoscopic group in relation to having had less incomplete tumor ablation (P=0008), and higher cancer-specific survival patients (P=0.04)
• Nevertheless, the laparoscopic cryoablation group of patients did have longer hospital stays (P<0.00001), as well as laparoscopic cryoablation treatment procedures, were more-costly, in comparison with the percutaneous cryoablation procedures
• More Clavien-1 complications were found associated with the percutaneous cryoablation procedures which were significant (P=0.001) in comparison with the laparoscopic cryoablation procedures, but more Clavien-III complications were found in the laparoscopic ablation group (P=0.001)
• No other differences were found in any other outcome parameters
Aboumarzouk et al., [3] concluded that laparoscopic cryoablation of renal tumors was found to be associated with less incomplete tumor ablation rates and with higher cancer-specific survival rates; nevertheless, higher time of hospitalization, more major complications that amounted to Clavien -III complications, and laparoscopic cryoablation procedures were more expensive in comparison with the percutaneous ablation procedures.
It would be argued that cryotherapy as treatment for small renal tumors at the moment is not a widely adopted form of treatment for small renal tumors and that before cryotherapy is globally adopted as an alternative standard treatment, it would be a good idea to undertake a large multicenter trial that would compare cryotherapy with partial nephrectomy for small renal tumors to ascertain the comparative long-period outcomes of both treatment modalities.
Enikeev et al., [4] undertook a study that involved 12 patients whose ages had ranged between 52 years and 76 years who had undergone ultrasoundscan- guided per-cutaneous cryo-ablation of kidney tumors from 2015 to 2017. In 11 of the12 patients, the size of the tumor mass was 3.0 cm (T1a), and in one patient the tumor had measured 4.5 cm (T1b). Enikeev et al., [4] reported that Doppler ultrasound scan. Contrast-enhanced MSCT scan and conventional 3-dimensional modeling had been undertaken in all patients pre-operatively, and at 6 months pursuant to the cryotherapy procedure to assess the size and extent of a tumor as well as the spatial location of a kidney tumor internal surface to the pelvicalyceal system. With regards to all the patients, the tumors were found to be positioned along the posterior or lateral surface of the kidney, within the lower or middle segment, and without invasion of the renal sinus. Intraoperatively immediately, prior to the cryo-ablation procedure biopsies of each tumor was taken and histological examination of all the biopsy specimens confirmed a diagnosis of renal cell carcinoma. Enikeev et al., [4] summated their results as follows:
• Endotracheal, spinal, local, and intravenous anesthesia was utilized in 1, 6, 5, and 1 patient respectively
• The mean duration of the cryo-ablation session was 60 minutes
• Doppler ultrasound scan undertaken 6 months pursuant to the cryotherapy did show that in 11 patients who had T1a tumors, the size of a tumor had decreased by an average size of 8 mm with no evidence of blood flowing into the tumors
• MSCT scan with 3-dimensional modeling undertaken 6 months pursuant to the cryotherapy did show a decrease in the size of a tumor and total absence of contrast agent accumulation, or contrast accumulation gradient not exceeding 10 Hounsfield Units (HU) in comparison with approximately 200 HU preceding the cryotherapy. With regards to the patient who had a T1b renal cell carcinoma, MSCT scan did show a decrease in the size of a tumor from 4.5 cm to 3.7 cm; nevertheless, there was a mass which did measure up to 1.5 cm that had a high gradient of contrast agent accumulation. This patient did undergo kidney resection (nephrectomy) without developing any intra-operative or post-operative complication
Enikeev et al., [4] made the ensuing conclusions: Their accumulated experience had enabled them to confirm the effectiveness and safety of ultrasound scan-guided percutaneous cryo-ablation and which had enabled them to recommend ultrasound scan guided per-cutaneous cryo-ablation of renal tumors as a treatment modality of choice for patients who have Stage T1a carcinoma of the kidney which is positioned along the posterior and lateral surface of the kidney within the lower and middle segment of the kidney without renal sinus invasion.
It would be argued that despite the promising short-term outcome reported by Enikeev et al., [4] a long period of follow-up is required with regards to the treatment of malignant lesions and even though the short term outcome pursuant to cryotherapy for small renal tumors in this study appears promising, there is need to undertake a large-scale multi-centre study that has a long period of follow-up to confirm the long-term outcome of cryotherapy to enable clinicians decide globally whether to accept cryotherapy as a good treatment option for small malignant renal tumors or not.
Pessoa et al., [5] undertook a systematic review and cumulative analysis of comparative studies related to laparoscopic versus percutaneous cryoablation of small renal masses by performing a systematic review of the literature that had been undertaken through to March 2016. They summarized the results of their analyses as follows:
• Out of 1725 cases of cry-ablation of renal cancer, 804 (46.6%) individuals had been treated by means of percutaneous cryo-ablation, and 921 individuals (53.4%) had been by means of laparoscopic cryoablation of the renal tumors
• Percutaneous cryo-ablation had been undertaken more frequently for tumors that had been located posteriorly (P<0.001); on the other hand, laparoscopic cryo-ablation was more often undertaken for lesions that were endophytic (P=0.01)
• With regards to length of follow-up of the patients, the length of follow-up lasted longer for the laparoscopic cryo-ablation (P<0.001). Percutaneous cryo-ablation was found to be associated with a hospital stay that was significantly shorter (P<0.001)
• A likelihood of finding residual disease was found to be lower for laparoscopic cryo-ablation (P=0.003); furthermore, tumor recurrence rate did favor cryo-ablation of the renal lesions (P=0.02). The two procedures of laparoscopic and percutaneous cryo-ablation of the renal tumors were similar for recurrence-free survival (P=0.008), as well as for overall survival (P=0.51). There was no significant difference found with regards to the post-operative estimated glomerular filtration rate (eGFR) (P=0.78)
Pessoa et al., [5] made the following conclusions:
• Laparoscopic and percutaneous cryo-ablation of the kidney lesions did offer similar oncological outcomes with minimal effect on renal function
• Percutaneous access for cryotherapy of kidney tumors could offer a shorter stay in hospital as well as faster recovery, which could be appealing in an era of cost-restraint
It would be argued that Pessoa et al., [5] had done a good job comparing laparoscopic cryo-ablation with percutaneous cryo-ablation of small renal tumors; however, what is needed is a comparison of cryotherapy with standard partial nephrectomy associated with a long period of follow-up to enable clinicians decide whether to regard cryotherapy as an alternative treatment option for small renal tumors that are associated with good longterm outcome as partial nephrectomy or not.
Bertolotto et al., [6] did investigate whether persistent enhancement that is detected upon contrast-enhanced sonography at post-operative day 1 (early contrast-enhanced sonography) pursuant to cryo-ablation of renal tumors does imply the presence of residual valuable tumour tissue, defined as residual enhancing tissue upon reference radiological imaging by means of computed tomography (CT) scan, or magnetic resonance imaging (MRI) scan that is performed 6 months pursuant to the cryoablation procedure. With regards to the methods, Bertolotto et al., [6] reported the following:
• Seventy-four patients who had had percutaneous cryo-ablation of kidney tumors who had had early contrast-enhanced sonography from November 2011 to August 2015
• Two independent readers had evaluated the early contrast-enhanced sonography findings as well as contrast-enhanced sonography investigations that were undertaken 1 month pursuant to the cryoablation of the renal lesions that had shown enhancement on early contrast-enhancement sonography. They did score intralesional enhancement in 4 groups which included: (a) no enhancement, (b) few intralesional vessels, (c) focal enhancing areas, and (d) diffuse enhancement. With regards to an inter-reader agreement in relation to the evaluation of lesion vascularity upon early contrast-enhanced sonography, this was assessed using weighted k statistics
• Computed Tomography (CT), or Magnetic Resonance Imaging (MRI) scans which were performed 6 months pursuant to the cryo-ablation procedure was utilized as the reference procedure for the assessment of absence or presence of residual disease
Bertolotto et al. [6] summated the results as follows:
• Inter-reader agreement in the assessment of intra-tumoral vascularization upon early contrast-enhanced sonography was very good (k=0.90)
• Contrast-enhancement was absent for both readers in 33 out of the 74 patients; in 21 patients, only a few intralesional vessels were visualized; in 13 patients, diffuse or focal contrast-enhancement was visualized. With regards to the remaining 7 patients, differences did exist. Four lesions did have focal enhancement on early contrastenhanced sonography and 1 lesion was adjudged avascular and did have residual tumors upon reference imaging. The cryo-ablation was successful in the remaining 69 of the 74 patients (which would amount to 93% of the patients)
Bertolotto et al., [6] concluded that pursuant to cryo-ablation, intratumoral enhancement on contrast-enhanced sonography does not imply there is the viability of tumor cell.
It would be argued that these initial results are promising but there is a need for a larger study with a long period of follow-up to ascertain the outcome of this treatment modality over a longer period of time.
Lalloué et al., [7] evaluated the oncologic and functional outcomes pursuant to Percutaneous Cryoablation (PCA) for renal masses. They retrospectively identified 26 patients who had undergone PCA for 28 kidney tumors between November 2006 and June 2011. They recorded the demographics of the patients and baseline clinical characteristics, features of the tumors, peri-operative information, as well as post-operative outcomes. A biopsy of a kidney tumor was undertaken systematically prior to the cryoablation procedure. Surveillance radiological imaging was undertaken at 1, 3, 6, and 12, months, and yearly thereafter. They did determine the oncological outcomes of the patients by radiological evidence of tumor recurrence, which had been defined by evidence of contrast-enhancement at the site of cryo-ablation upon control surveillance imaging 3 months pursuant to the cryo-ablation. Lalloué et al., [7] summated their results as follows:
• The mean age of the patients was 70.1 years, and the patients had to mean Charlson Comorbidity Index (CCI) and body mass index were 6 and 29 kg/m2 respectively
• There were 11 kidney transplants that included 4 solitary ones. The mean size of the tumors was 29.5 mm and the sub-types and locations of the tumors were: Clear cell renal cell carcinomas which were found in 16 out of the 28 (57.14%) tumors; endophytic tumors in 17 out of 28 (60.71%) tumors; mid-kidney in 14 out of 28 (50%) (± 9.8)
• Twenty- five cryo-ablation procedures were undertaken percutaneous with two by lumpectomy. The mean clearance pre-operative MDRD was 66 mL/min. The mean length of stay 3.3 days (± 2.2). The intraoperative complications did comprise of 2 cases of pneumothorax and 6 minor complications which (≤ 2). There were no major complications encountered. The mean follow-up was 27.5 months (± 15.7). The MDRD clearance distance was 61.9 mL/min. The overall survival and disease-specific survival was 100%, but the recurrencefree survival was 78.6% with 5 recurrences and 1 failure of treatment
Lalloue et al., [7] concluded that percutaneous cryo-ablation provides a safe and oncologically effective treatment option to extirpative surgery for kidney masses in patients who have significant co-morbidities.
Whilst these results would appear promising, a much longer period of follow-up in a similar type of study would be necessary with regards to understanding the long-term outcome of treating small renal tumors by means of radiotherapy.
Dominguez et al., [8] undertook a retrospective analysis of 17 renal tumors which were diagnosed in 16 patients which had been treated by means of cryotherapy. The ages of the patients did range between 43 years and 80 years and the mean age was 66 years. The sizes of the tumors had ranged between 0.7 cm to 3.7 cm and the mean tumor size was 1.8 cm. Cryotherapy had been undertaken by means of double freeze cycle laparoscopically in all cases and in 10 of them trans-peritoneal approach was adopted and in 7 cases retroperitoneal approach was used. Dominguez et al., [8] summarized their results as follows:
• Peri-operative biopsies of the renal lesions had been undertaken in all cases and histological examination of the specimens had been positive with regards to 10 (59%) of the cases
• The mean hospital stay was 2.8 days and the mean operating time 162 minutes
• All the cases were treated by means of laparoscopic cryotherapy with the exception of one case which was converted to open surgery cryotherapy because of bleeding
• With regards to complications, one patient did require a blood transfusion within the immediate post-operative period. Most of the complications had been Clavien-Dindo grades I and II. Seventy-six percent of the patients did not develop any complication. After a follow-up that ranged between 6 months and 102 months and a mean follow-up of 31 months, 1 patient had died from non-tumour related causes, and 12 patients who constituted 75% of the patients did show no evidence of local tumor recurrence or tumor progression. One patent did have persistence of a tumour and therefore did undergo partial nephrectomy at 6 months. One patient did develop a metachronous tumor recurrence in the same kidney at 36 months, and another patient did develop another tumor recurrence at 23 months
Dominguez et al., [8] concluded that Laparoscopic cryotherapy of renal tumors is a safe and feasible option of treatment and the technique would constitute a good alternative treatment option to surgery for selected kidney tumors.
It would be argued that long-term outcome studies are necessary to enable clinicians to establish if a treatment option of any type of malignancy is good. The study of Dominguez et al., [8] appears to be associated with a reasonable outcome but there is the need to undertake a further similar study recruiting a larger number of patients who would be followed up for a long time to ascertain the long-term outcome of the disease.
Rodriguez-Faba et al., [9] undertook a prospective study of 28 patients who had posterior-facing T1a kidney tumors with middle and inferior external borders. They reported that all the patients had undergone ultrasound scan-guided Percutaneous Renal Cryotherapy (PRC). All the patients had undergone follow-up surveillance Computed Tomography (CT) scan at 1 month and every 6 months, and good CT scan result was defined the total absence of contrast incorporation. They did utilize Kaplan Meier estimator to analyze their descriptive and survival study. Rodriquez-Faba et al., [9] summarized their results as follows:
• Twenty-eight percutaneous renal cryotherapy procedures were undertaken on 28 patients who had a mean age of 68.3 years (standard deviation of 10.1 years)
• The tumors had a mean size of 25.5 mm with a standard deviation of 7.5 mm. The mean nephrometry score was 1.41 with a standard deviation of 0.52. The mean pre-operative serum creatinine was 133.5 (144.1) m-mols/L
• There were no intra-operative complications and with regards to postoperative complications, there was only 1 patient, (3.5%) who developed a skin lesion that resulted in the treatment of a tumor in a transplanted kidney which was classified as Clavien II
• The median follow-up of the patients was 25 months and the mean postoperative serum creatinine was recorded as 133.5 (110.3) mmol/L. Two patients were found to have developed radiological recurrences (93% efficacy), and their mean time to recurrence 12 months and 19 months respectively. No tumor-related deaths ensued
Rodriguez-Faba et al., [9] made the following conclusions:
• Their series of patients which was the largest series in their country on PRC at the time of publication of their paper did show that, with an appropriate selection of tumors, PRC is a safe technique which is associated with minimal morbidity
• Ultrasonography does enable the controlled performance of the procedure and does save the patient from radiation as well as it does reduce the cost of treatment
It would be argued that the study of Rodriguez-Faba et al., [9] was a good study that contained a small number of patients who were followed up for a relatively short period of time and in view of this there is the need for another study that would recruit a larger number of patients who would be followed up for a long period of time to determine the long-term outcome of patients who have undergone the procedure.
Khoder et al., [10] undertook a prospective non-randomised study between April 2007 and October 2009 that had included 16 patients whose ages had ranged between 48 years and 80 years and whose mean age was 68 years and who did have peripherally located renal tumors that were candidates for nephron-sparing surgery of which 5 were candidates for open partial nephrectomy (OPN) and 11 were candidates for Laparoscopic Partial Nephrectomy (LPN). All patients in the study had undergone cryoablation of a Renal Tumor (RT) that was followed in the same session by Open Partial Nephrectomy (K-OPN) and Laparoscopic Partial Nephrectomy (K-LPN). They did estimate the peri-operative and followup parameters. For retrospective comparison as a control group, a matched pair cohort of 41 patients, 20 of whom had had open partial nephrectomy (OPN), and 21 who had had Laparoscopic Partial Nephrectomy (LPN) as standard operations due to the same indications were selected. Khoder et al., [10] summated the results as follows:
• The ages of the patients who did undergo Open Partial Nephrectomy (K-OPN) had ranged between 69 years and 83 years and their mean age was 74 years and this group of patients did have blood loss that ranged between 50 millilitres and 200 millilitres and their mean blood loss was 140 millilitres. The ages of the patients that underwent Laparoscopic Partial Nephrectomy (K-LPN) did range between 48 years and 80 years and their mean age was 66.6 years. The blood loss in this group had ranged between 50 millilitres and 700 millilitres and the mean blood loss was 100 millilitres
• All the operations/the procedures had been completed successfully without the need to convert to open surgery in the cases of the Laparoscopic Partial Nephrectomy (K-LPN), and all the operations were undertaken without transfusions or intra-operative complications
• In comparison with the previously undertaken Open Partial Nephrectomy (OPN)/Laparoscopic Partial Nephrectomy (LPN) group, the cryotherapy followed by the Open Partial Nephrectomy (K-OPN) and cryotherapy followed by Laparoscopic Partial Nephrectomy (KLPN) group were found to be associated with a longer operating time (P<0.05) and a comparable post-operative hospital stay. No early postoperative complications developed. Cryo-ablation did not affect the histopathological evaluation of the tumors and the resection margins of the specimens. Histopathology examination did show cytologic changes that suggested fresh coagulative necrosis, glomerular vascular congestion as well as interstitial hemorrhages following cryotherapy. One patient who had Laparoscopic Partial Nephrectomy following cryotherapy (K-LPN) did develop a pararenal abscess that necessitated puncture after 7 weeks. The follow-up which did range between 9 months and 42 months was uneventful
Khoder et al. [10] made the ensuing conclusions:
• Their study did show that K-LPN is feasible without increasing procedure morbidity or compromising surgical and oncological outcomes
• K-LPN does not add any advantage to tumor excision
• The pathological findings did document early cryoablation effects but viable tissue
It would be argued that even though the results of Khoder et al., [10] do appear promising, there is the need to convince all and sundry that cryoablation (cryotherapy) would be a gold standard alternative treatment modality for small renal tumors which could be achieved by undertaking a large-scale random controlled trials recruiting patients of all age groups who can be followed up for a long time and if the results are proven to be good in the long-term then cryo-ablation (cryotherapy) can then be recommended to be considered as an option of choice for the treatment of small renal tumors of all age groups rather than for the old and frail patients who are not fit to undergo open surgery.
Sisui et al., [11] undertook a retrospective multi-center analysis of 154 consecutive patients who had undergone either ultrasound scan-guided laparoscopic renal cryoablation (LRC) which included 88 patients, or Computed Tomography (CT)-guided Percutaneous Renal Cryoablation (PRC) which included 66 patients from March 2003 to December 2011. They compared RENAL score and demographics with post-operative complications (Clavien). They did carry out multi-variable analysis factors associated with the development of post-procedure complications. Sisui et al., [11] summarized their results as follows:
• The mean age of the patients was 68 years of whom 94 were men and 60 were women
• The follow-up did range between 23.6 months and 45.6 months and the median follow-up was 34 months
• The mean size of a tumor was 2.6 ± 1 cm. The mean RENAL score was 5.2 ± 1.4. Differences within Anterior/posterior component and Hilar domain of the RENAL scores had been noted, with percutaneous renal cryoablation (PRC) that favored posterior tumors and hilar lesions in comparison with laparoscopic renal cryoablation (LRC) (P<0.001 and P=0.044) respectively
• There ensued 14.9% complications, all of which had been adjudged to be low-grade (Clavien 1, 2)
• There were no differences in complications between Laparoscopic Renal Cryoablation (LRC) and the Percutaneous Renal Cryoablation (PRC) (15.9% versus 13.6%, P=0.82). Majority of the complications was hemorrhagic which did occur in 9 out of 154 patients (5.8%), significant increase within the hemorrhagic rate was observed for patients with “N” (“nearness”) component score of 2 or 3 (5/36, or 13.9%), in comparison with patients with patients who had “N” score of 1 (4/115 or 3.5%, p=0.033). The multi-variable analysis did show that increasing RENAL score had been associated with postprocedure complications (odds ratio [OR]=1.37, P=0.025). The multivariable analysis did show that when separated into individual domains, “N” score 3 was adjudged to be significantly associated with postoperative complications (OR 16.15, P=0.027)
Sisui et al. [11] made the ensuing conclusions:
• The increasing RENAL score was associated with the development of post-procedure complications
• Further investigation would be required to elucidate the role of the RENAL nephrometry score in risk stratification preceding renal cryotherapy
It would be argued that the results of Sisui et al., [11] are promising; nevertheless, there is the need to undertake a larger multi-center trial recruiting patients of all age groups who have small renal tumors and who would be followed up for a longer period of time in order to establish the long-term outcome of cryo-ablation in small renal tumors.
Cordeiro et al., [12] undertook a literature search on laparoscopic cryotherapy for small renal masses. They reported that they had selected 27 reports that had addressed Laparoscopic Cryoablation (LCA) for Small Renal Masses (SRMs). The number of patients per study did range between 20 and 144. The mean age of the patients across the series had ranged between 62 years and 73 years. The mean size of the renal tumors did range between 2.7 cm to 4 cm but the majority of the tumors were less than 3 cm. Overall, more than 55% of the ablated renal lesions had been confirmed by pathology examination of specimens of the lesion as renal cell carcinoma. The follow-up of the patients had ranged from 9 months and 93 months. Seven series had documented a follow-up longer than 36 months. Four urology groups did report intermediate- and long-term outcomes. Tumour persistence rates did range 0% to 17% and tumor recurrence rates between 0% and 14%. The overall complication rates had ranged from 0% to 40%. Cordeiro et al., [12] made the following conclusions:
• Retrospective observational data and few prospective series on LCA of SRMs had shown acceptable oncological 3- to 5-year outcomes as well as with a low recurrence rate
• LCA had proven to be a safe procedure with an overall low complication rate
• LCA is mainly indicated for SRMs in elderly patients who are affected by co-morbidity and high surgical risk tumors within the anterior valve of the kidney or in contact with the ureter or neighboring organs
It would be argued that considering that the longest period of follow-up for laparoscopic cryotherapy was only 93 months, there is the need for a large multi-center study that would recruit a very large number of patients of all age groups who would be followed-up for many years to determine the long-term outcome of patients pursuant to laparoscopic cryotherapy. It would also be stated that it is only after the long-term outcome following laparoscopic cryotherapy for small renal tumors is known that laparoscopic cryotherapy would be promulgated as a good first-line treatment option for small renal tumors.
Long et al., [13] reviewed thirty-seven manuscripts that included 2344 renal lesions that had been treated by Surgical Cryoablation (SCA) or by Percutaneous Cryoablation (PCA). They stated that when they had compared SCA with PCA series, anterior/posterior designation had been reported in 31% versus 47% of the series; endophytic designation had been reported in 17% versus 40% of the series; and polarity designation had been reported in 48% versus 47% of the series (all P values>0.05). With regards to those tumors that had been treated by means of SCA, 44% were anterior lesions, and 28% were posterior lesions; whilst with regards to renal tumors that had been treated by PCA, 9% were anterior and 81% were posterior. Tumour description location had been absent in 32% in 14 out of 44 published series. Long et al., [13] made the following conclusions:
• Despite that the location of a tumor is integral to the choice of treatment renal mass, anatomical tumor description had been vastly underreported in the cryotherapy literature
• Approximately, one-third of renal tumor masses that had been treated by SCA, was on the posterior surface of the affected kidney and could be amenable to treatment by means of PCA, thus avoiding the risk of general anesthesia and intra-abdominal dissection in co-morbid cohorts
• Better reporting objective measures of tumor anatomy and location in cryotherapy literature could facilitate standardization of treatment protocols in patients who have renal masses
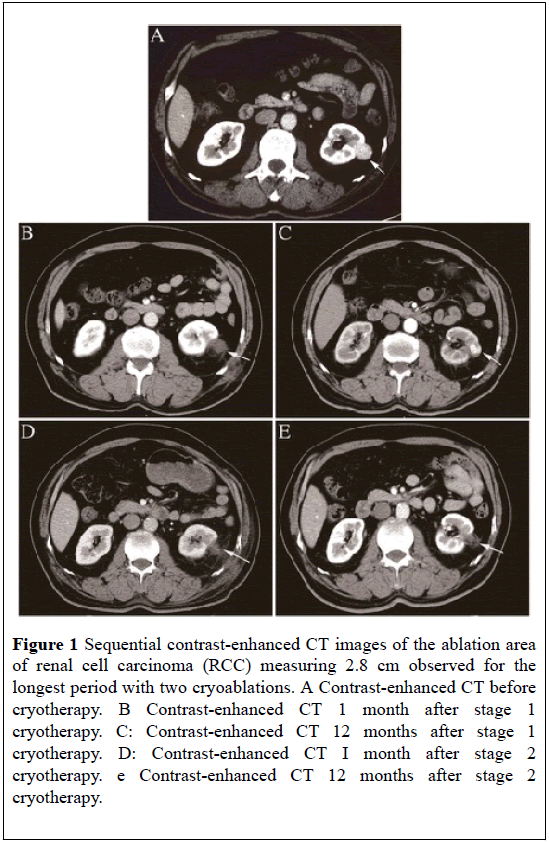
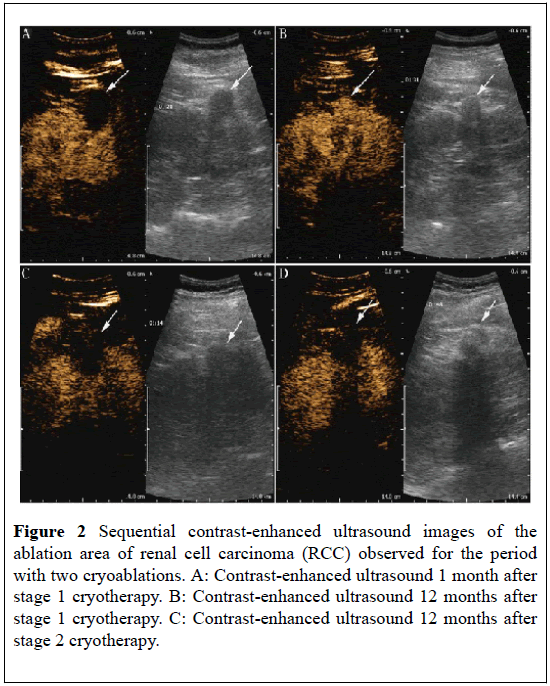
Yan et al., [14] undertook a study to evaluate the feasibility, safety, and therapeutic effects of percutaneous renal cryoablation under local anesthesia with conscious sedation for patients who had unresectable stage 1 (T1N0M0) Renal Cell Carcinoma (RCC) in high surgical risk Yan et al., [14] reported 18 patients who were not candidates for surgical operation who had undergone primary cryotherapy guided by gray-scale ultrasound. Contrast-Enhanced Ultrasonography (CEUS) and contrast-enhanced Computed Tomography (CT) were undertaken to evaluate treatment at the completion of treatment (Figures 1 and 2). They reported that the followup period had ranged between 12 months and 56 months and the mean follow-up was 26.8 months. All tumors were biopsied preceding cryotherapy. Seventeen tumors had remained free of enhancement during the period of follow-up. They did not find any major complication associated with the cryoablation procedures, although two instances of sub-capsular hematomas, one of retroperitoneal errhysis and one of nausea were observed pursuant to cryoablation. One patient did develop a local recurrence of a tumor who did receive additional cryoablation. The local tumor control rate was 100% of T1N0M0 tumors including the recurrence case who had undergone additional cryoablation. Yan et al., [14] concluded that percutaneous cryoablation could be recommended as a feasible, safe, and promising option of treatment for a renal tumor, especially those unresectable stage 1 RCC, with a low risk of complications.
Figure 1: Sequential contrast-enhanced CT images of the ablation area of renal cell carcinoma (RCC) measuring 2.8 cm observed for the longest period with two cryoablations. A Contrast-enhanced CT before cryotherapy. B Contrast-enhanced CT 1 month after stage 1 cryotherapy. C: Contrast-enhanced CT 12 months after stage 1 cryotherapy. D: Contrast-enhanced CT I month after stage 2 cryotherapy. e Contrast-enhanced CT 12 months after stage 2 cryotherapy.
Figure 2: Sequential contrast-enhanced ultrasound images of the ablation area of renal cell carcinoma (RCC) observed for the period with two cryoablations. A: Contrast-enhanced ultrasound 1 month after stage 1 cryotherapy. B: Contrast-enhanced ultrasound 12 months after stage 1 cryotherapy. C: Contrast-enhanced ultrasound 12 months after stage 2 cryotherapy.
Conclusion
The reported global experience related to cryotherapy of localized small kidney tumors has indicated that small kidney tumors could be safely and effectively treated by means of cryotherapy (percutaneous, laparoscopic, or open surgical cryotherapy).
Cryotherapy of small renal tumors tends to satisfactorily treat small localized renal carcinomas with very minimal complications and with a very low incidence of residual disease which can be detected by using control contrast CT or contrast MRI scan and any residual disease identified can be re-treated with cryotherapy or surgical excision.
The short- and medium-term outcome of cryotherapy of small renal tumors is good but there is need for further large-scale multi-center trials on cryotherapy of small localized renal tumors to ascertain the long-term prognosis associated with the procedure in order to recommend the procedure as a globally accepted alternative option of treatment as opposed to partial nephrectomy (open or laparoscopic).
Percutaneous cryotherapy of small renal tumors could be safely and effectively undertaken on patients with co-morbidities and old patients in order to reduce morbidities and complications associated with open or laparoscopic surgical operations and to reduce the duration of hospital stay associated with the treatment of small localized renal tumors.
Considering that the long-term outcome following treatment of small renal tumors with cryo-ablation (cryotherapy is not known or generally documented, there is a global need for a large-scale multi-center trial to ascertain the long-term outcome of this treatment modality before one can be promulgated as a treatment option for small renal tumors associated with a good long-term outcome.
REFERENCES
- Mohammed A, Miller S, Douglas-Moore J, et al. Cryotherapy and its applications in the management of urologic malignancies: A review of its use in renal and prostate cancers. Urol Oncol. 2014;32:39.e19-39.e27.
- Unger JG. Cryotherapy. Medscape medicine. 2017.
- Aboumarzouk OM, Ismail M, Breen DJ, et al. Laparoscopic vs Percutaneous cryotherapy for renal tumors: A systematic review and meta-analysis. J Endourol. 2018;32:177-83.
- Enikeev DV, Glybochko PV, Alvaev YG, et al. Ultrasound-guided percutaneous cryoablation of renal tumors: Urologia. 2017;3:68-73.
- Pessoa RR, Autorino R, Laguna MP, et al. Laparoscopic versus percutaneous cryoablation of small renal mass: Systematic review and cumulative analysis of comparative studies. Clin Genitourin Cancer. 2017;15:513-519 e5.
- Bertollo M, Siracusano S, Cicero C, et al. Cryotherapy of renal lesions: Enhancement on contrast-enhanced sonography on postoperative day 1 does not imply visible tissue persistence. J Ultrasound Med. 2017;36:301-310.
- Lalloue F, Ruffion A, Valette PJ, et al. Cryotherapy percutaneous for renal tumors: Our center’s beginning experience. Prog Urol. 2016;26:310-8.
- Dominguez A, Bellido JA, Munoz Rodriguez J, et al. Retroperitoneal and transperitoneal laparoscopic cryotherapy for small renal masses. Actas Urol Esp. 2015;39:582-87.
- Rodriguez-Faba O, Palou J, Rosales A, et al. Prospective Study of ultrasound-guided percutaneous renal cryotherapy: Case selection as an optimization factor for a technique. Actas Urol Esp. 2015;39:8-12.
- Khoder WY, Siegert S, Stief CG, et al. Results of a prospective study comparing the clinical efficacy of cryoablation of renal cell cancer followed by immediate partial nephrectomy. Eur J Surg Oncol. 2014;40:96-102.
- Sisui DM, Liss MA, Palazzi KL, et al. Renal nephrometry score is associated with complications after renal cryoablation: A multicentre analysis. Urology. 2013;81:775-80.
- Cordeiro ER, Barwari K, Anastasiadis A, et al. Laparoscopic cryotherapy for small renal masses: Current State. Arch Esp Urol. 2013;661:41-53.
- Long CJ, Canter DJ, Smaldone MC, et al. Role of tumor location in selecting patients for percutaneous versus surgical cryoablation of renal masses. Can J Urol. 2012;19:6417-22.
- Yan X, Zhang M, Chen X, et al. Image-guided percutaneous renal cryoablation for stage 1 renal cell carcinoma with high surgical risk. World Journal of Surgical Oncology. 2015;13:200.