Daily collaborative meeting: An emerging relationship centered communication model of St Luke’s medical center global city, Philippines
Received: 24-Jan-2018 Accepted Date: Feb 22, 2018; Published: 05-Mar-2018
Citation: Rafael C Solis. Daily collaborative meeting: An emerging relationship centered communication model of St Luke����������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â����������������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����â������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â����������������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â����â������������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����â������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â�����¢����������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â����������������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����â������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â����â������������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â����â������������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����â������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â����â�¬����������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â����������������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����â������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â����â������������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â����â������������â������������â����â����������������â����â��������â����â����������������â������������â����â����â������������â����â��������â����â����â������������â������������â����â����������������â����â��������â����â����â������������â������������â����â����â������������â����â��������â����â����â�¢s medical center global city, Philippines. Pulsus J Surg Res. 2018;2(1):27-33.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Communication is critical in patient experience. It is important to consider that is not just verbal in form. It is imparting thoughts, opinions and information by verbal or written form. One study states that 93 percent of communication is more affected by body language, attitude, and tone, leaving only 7 percent of the meaning and intent based on the actual words said. Whereas the spoken words contain the crucial content, their meaning can be influenced by the style of delivery, which includes the way speakers stand, speak, and look at a person.
Introduction
Communication is critical in patient experience. It is important to consider that is not just verbal in form. It is imparting thoughts, opinions and information by verbal or written form. One study states that 93 percent of communication is more affected by body language, attitude, and tone, leaving only 7 percent of the meaning and intent based on the actual words said. Whereas the spoken words contain the crucial content, their meaning can be influenced by the style of delivery, which includes the way speakers stand, speak, and look at a person.
Interpersonal Communication is an offshoot of the interchange of information between humans.In health care, communication is an exchange of content relating to health. This becomes an avenue of relationship building from among health care workers. Such relationship is premised on various factors, ranging from leader’s characteristics to organizational support. In essence, health care communication is an interpersonal exchange that takes place among health care practitioners.
During the course of a 4-day hospital stay for example, a patient may interact with 50 different employees, including physicians, nurses, technicians, and others. Effective clinical practice thus involves many instances where critical information must be accurately communicated, thus health care communication becomes critical.
The 1999 Institute of Medicine (IOM) report, To Err Is Human: Building a Safer Health System, revealed that between 44,000 and 98,000 people die every year in U.S. hospitals because of medical errors. Even more disturbing, communication failures are the leading root cause of the sentinel events reported to the Joint Commission from 1995 to 2004 [1]. More specifically, the Joint Commission cites communication failures as the leading root cause for medication errors, delays in treatment, and wrong-site surgeries, as well as the second most frequently cited root cause for operative and postoperative events and fatal falls.
Communication failures are an extremely common cause of inadvertent patient harm. Certain elements in the hospital practice environment are important predictors of variation in patients’ outcomes. Patients’ safety is one outcome that has received international attention ever since the Institute of Medicine publication. In the classic study on outcomes of intensive care, communication between nurses and physicians was the single factor most significantly associated with excess hospital mortality. In more recent research, verbal miscommunication between nurses and physicians was responsible for 37% of all errors.
Effective Communication therefore is crucial as it has critical patient safety implications. A communication system that is efficient is integral to provision of quality patient care. As the communication system becomes efficient, professionals in the organization provides quality patient care.
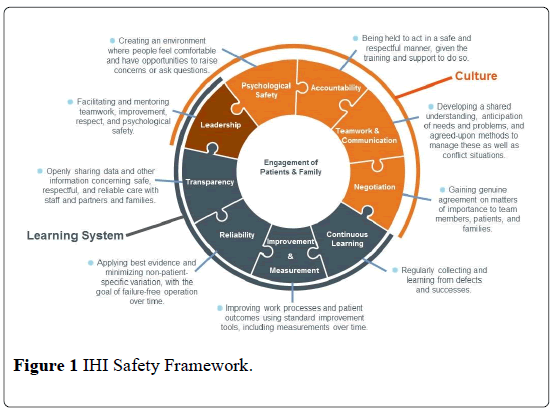
IHI proposed a comprehensive safety framework, where communication is one component. (Figure 1). Underpinning the framework are two essential and interrelated domains: culture and the learning system. In this context, culture is the product of individual and group values, attitudes, competencies, and behaviors that form a strong foundation on which to build a learning system. A learning system is characterized by its ability to self-reflect and identify strengths and defects, both in real time and in periodic review intervals. The culture and learning system domains are both foundational to the framework. There are four cultural components (psychological safety, accountability, teamwork and communication, and negotiation) in addition to one shared component (leadership) that falls within both domains (culture and the learning system).
Communication in health care likewise has patient experience component. It is a complex process where there are contact points. A Moment of Truth which will affect the organization. At each touch point, patients evaluate the quality of care and, ultimately, decide if they will return or recommend the organization to others [2].
Patients’ perceptions of the quality of the healthcare they received are highly dependent on the quality of their interactions with their healthcare clinician and team. This is what Kennedy was pointing as touch points and moments of truth. There is a wealth of research data that supports the benefits of effective communication and health outcomes for patients and healthcare teams. Patient Experience is likewise rich with data as it speaks of outcomes. The patient-centered care model underscores the essential features of healthcare communication which relies heavily on core communication skills, such as reflective listening and empathy, as a way to respond to the unique needs, values and preference of individual patients. This is the heart of patient experience.
In SLMC, patient experience is defined as “The sum total of anticipatory, compassionate, innovative patient centered care of the St Luke’s health care system that impacts the overall perception of patient care”. The anticipatory component of the definition, will prevent the patient experience gap described earlier as falling short of the expectations in the care provided. The requirement to anticipate the needs of our patients is critical in development of a communication model anchored in best practices in patient care.
This paper will present the development of a communication model. The emerging model incorporates the anticipatory patient centered care in the daily collaborative huddles. Likewise, the model development integrates two best practices in communication. Lastly, the paper describes the applicability of the model in the “wow” moments in patient care.
SLMC organizational huddles: the beginnings
Significant to development of SLMC Communication Model is Team work and Communication. IHI Safety framework proposes a strong hallmarks of strong team, where communication becomes the hub. High-functioning teams use structured communication in which they consistently, succinctly, and respectfully share critical information. The Daily Collaborative Huddle is an example of a structured communication where there is sharing of critical information about patient care delivery issues and concerns.
Daily Collaborative Meeting is a means to effective communication. For communication to be effective, critical information needs to be communicated to frontline managers prior to the start of the day’s operation [3]. Effective Communication involves interactive listening. Interactive listening, requires asking questions and reflection. Communication that is effective produces a healthy work environment and fosters team work. A leader who openly communicates with his subordinates can foster positive relationships that benefit the company as a whole. Fundamentally, relationships grow out of communication, and the functioning and survival of organizations is based on effective relationships among individuals and groups.
Patient-centered care model underscores the essential features of healthcare communication which relies heavily on communication as a core. This suggests that communication is the heart of patient experience. As patient experience becomes embedded in the care model, communication needs to be effective. In the mid-1980’s, Parasuraman et al. also considered customer expectations when they proposed their conceptual model of service quality. Patient like customers, compare their perceptions formed during or following the encounter with their service expectations [4]. This gap is a function of service deficiencies in an organization related to understanding customer expectations. Numerous studies support the development of providers’ communication skills. Communication has been favorably affect clinical outcomes, patient experience and patient satisfaction and occurrence of sentinel events.
Wofford as early as 2004 identified disrespect, mismatched expectations of care, inadequate information, and distrust as the most common types of patient complaints about provider behaviors and suggested that these topics be included in training curricula related to professionalism and communication skills [5]. In another study made by Chang in 2006, patient perception of provider listening and explaining, considered components of effective communication impacted global ratings of quality care [6].
The healthcare industry is fundamentally a chaotic world. Poor communication is an important issue, particularly because it can lead to errors and poor patient outcomes. Communication is key in ensuring that chaos is prevented in the hospital setting. When mistakes occur in hospitals, more often than not, they are a result of communication problems rather than just errors in judgment or negligence [7].
It is essential, therefore, to cultivate an environment conducive to effective communication, through appropriate use of communication channels (Kron, 1992). One of the channels can be Huddles. The concept of a “huddle”, a brief meeting between physicians and support staff prior to patient care sessions, had been used as a communication tactic in healthcare settings.
The Institute for Healthcare Improvement (IHI) advocates huddle as a tool to enhance communication, teamwork, efficiency and patient safety (Institute for Healthcare Improvement, 2012). The idea of using quick “huddles”, as opposed to the standard one-hour meeting, arose from a need to speed up the work of improvement teams. “Huddles” enable teams to have frequent but short briefings so that they can stay informed, review work, make plans and move ahead rapidly.
The Huddle Process as a brief meeting to share information normally starts at the beginning of the work day. The brief conference assist members of the team to work together for the common goal of safe, efficient patient care. It is a time to plan contingencies, express concerns, address conflicts and reassign resources. It is also allows staff to discuss, evaluate situations and errors assessing resolution and ultimately eliminate it. The huddle process requires a consistent agenda or format. In SLMC, Huddle Process takes an average of 20.75 minutes, derived from a time and motion assessment done by the Hospital Operations Group last October 15. It starts at seven in the morning, ends roughly by seven thirty, maximum by eight. The huddle format utilizes the best practice of three point agenda: Look Back, Look Ahead and Follow up.
The birth of Huddle in St Luke’s can be traced back with the crafting of the 2013 Vision and Mission. The thrust of the CEO and President was anchored in the Five Imperatives of an Academic Medical Center. One of the imperatives is Upgrading Operating Model that is adopting a multidisciplinary approach. This essentially a characteristic of an Organizational Huddles. The tailor fitting of operating model is to support its value proposition in a competitive environment. The organizational huddles is likewise anchored in the Key Result Areas of the Medical Center, which includes: Process Efficiency, Great Patient Experience and People Empowerment. Organizational Huddle as practice in health care industry, is a senior leader initiated and applies an Open, Transparent, Objective leadership style. Similarly in SLMC, one of its core values is people empowerment which is exemplified in a leadership style that is open, objective and transparent.
St. Luke’s Medical Center (SLMC) enjoys the distinction of being the country’s top healthcare facility, the first accredited Philippine hospital by the Joint Commission International Accreditation (JCIA) and one of the world’s best hospitals. It was clear that in order to improve the hospital’s operational efficiency and in repsonse to the strategic thrust of the President and CEO, change was inevitable. SLMC-Global City realized that it had to enhance its operations in order to achieve competitive advantage by capitalizing on its greatest asset – its people. The ultimate desire to provide great patient experience was likewise anchored in the adoption of the huddle.
SLMC huddles: best practices adoption
The link of patient experience and communication has been established from the studies mentioned earlier. There are two communication models that have served as a foundational basis of the emerging model. The first model is REDE Model. This is a conceptual paradigm that was used in evaluating relationship centered communication. It considers the power of relationships in establishing effective communication. There are three phases of the Relationship: The first is Establishing Relationship through the creation of a climate conducive to the development of trust. Trust is achieved through openness in communication. The second phase which Development is centered again on Trust. This time, Trust is developed by conveying value and respect. Establishment requires enhancement of the therapeutic nature of a relationship by increasing further openness. Engagement is achieved through collaborative planning.
The other model in communication that serves a basis for the development of the emerging model is DCI: Daily Check In for Safety. The model is a focused reporting and conversation among leaders. It is a real time risk assessment. A practice that requires consistency, if leaders does not concern himself with details, subordinates will likewise do the same. A 15-30 minutes meeting with leaders and managers of the organization using a three point agenda. Looking back from the last 24 hours regarding issues and safety is the first agenda in the meeting. In SLMC, this is operationalized with the reporting of House Managers about reported issues from the afternoon and night shifts. Reporting follows a standardized template of Situation, Background, Analysis and Resolution or Recommendation or the SBAR. When issues are unresolved, a follow up is required. The follow up is similar to the Third point agenda, where it is reported in the Huddle the following day. The Second Point Agenda, Looking Ahead is anticipation of possible issues related to safety and quality care. Reporting of Multidisciplinary Monitored Patients provides managers of anticipated care and possible related issues that may be borne from the care to be provided.
Shared Situational Awareness as a feature of DCI, enables the leader to be proactive. In the meeting, it becomes an opportunity for the leader to think and speak on how to resolve the issue. It is like closing the blunt and sharp ends disconnect which is happening in many organization. Leaders lose sight of realities and challenges at the frontline. While workers at the sharp end, feels that risks becomes normalized and actions have high consequences of failure. As situation is being shared and brought to awareness, it prevents disconnect. In SLMC, at the beginning of the day, leaders are made aware of the issues in other areas of the hospital, making it a shared knowledge of how it was resolved and prevent it from happening again.
The DCI Model is a Forum for Heightened Risk Awareness. When risks are talked about, attention is given to managing behaviors or actions and processes to prevent recurrence. In SLMC, the sharing of issues and concerns increases risk awareness and therefore it becomes a way of life.
In the model, the leader analyzes events of harm and determine causes and corrective actions to prevent recurrence. The model promotes questioning attitude about existing issues and the evolving conditions that threaten safe and quality outcomes. This model likewise, improves credibility of the leader as staff realizes and feels confident that issues are being addressed. DCI model also focuses on understanding the structures in a system and how these structures guide the actions and interactions of people who work in the system. Recognition of interconnectedness between and among structures and people is fundamental in the ability to prevent, detect and correct problems. Sharing of ideas and resources becomes evident.
Another feature of DCI Model is Ownership. This is considered as the hallmark of accountability. Being the hall mark, the need to be transparent is likewise crucial. It suggests that the leader must be open, to eventualities in operations. In the past, event reporting lived on paper, now leaders have to own the event that happen under their nose and on their watch.
The DCI communication model as a best practice in organizational huddle, does not just happen. It requires evolution. It requires the leaders to shift paradigm: A Risk Averse Mind set (leaders have to perceive the situation and look for risks and the Risk Averse Action (what leaders say and do to promote and influence individual and team behaviors). In SLMC, we believe that all the principles of DCI are worth adopting and therefore a fertile ground for evidence based management practice.
REDE as a conceptual model, advocates for a work environment that fosters development of trust. As the Relationship grows, where trust becomes operational, Information flows freely. The openness in the relationship creates a climate conducive to transformation. Establishment as a phase in the model requires enhancement of the therapeutic nature of a relationship by increasing transparency, a manifestation likewise of transformation. Engagement is achieved through collaborative planning which makes it informative. In SLMC, the leadership, believes in the same way. To communicate is to inform and transform, a unique feature of core value of innovationin St Luke’s. Likewise, Patient Experience in SLMC is innovative. The of belief of application of better solutions that meet new requirements and unarticulated needs.
The other best practice and evidence of the model, is its generalizability in variety of context, whether clinical or administrative areas. Relationship, Establishment, Development and Engagement can be applied where communication tools are used to be able create a relationship.
DCI model is a 15 minute meeting of the senior leaders with all department leaders of the organization. It occurs in the morning, seven days a week. This practice enables the leader to be proactive. In the meeting, it becomes an opportunity for the leader to think and speak on how to resolve an issue. The three point agenda becomes the pivot. Looking back, looking ahead and Follow up makes the model status oriented. In SLMC, the organizational huddle was initiated in 2013, with the end view of capturing issues and concerns at an earlier stage to prevent it from being raised as a formal complaint. As the huddle forms part of the daily safety check, it also had utilized a reporting mechanism that captures issues from the last 24 hours. Issues reported are utilizing the SBAR framework, managers discusses the issue, analyzes possible root causes, identify and recommend solutions. Anticipating possible issues to occur, managers from the functional units are also reporting multidisciplinary monitored patients for special procedures and therapeutic regimens, that is our version of looking ahead from the three point agenda of DIC Model. Follow up, in our case happens when an issue has not been resolved. Multidisciplinary team addresses it, making the huddle process status oriented and team work driven.
One of the loop holes of the REDE model being a conceptual paradigm that requires testing of its applicability. Empirical Testing of the assumptions of the model will ensure that this model can improve communication and therefore addresses issues and concerns. Testing may take some time. The model would likewise require consistency of communication skills which may hamper creativity and innovations. The DCI model’s loop holes which may appear also as a challenge includes: a requirement for consistency and therefore resistance to everyday and everyone in a meeting has to be addressed. The leader must emphasize the role that every leader plays in problem solving and in learning from the problems experienced by others. The model being a safety driven model, requires focus. The leader course correct unrelated issues when it happens during the 15 minutes meeting. Lastly, the lack of evaluation standards as to impact on organizational performance is one identified loop holes. The leaders need to deliver overall performance excellence, and that makes it difficult to measure given the complexity of issues in health care.
SLMC daily collaborative huddle
Guided by research findings that show the benefits of huddle implementation, SLMC-Global City embraced the huddle process in April 2013. The Head for Operations spearheaded a 30-minute daily collaborative meeting or huddle. Members of the huddle are senior managers from frontline functional groups.
The Daily Collaborative Meeting or Huddle adopted the Three Point Agenda of Daily Check In Model. The House Managers, reports issues and concerns reported by the unit from past 24 hours. The reporting of the issues follows the SBAR framework of communication. The issue or concern reported should be resolved within the day. In the event that the group agreed that an issue is not yet solved, the concerned unit conducts further investigation to report findings and resolution the next collaborative meeting. In the DCI Model, it is called the Follow up. The looking ahead is the report on MMP. The list is read focusing on anticipated procedures and therapeutic regimens. This enables the senior managers to be prompted, anticipation of safety related issues borne out of the procedure, making frontline staff situationally aware.
SLMC daily collaborative huddle: data driven, risk aversion
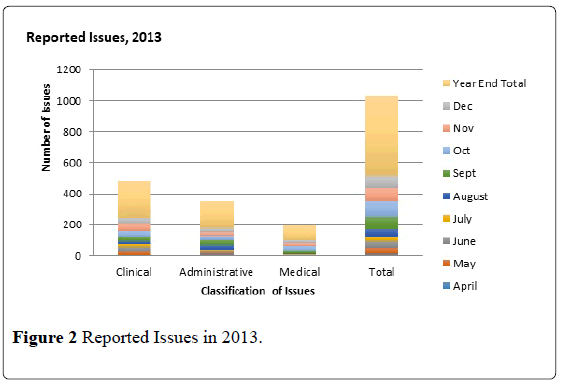
When we started the huddle in 2013, it teaches us to record, track and monitor reported issues. These issues are reported and captured by the units. The reporting likewise taught us the value of blame free environment as our staff are encouraged to self-report, critically analyze situation and empowered to resolve issues. In 2013, there was a daily average of two issues being discussed during the huddle, excluding the issues on falls (slips and trips), needle stick injuries or sharp object injuries and spills (blood and chemicals). September, October and November were the months with most number of raised concerns, with a daily average of three issues. Only 11 concerns were recorded in April because the collaborative meetings started toward the end of April. The months of May, June and July had the least number of issues with a daily average of one concern 9 (Figure 2).
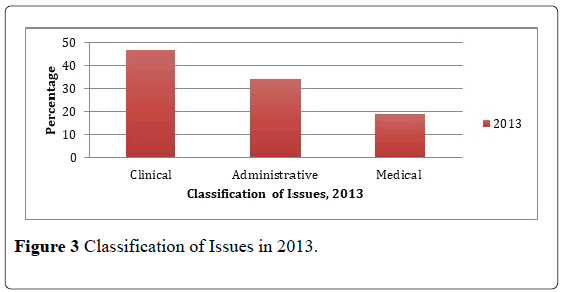
It is also important to note that majority of the attendees of the daily collaborative meetings were from Clinical Operations Groups, thus a greater number of reported incidents were "clinical" in nature – with 243 reported concerns out of 518 (Figure 3).
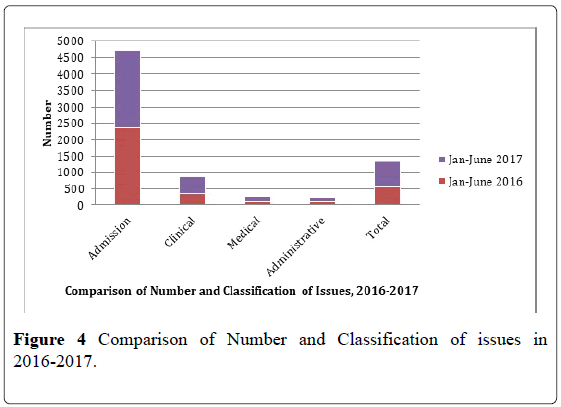
Based on these data gathered from April to December 2013, concerns that were related to clinical issues were the highest with 243 or 46.82 percent. Administrative-related issues followed with 176 or 33.91 percent. Ninetynine concerns (19.27 percent) that were medical in nature were the last in the list (Figure 4).
Issues discussed in the huddle from April to December 2013 revealed that policies, procedures and practices where the most issues are coming from, are either deviation or non compliance, with 224 concerns. A total of 96 issues on facilities/equipment was raised, while concerns on associates’ exchange of information had 76. There were 55 issues on activities in line with day to day operations and 40 concerns about costs that included fees and charging of procedures, while manpower-related issues had recorded a total of 27 concerns.
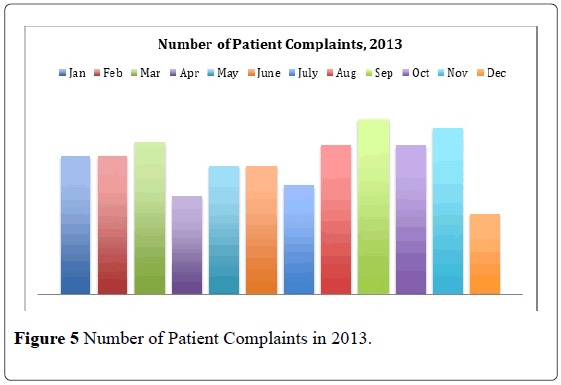
As reporting of issues becomes open, transparent and objective, issues and complaints were noted to have likewise increase in 2013. The data suggests that there might under reporting. However, there was no clear indication that it is directly correlated at that time (Figure 5).
As the huddle becomes part of the daily operations, there were identified pains and setbacks. The so called conception of the huddle as a strategic alignment with the direction of the Medical Center demonstrated some resistance during the labor process. As the huddle progresses, members were adamant on multidisciplinary meeting for finding multidisciplinary solution. As of now, our struggle is an engagement with our physician partners.
As the Huddle becomes part of the daily routine of frontline managers and senior leaders, it likewise has it’s joy and celebration for small successes. As the Huddle gains it stance, just like a toddler, remember SLMC GC was born in 2010, our huddle process was like a small child gaining its grounds. Some of the success huddle had from the perspective of the members were: Huddle forms part of the daily routine of all attendees. This makes them more receptive to situations occurring in the unit, department and the hospital as a whole. A characteristic necessary for competitive health care environment. Aside from the situational awareness that was developed among attendees, they felt that they empowered to bring forth concerns and propose solutions to it. This in greater scheme fostered teamwork. Employees understood the roles they play within the organization. The introduction of “huddles” enhanced the team approach to patient care.
Where are we now?
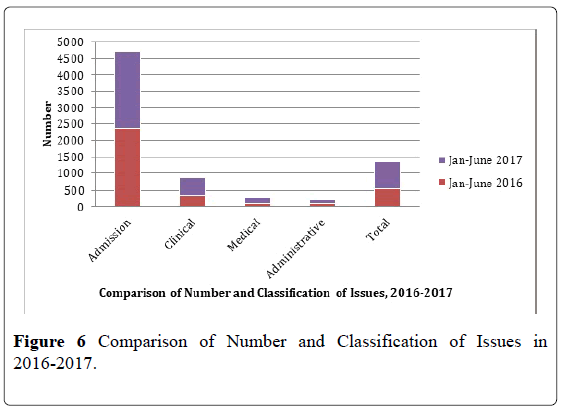
The huddle process had taught SLMC good utilization of data. Comparison of the number and classification of issues from 2016 and 2017 Jan to June revealed that with increasing admission, at the growth rate of 100.1% reported issues in the collaborative meeting also had increased considerably. A 32.62% was noted. This suggests that as issues are being presented, discussed and solved, the escalation to formal complaints are reduced. As this becomes a learning experience, the more issues are openly discussed and solutions are offered the more the process becomes efficient (Figure 6).
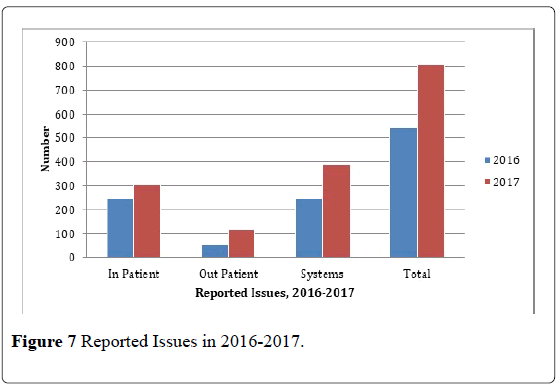
This data likewise shows that in and out patient issues were consistently increasing from the data of 2016 and 2017. The data suggests that issues raised by associates including our physicians and patients are signs of openness. The leader’s non punitive behavior makes associates freely report captured issues and concerns at the unit level. Most of the issues identified and reported are systems in nature making it more critical in the pursuit for operational efficiency towards provision of excellent patient experience. A 32.62% increase in the total reported issues is a such manifestation (Figure 7).
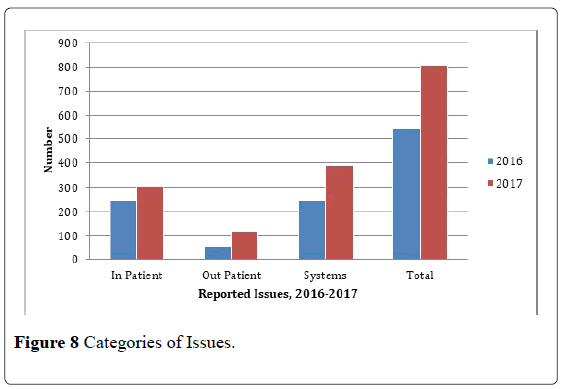
Corroborating the findings as to system issues being reported in the huddle, types of issues as to process was consistently recorded in the 2016 and 2017 data. Process issues were related to hospital guidelines, policies and procedures. Communication issues had also consistently been in the list of most common issues being reported. These issues are related to exchange of patient information within the Medical Center. The consistency suggests that the issues are both patient and associate or employee interaction centered and reaction driven. This means that the process that are deviated in the discharge of function will have a corresponding reaction from the recipient of care. Such deviation is a cause and effect interaction. Cost being the third highest in the reported issues are related to charging concerns and collection of fees which may also be related to communication and process (Figure 8).
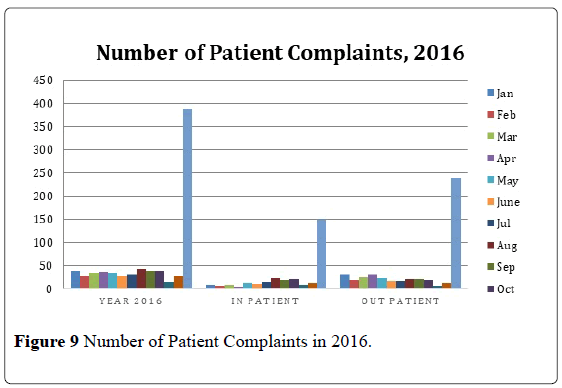
As the culture of no blame becomes evident in the huddle process, with the hallmark incorporation of relationship in the process, where Trust, Openness and Transparency are operational, the number of complaints from issues and concerns raised during the morning collaborative meetings both in the inpatient and outpatient settings, there was a decrease of 67.4% from the 2013 data. This considerable decline in the patient complaints proves that the Huddle is abating issues to be full blown patient complaints (Figure 9).
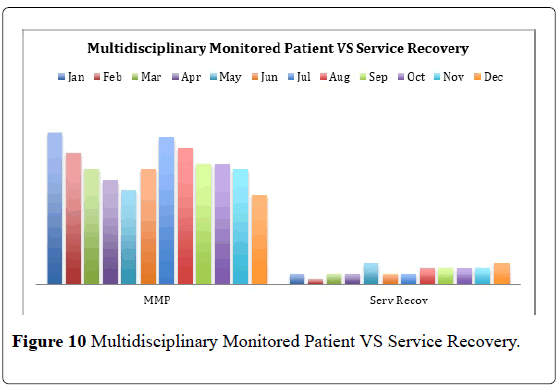
Corroborating the finding is the increasing number of MMP and a decreasing Service Recovery from these specially monitored patients. A ratio of 4:1 was noted (Figure 10).
The need to provide great patient experience, the Medical Center embarked to a third party external benchmarking. The move was to ensure that data on patient satisfaction and their experience being handled and collated by a third party and comparison made from the best hospitals around the globe. Our subscription to Press Ganey was last July of this year. Our performance are commendable. It shows that we are doing well as to satisfying our patients and providing them with great patient experience.
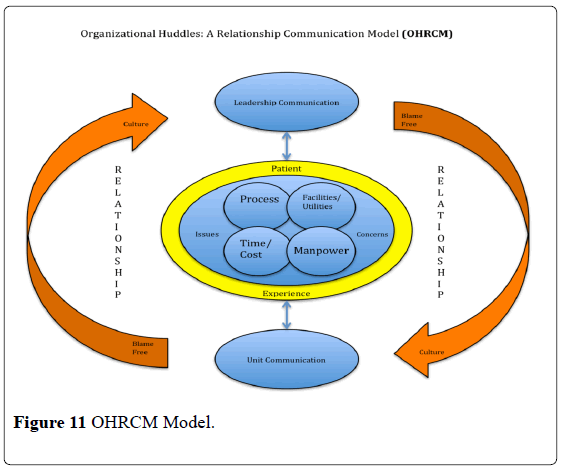
OHRCM: the emerging model
As our Daily Collaborative Meetings taught us many lessons of best practices, an emerging model is being proposed. The model is dubbed as OHRCM. The claim of its usefulness is only true in St Luke’s. The model fosters RELATIONSHIPS both at the leadership and unit levels. The relationship is premised on no blame culture and therefore it fosters Trust, Transparency and Openness. To be able to establish relationship, the leaders and managers must reflectively listen to issues and concerns surrounding patient care and their experience. When this is achieved, the team can now collaboratively plan the actions needed to address issues and concerns of patients, enabling us to provide great patient experience (Figure 11).
OHRCM assumptions: The model has several assumptions. Huddle is relationship based. It considers the power of relationships in establishing effective communication. There are three phases of the Relationship: The first is Establishing Relationship through the creation of a climate conducive to the development of trust. Trust is achieved through openness in communication. The second phase which Development is centered again on Trust. This time, Trust is developed by conveying value and respect. Establishment requires enhancement of the therapeutic nature of a relationship by increasing further openness. Engagement is achieved through collaborative planning. This involves establishing relationship. In doing so the leadership must listen reflectively. In this manner the leader creates a supportive and safe atmosphere of information sharing. This resonates to No Blame Culture. In order to do that, the leader must foster trust and Collaboration. Personal connection is further enhanced when plan to address the issue is collaboratively developed.
OHRCM assumptions: The model has several assumptions. Huddle is relationship based. It considers the power of relationships in establishing effective communication. There are three phases of the Relationship: The first is Establishing Relationship through the creation of a climate conducive to the development of trust. Trust is achieved through openness in communication. The second phase which Development is centered again on Trust. This time, Trust is developed by conveying value and respect. Establishment requires enhancement of the therapeutic nature of a relationship by increasing further openness. Engagement is achieved through collaborative planning. This involves establishing relationship. In doing so the leadership must listen reflectively. In this manner the leader creates a supportive and safe atmosphere of information sharing. This resonates to No Blame Culture. In order to do that, the leader must foster trust and Collaboration. Personal connection is further enhanced when plan to address the issue is collaboratively developed.
Huddle is Leadership and Cross Unit Communication. The assumption that relationship is crucial in the huddle process and the means to the establishment of the relationship is by fostering: trust, which becomes the foundation of relationship, the development of blame free culture is also established in the forged relationship. The means to it is exemplified in openness and transparency of the leaders; and lastly, the model is geared towards professional heterogeneity. The huddle becomes the avenue of teamwork and collaboration. The means to the establishment of the relationship is by fostering: trust, which becomes the foundation of relationship, the development of blame free culture is also established in the forged relationship. The means to it is exemplified in openness and transparency of the leaders. The model is likewise premised towards professional heterogeneity. The huddle becomes the avenue of teamwork and collaboration. Cross Unit Communication is simply mirroring the Leadership Communication. As leaders in the huddle shares the issues and concerns in their respective units, the Manager is guided with the same principles of OHRCM, no blame culture, collaboration and teamwork.
Lastly, Huddle is patient experience focused: As issues and concerns are shared and the situational awareness of the managers are heightened, resolution of issues and concerns is the primordial responsibility of all.
OHRCM and patient experience link: Learning from the experience in huddle, the model can now be link to patient experience. The connect can be further brought at patient level. The connection is with the use of a structured communication tool that can be used by all associate. The HEART is to listen, reflectively listen to issues and concerns, when one is able to actively listens he can empathize and it heightened once awareness of the patient’s situation. When needed to apologize for deficiencies, one is likewise able to situationally be aware. To apologize for the deficiency of others when issues are raised is a manifestation of No Blame Culture developed through the Trust and Transparency in sharing information. Responding is arresting the issue at the unit level and preventing it from escalating to formal complaints. This model is patient experience as it is focused in the resolution of issues and concerns.
Huddle as a management communication model can be applied in health care, as the meeting being short, issue focused, multidisciplinary it may foster productivity. As a relationship driven, the model can foster collaboration among teams. As the huddle becomes patient experience centered, members of the huddle become situationally aware.
The emerging communication model taught us valuable lessons of information sharing. This means that relationship must first be established. This can be done by fostering: trust, which becomes the foundation of relationship, Trust is achieved through openness in communication. The second phase which Development is centered again on Trust. This time, Trust is developed by conveying value and respect. Establishment requires enhancement of the therapeutic nature of a relationship by increasing further openness. Engagement is achieved through collaborative planning.
Huddle is shared situational awareness, early identification and resolution of Problems. Once relationship is established, members of the huddle becomes pre-occupied with early detection and resolution of issues and concerns. The huddle becomes the avenue of sharing, where team work is developed and enhanced.
Conclusion
This how we do huddle in SLMC, customized as to the needs of our patients. Because at SLMC, the needs of our patients come first. As we present the emerging model of communication, we are anticipating for opportunities of growth and its application makes us happy in sharing it.
The lessons it taught us, opens more opportunities for strengthen partnerships and active involvement of our physician partnerships in our daily huddle. The testing of the model likewise is a rich area for data analysis, this time in big and group huddle.
REFERENCES
- Joint Commission on Accreditation of Healthcare Organizations. The Joint Commission guide to improving staff communication. Oakbrook Terrace, IL: Joint Commission Resources 2005.
- Denise MK, John PF, David JG. Improving the patient experience through provider communication skills building. Patient Experience Journal: 2014;1.
- Reason J. Human error: models and management. British Medical Journal 2000;320:768-70.
- Parasuraman A, Zeithaml VA, Berry LL. SERVQUAL: a multiple item scale for measuring, consumer perceptions of service quality. Journal of Retailing 1988;64:12-40.
- Wofford MM, Wofford JL, Bothra J, et al. Patient complaints about physician behaviors: a qualitative study. Acad Med 2004;79:134-138.
- Chang ACS, Read J. The Effects of Listening Support on the Listening Performance of EFL Learners. TESOL Quarterly 2006;40:375-397.
- Albrecht T, Goldsmith D. Social support, social networks, and health. In: Thompson T, Dorsey A, Miller K, Parrott R, eds. Handbook of Health Communication. Mahwah, NJ: Lawrence Erlbaum Associates Inc; 2003;263-284.