Dens fracture or odontoid bone
Busra Candan1,Onder Tomruk2,Ozcan Yildiz2 and Soner Albay1*
1Departments of Anatomy,Suleyman Demirel University Faculty of Medicine, Isparta, Turkey.
2Departments of Anatomy and Emergency Medicine,Suleyman Demirel University Faculty of Medicine, Isparta, Turkey.
3Suleyman Demirel University Faculty of Medicine, Isparta, Turkey.
- *Corresponding Author:
- Soner ALBAY, MD
Associate Professor, Suleyman Demirel University ,Faculty of Medicine Department of Anatomy Isparta, 32260, Turkey
Tel: +90 246 211 3680
E-mail: soneralbay@yahoo.com
Date of Received: February 26th, 2013
Date of Accepted: October 23rd, 2013
Published Online: May 18th, 2014
© Int J Anat Var (IJAV). 2014; 7: 14–16.
[ft_below_content] =>Keywords
dens axis, odontoid bone, odontoid fracture
Introduction
During the embryological development the axis is formed from the proatlas, the C1 sclerotome and the C2 sclerotome. Failure of the odontoid process (C1 sclerotome) to fuse with the body of the axis (C2 sclerotome), or failure of the apex of the odontoid process (proatlas) to fuse with the main portion of the odontoid process has been advocated. The etiology of os odontoideum remains unsettled; both acquired and congenital mechanisms have been suggested [1].In 1863, separation of the odontoid process from the body of the axis was first described in a postmortem specimen. In 1886, Giacomini coined the term os odontoideum for this condition [2]. This entity is clinically important because a mobile or insufficient dens renders the transverse atlantal ligament ineffective at restraining atlantoaxial motion. Sliding of the atlas on the axis may compress the spinal cord or injure the vertebral arteries. Os odontoideum is a rare lesion, and its pathogenesis has been extensively debated in the literature. Some authors have argued that it is congenital and represents the centrum of atlas. However, most authors believe that it is a result of trauma leading to a chronic non-united fracture of the odontoid process [3]. Patients with this condition may be asymptomatic or they may have neck pain, torticollis, or neurological symptoms that may develop either acutely or chronically from repeated spinal cord injury or involvement of the vertebral artery [4]. Os odontoideum has been noted to have a round or oval shape and a smooth margin. On the radiographs, os odontoideum is marked by a small corticated ossicle separated from the base of the odontoid [1]. In this paper, we present a case of os odontoideum that was diagnosed in a trauma patient.
Case Report
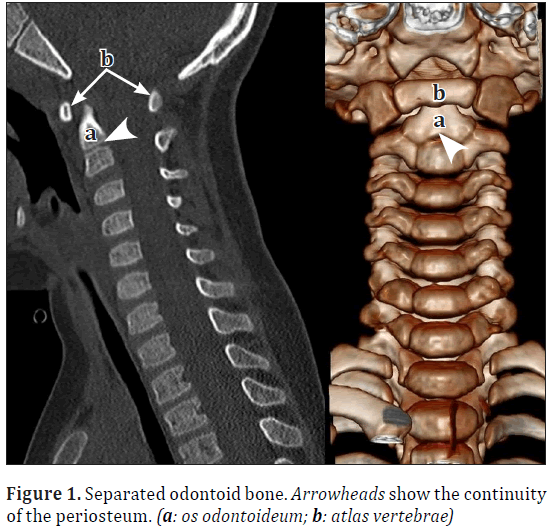
A three-year-old boy presented to the Emergency Department with a fell from 3-meter-high and suspected fractures at lumbar, thoracic and cervical spine and pelvis, face, skull, rib and sternum, in September 2012.But no fractures were identified on CT images (performed on Siemens Somatom Definition AS 128 Slice) and the major diagnostic neurological and clinical examinations were normal. His vital signs demonstrated a normal temperature of 36.3°C, respiratory rate 18 breaths/min, heart rate 136 beats/min, and blood pressure 90/50 mm Hg. On physical examination, he was alert and oriented but agitated. A series of laboratory tests revealed no remarkable findings. Radiographs of the cervical spine showed normal curvature, and no obvious fractures. Due to the severity of his symptoms and signs, CT scan of the cervical spine was performed. The odontoid process was seen to be separate from the body of axis in the CT images. At first glance, this condition was thought to be a fracture but a detailed examination revealed no impairment in the continuity of the periosteum of these two parts. As a result, we concluded that odontoid process was not broken; it was rather a separate bone (Figure 1). CT images revealed a typical odontoid bone with anteriorly displaced atlas on the axis. Patient was informed and conservative treatment was recommended.
Discussion
The tip of the dens and its associated ligaments arise from the fourth occipital through the C0 somites, which do not ossify until middle childhood. The base of the dens is formed from the C0 and C1 sclerotomes as a 2 paired structure that ossifies just prior the birth. The C2 and C3 sclerotomes give rise to the body of the axis, which fuses with the dens at the age of 4 years. The axis has 5 primary and 2 secondary ossification centers. C0, C1, and C2 sclerotomes contribute to various portions of the dens. The principal portion of the dens body arises from the original center of C1. The odontoid process separates from the atlas between the sixth and seventh week of intrauterine life and moves caudally to join the body of the axis [5–6].
Os odontoideum is a developmental variant of the axis in which the odontoid process is divided transversely. The uppermost segment without attachment to the base of the process moves with the anterior arch of the atlas to which it is held by the transverse ligament. The ossicle is small, rounded, and separated from the base of the odontoid by a significant gap [7]. If the ossicle is located where the odontoid tip would normally be, it is said to be orthotopic; if the ossicle is located near the base of the occiput in the region of the foramen magnum, it is termed dystopic. Os odontoideum may be confused with Type 1 or Type 2 odontoid fracture [8].
The classification system by Anderson and D’Alonzoclassifies odontoid fractures based on location on lateral and anteroposterior radiographs. Type I fractures occur through the apical portion of the odontoid process, whereas the more common Type II fractures occur through the base of the dens. Type III fractures occur through the body of the axis with frequent extension into the atlantoaxial facet joints [9].Type III odontoid fractures of the axis are the second most common injuries of the cervical spine. Type III odontoid fractures may occur without major trauma [10].
The aims of surgery in a patient with os odontoideum–as in other spinal pathologies–are stabilization and neural canal decompression when necessary. The preferred surgical stabilization method in the literature is posterior C1-C2 arthrodesis. Two large series by Fielding et al. and later by Spierings and Braakman in the early1980s described both operative and non-operative management strategies for this group of patients [11]. Fielding et al. described 35 patients with os odontoideum. They performed successful C1-C2 posterior arthrodesis [12]. Spierings and Braakman reported a series of 37 patients with os odontoideum [13]. The authors conclude that patients with os odontoideum without C1-C2 instability can be managed without surgical stabilization and fusion with good results [11].
When os odontoideum is suspected, a thorough physical examination is mandatory. This assessment begins with a complete neck and cervical spine examination. Evaluate for tenderness, range of motion and associated anomalies. A careful neurologic examination should include assessment of cerebellum and brainstem function, gait evaluation, and Romberg test. In patients with atlanto-axial instability, upper motor neuron findings are commonly reported and include spasticity, hyperreflexia, clonus, and proprioceptive loss [3].
Conclusion
A rare variant of the second cervical vertebrae, os odontoideum has been reported here. Although it is uncommon, os odontoideum may lead to atlanto-axial instability and spinal cord compression. On the radiographs, os odontoideum is marked by a small corticated ossicle separated from the base of the odontoid. Surgical treatment is usually indicated.
References
- Dai L, Yuan W, Ni B, Jia LS. Os odontoideum: etiology, diagnosis, and management. Surg Neurol. 2000; 53: 106–109.
- Giacomini C. Dell’os-odontoideum Nell’uomo. Gior Acad Med Torino. 1886; 49: 24–28.
- Klimo P Jr, Kan P, Rao G, Apfelbaum R, Brockmeyer D. Os odontoideum: presentation, diagnosis, and treatment in a series of 78 patients. J Neuro surg Spine.2008; 9: 332–342.
- Dunbar HS, Ray BS. Chronic atlanto-axial dislocations with late neurologic manifestations. Surg Gynecol Obstet. 1961; 113:757–762.
- McRae DL. The significance of abnormalities of the cervical spine. AmJRoentgenol (AJR).1960; 84: 3–25.
- Shaffrey CI, Chenelle AG, Abel MF, Menezes AH, Wiggins GC. Anatomy and physiology of congenital spinal lesions. In: Benzel EC, ed. Spine surgery: Techniques, complication avoidance, and management. 2nd Ed., Amsterdam, Elsevier. 2005; 61–87.
- Fielding JW. Disappearance of the central portion of the odontoid process. A case report. J Bone Joint Surg Am. 1965; 47: 1228–1230.
- Whitecloud TSIII, Brinker MR. Congenital anomalies of the base of the skull and the atlanto-axial joint. In: Camins MB, O’Leary PF, eds. Disorders of the cervical spine. Baltimore, Williams and Wilkins. 1992; 199–211.
- Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. 1974. J Bone Joint Surg Am. 2004; 86-A: 2081.
- Panczykowski D, Nemecek AN, Selden NR. Traumatic TypeIII odontoid fracture and severe rotator atlantoaxial subluxation in a 3-year-oldchild: case report. J NeurosurgPediatr. 2010; 5: 200–203.
- Kaya RA,Turkmenoglu O, Cavusoglu H, Kahyaoglu O, Aydin Y. Os odontoideum: case report. Turk Neurosurg. 2005; 15: 157–161.
- Fielding JW, Hensinger RN, Hawkins RJ. Os odontoideum. J Bone Joint Surg Am. 1980; 62: 376–383.
- Spierings EL, Braakman R. The management of os odontoideum: Analysis of 37 cases. J Bone Joint Surg Br. 1982; 64: 422–428.
Busra Candan1,Onder Tomruk2,Ozcan Yildiz2 and Soner Albay1*
1Departments of Anatomy,Suleyman Demirel University Faculty of Medicine, Isparta, Turkey.
2Departments of Anatomy and Emergency Medicine,Suleyman Demirel University Faculty of Medicine, Isparta, Turkey.
3Suleyman Demirel University Faculty of Medicine, Isparta, Turkey.
- *Corresponding Author:
- Soner ALBAY, MD
Associate Professor, Suleyman Demirel University ,Faculty of Medicine Department of Anatomy Isparta, 32260, Turkey
Tel: +90 246 211 3680
E-mail: soneralbay@yahoo.com
Date of Received: February 26th, 2013
Date of Accepted: October 23rd, 2013
Published Online: May 18th, 2014
© Int J Anat Var (IJAV). 2014; 7: 14–16.
Abstract
In this report, the authors describe a case of a 3-year-old boy with odontoid bone diagnosed after trauma. The patient presented with pain following a fall from 3 meters height. Cervical CT images revealed an odontoid bone. The odontoid bone and body of axis had continuous intact periosteum. The regional anatomy and etiology of os odontoideum are discussed here.
-Keywords
dens axis, odontoid bone, odontoid fracture
Introduction
During the embryological development the axis is formed from the proatlas, the C1 sclerotome and the C2 sclerotome. Failure of the odontoid process (C1 sclerotome) to fuse with the body of the axis (C2 sclerotome), or failure of the apex of the odontoid process (proatlas) to fuse with the main portion of the odontoid process has been advocated. The etiology of os odontoideum remains unsettled; both acquired and congenital mechanisms have been suggested [1].In 1863, separation of the odontoid process from the body of the axis was first described in a postmortem specimen. In 1886, Giacomini coined the term os odontoideum for this condition [2]. This entity is clinically important because a mobile or insufficient dens renders the transverse atlantal ligament ineffective at restraining atlantoaxial motion. Sliding of the atlas on the axis may compress the spinal cord or injure the vertebral arteries. Os odontoideum is a rare lesion, and its pathogenesis has been extensively debated in the literature. Some authors have argued that it is congenital and represents the centrum of atlas. However, most authors believe that it is a result of trauma leading to a chronic non-united fracture of the odontoid process [3]. Patients with this condition may be asymptomatic or they may have neck pain, torticollis, or neurological symptoms that may develop either acutely or chronically from repeated spinal cord injury or involvement of the vertebral artery [4]. Os odontoideum has been noted to have a round or oval shape and a smooth margin. On the radiographs, os odontoideum is marked by a small corticated ossicle separated from the base of the odontoid [1]. In this paper, we present a case of os odontoideum that was diagnosed in a trauma patient.
Case Report
A three-year-old boy presented to the Emergency Department with a fell from 3-meter-high and suspected fractures at lumbar, thoracic and cervical spine and pelvis, face, skull, rib and sternum, in September 2012.But no fractures were identified on CT images (performed on Siemens Somatom Definition AS 128 Slice) and the major diagnostic neurological and clinical examinations were normal. His vital signs demonstrated a normal temperature of 36.3°C, respiratory rate 18 breaths/min, heart rate 136 beats/min, and blood pressure 90/50 mm Hg. On physical examination, he was alert and oriented but agitated. A series of laboratory tests revealed no remarkable findings. Radiographs of the cervical spine showed normal curvature, and no obvious fractures. Due to the severity of his symptoms and signs, CT scan of the cervical spine was performed. The odontoid process was seen to be separate from the body of axis in the CT images. At first glance, this condition was thought to be a fracture but a detailed examination revealed no impairment in the continuity of the periosteum of these two parts. As a result, we concluded that odontoid process was not broken; it was rather a separate bone (Figure 1). CT images revealed a typical odontoid bone with anteriorly displaced atlas on the axis. Patient was informed and conservative treatment was recommended.
Discussion
The tip of the dens and its associated ligaments arise from the fourth occipital through the C0 somites, which do not ossify until middle childhood. The base of the dens is formed from the C0 and C1 sclerotomes as a 2 paired structure that ossifies just prior the birth. The C2 and C3 sclerotomes give rise to the body of the axis, which fuses with the dens at the age of 4 years. The axis has 5 primary and 2 secondary ossification centers. C0, C1, and C2 sclerotomes contribute to various portions of the dens. The principal portion of the dens body arises from the original center of C1. The odontoid process separates from the atlas between the sixth and seventh week of intrauterine life and moves caudally to join the body of the axis [5–6].
Os odontoideum is a developmental variant of the axis in which the odontoid process is divided transversely. The uppermost segment without attachment to the base of the process moves with the anterior arch of the atlas to which it is held by the transverse ligament. The ossicle is small, rounded, and separated from the base of the odontoid by a significant gap [7]. If the ossicle is located where the odontoid tip would normally be, it is said to be orthotopic; if the ossicle is located near the base of the occiput in the region of the foramen magnum, it is termed dystopic. Os odontoideum may be confused with Type 1 or Type 2 odontoid fracture [8].
The classification system by Anderson and D’Alonzoclassifies odontoid fractures based on location on lateral and anteroposterior radiographs. Type I fractures occur through the apical portion of the odontoid process, whereas the more common Type II fractures occur through the base of the dens. Type III fractures occur through the body of the axis with frequent extension into the atlantoaxial facet joints [9].Type III odontoid fractures of the axis are the second most common injuries of the cervical spine. Type III odontoid fractures may occur without major trauma [10].
The aims of surgery in a patient with os odontoideum–as in other spinal pathologies–are stabilization and neural canal decompression when necessary. The preferred surgical stabilization method in the literature is posterior C1-C2 arthrodesis. Two large series by Fielding et al. and later by Spierings and Braakman in the early1980s described both operative and non-operative management strategies for this group of patients [11]. Fielding et al. described 35 patients with os odontoideum. They performed successful C1-C2 posterior arthrodesis [12]. Spierings and Braakman reported a series of 37 patients with os odontoideum [13]. The authors conclude that patients with os odontoideum without C1-C2 instability can be managed without surgical stabilization and fusion with good results [11].
When os odontoideum is suspected, a thorough physical examination is mandatory. This assessment begins with a complete neck and cervical spine examination. Evaluate for tenderness, range of motion and associated anomalies. A careful neurologic examination should include assessment of cerebellum and brainstem function, gait evaluation, and Romberg test. In patients with atlanto-axial instability, upper motor neuron findings are commonly reported and include spasticity, hyperreflexia, clonus, and proprioceptive loss [3].
Conclusion
A rare variant of the second cervical vertebrae, os odontoideum has been reported here. Although it is uncommon, os odontoideum may lead to atlanto-axial instability and spinal cord compression. On the radiographs, os odontoideum is marked by a small corticated ossicle separated from the base of the odontoid. Surgical treatment is usually indicated.
References
- Dai L, Yuan W, Ni B, Jia LS. Os odontoideum: etiology, diagnosis, and management. Surg Neurol. 2000; 53: 106–109.
- Giacomini C. Dell’os-odontoideum Nell’uomo. Gior Acad Med Torino. 1886; 49: 24–28.
- Klimo P Jr, Kan P, Rao G, Apfelbaum R, Brockmeyer D. Os odontoideum: presentation, diagnosis, and treatment in a series of 78 patients. J Neuro surg Spine.2008; 9: 332–342.
- Dunbar HS, Ray BS. Chronic atlanto-axial dislocations with late neurologic manifestations. Surg Gynecol Obstet. 1961; 113:757–762.
- McRae DL. The significance of abnormalities of the cervical spine. AmJRoentgenol (AJR).1960; 84: 3–25.
- Shaffrey CI, Chenelle AG, Abel MF, Menezes AH, Wiggins GC. Anatomy and physiology of congenital spinal lesions. In: Benzel EC, ed. Spine surgery: Techniques, complication avoidance, and management. 2nd Ed., Amsterdam, Elsevier. 2005; 61–87.
- Fielding JW. Disappearance of the central portion of the odontoid process. A case report. J Bone Joint Surg Am. 1965; 47: 1228–1230.
- Whitecloud TSIII, Brinker MR. Congenital anomalies of the base of the skull and the atlanto-axial joint. In: Camins MB, O’Leary PF, eds. Disorders of the cervical spine. Baltimore, Williams and Wilkins. 1992; 199–211.
- Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. 1974. J Bone Joint Surg Am. 2004; 86-A: 2081.
- Panczykowski D, Nemecek AN, Selden NR. Traumatic TypeIII odontoid fracture and severe rotator atlantoaxial subluxation in a 3-year-oldchild: case report. J NeurosurgPediatr. 2010; 5: 200–203.
- Kaya RA,Turkmenoglu O, Cavusoglu H, Kahyaoglu O, Aydin Y. Os odontoideum: case report. Turk Neurosurg. 2005; 15: 157–161.
- Fielding JW, Hensinger RN, Hawkins RJ. Os odontoideum. J Bone Joint Surg Am. 1980; 62: 376–383.
- Spierings EL, Braakman R. The management of os odontoideum: Analysis of 37 cases. J Bone Joint Surg Br. 1982; 64: 422–428.