Desisting from gender dysphoria after 1.5 years of puberty suppression
Received: 24-May-2022, Manuscript No. PULJCAP-22-4817; Editor assigned: 28-May-2022, Pre QC No. PULJCAP-22-4817(PQ); Accepted Date: Jul 01, 2022; Reviewed: 03-Jun-2022 QC No. PULJCAP-22-4817(Q); Revised: 10-Jun-2022, Manuscript No. PULJCAP-22-4817(R); Published: 05-Jul-2022, DOI: 10.37532/puljcap.2022.6(4)-30-34
Citation: Rolver A, Focker M, Romer G. Desisting from gender dysphoriaafter 1.5 years of puberty suppression. J Child Adolesc Psychiatr.2022; 6(4):30-34.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Over the last decade medical care for transgender youth has improved. Gonadotropin-Releasing-Hormone-Analogues (GnRHa) stop and delay puberty and can relieve the distress of Gender Dysphoria (GD). Only a few adolescents treated with GnRHa desist from GD, thus systematic and in-depth investigations are missing.
Case Presentation: A case of peri pubertal onset gender dysphoria (12.4 years) is presented. It illustrates the desistance from GD after a 15-month-treatment with GnRHa. The blocking of puberty lead to a reduction of GD, the process of gender identity development still continued, leading to a non-binary outcome.
Conclusion: This case report illustrates that after treatment with puberty blockers desistance from gender dysphoria can occur. Further, GnRHa do not “the ongoing process of gender identity formation in psychosexual development. Thus, puberty suppression is a reversible treatment option that can be seen as a meaningful step to prepare the readiness for partially irreversible gender-affirming hormone treatment.
Key Words
Gender Dysphoria; Gender Incongruence; Gonadotropin-ReleasingHormone-Analogues; Puberty blocking; Gender identity
Introduction
According to ICD-11, Gender Incongruence (GI) refers to the mismatch of an individual`s experienced gender and his or her birth-assigned sex which often leads to a desire to live and be accepted as a person of the experienced gender. If people suffer from gender incongruence or experience impairment in social, school, or other important areas of functioning, Gender Dysphoria (GD) can arise. According to DSM-5 adolescents with GD experience a distressing incongruence between their birth-assigned sex and the gender they identify with [1,2]. The identification with the other gender and experienced GD can be accompanied by the desire to change the sexual characteristics of the physical body and to seek genderaffirming medical treatment (e.g. hormonal treatment, surgery).
Based on systematic reviews of past studies mainly based on utilization rates of specialized medical centers offering sex-reassigning interventions, the average prevalence rate of transgender adults has been estimated at 6.8 of 100.000 persons [3,4]. However, this rate is likely to be biased by underestimation, because individuals with gender incongruence who did not seek medical treatments were not detected as cases. In a recent populationbased epidemiological survey from Sweden gender incongruence in adults was reported by 0.9% of legally males and 1.0% of legally females, whereas a strong desire to seek medical treatment for sex reassignment was reported by 0,2% of the adult population across both sexes. This finding represents a rate about 30 times higher than the average rate estimated from past reviews named above. For children and adolescents, epidemiological studies are missing. In a New Zealandian study, 1.2% of a sample of high school students identified as transgender [5,6].
Over the last decades, medical care for transgender youth has changed including an increase in specialized health services. These clinics register an increasing demand accompanied by a shift in the gender-sex ratio towards natal females [7]. Adolescents with GD often face various associated social, emotional, and behavioral difficulties. The most prevalent associated problems of gender dysphoric adolescents are bullying, depression, suicide attempts, and self-harm. Thus, GD is often associated with mental disorders, mostly major depression and eating disorders [8-11].
The majority of prepubescent children with GI/GD have been reported not to have an outcome of persistent gender dysphoria after puberty. Concerning sexual preference, the most reported outcome of childhood GD has been (cis-gendered) homosexuality or bisexuality [12-14]. The persistence of GD has most likely been predicted by the intensity of GD in childhood (‘conviction’ vs. ‘wish’) and the amount of reported cross-gendered behaviors. However, despite the likelihood, there is no certain predictor to discriminate between later ‘disasters’ and ‘persisters’ before the onset of puberty. On the other hand, GD that persists from childhood into adolescence is likely to further persist into adulthood. Dutch longitudinal clinical follow-up studies on adolescents with childhood GD who received puberty suppression and/or gender-affirming hormones after comprehensive biopsychosocial assessment demonstrated that none of the participants desisted from gender-affirming surgery one year later. Some adolescents have not experienced childhood GD, thus any predictions about stability are harder to make. Furthermore, there is a growing number of adolescents who identify as non-binary. Given the various developmental pathways for children with GD and the dynamic nature of gender identity in adolescence an individualized approach in clinical care has to be taken [15-19].
Best clinical practice for child and adolescent GI/GD
According to international standards of care, clinicians should explore gender identity openly and exploratively. The treatment strategy focuses on constant and supportive counseling of children and parents, helping to create a safe and accepting environment for children and adolescents where they can unfold their gender identity. The affirmative approach encourages children and adolescents to transition to the gender role that fits with their subjective identity. This includes for adolescents the option of medical interventions to facilitate gradual and age-appropriate developmental transitions, particularly the option of endocrine treatment, both by suppressing puberty and by subsequent gender-affirming hormone treatment. Medical treatment options should be offered to patients step by step after careful clinical assessments and re-assessments. Puberty suppression is a fully reversible intervention that can be seen as an important step to preparing the readiness for gender-affirming hormone treatment both in the gender dysphoric adolescent and his or her social environment. It can also be helpful in cases when further time is needed for an adolescent with GD to explore his or her gender identity. A shared decision-making process for the treatment options is recommended, clinicians should evaluate the adolescent’s capacity for consent, helping the adolescent to reach the required capabilities for informed consent [20-24]
It has been acknowledged in international standards of care that particularly in adolescent GD ‘just waiting’ cannot be considered a neutral option because it can create additional harm due to ongoing and irreversible sexual maturation. The German Ethical Council has stated in 2020 that in individuals with GD after the onset of puberty the potential consequences of active medical interventions (e.g. puberty blocking) have to be carefully weighed against the potential consequences of not intervening. Clinicians have to carefully consider potential health benefits and risks of both medical intervention and not (yet) intervening by balanced reasoning in any individual case.
Puberty suppression with Gonadotropin-Releasing-Hormone-Analogues (GnRHa)
Current international treatment guidelines recommend GnRHa as an option to attenuate the distress of GD by reducing the suffering caused by the development of secondary sexual characteristics in puberty. The temporary halting of pubertal maturation relieves distress caused by masculinizing or feminizing body changes (e.g. puberty vocal change in Tran’s girls or menstruation in tran’s boys). This offers a limited period of time for gender dysphoric adolescents to reflect their gender identity and for mental health professionals to support self-exploration and reflections on other associated developmental problems. Gender dysphoric adolescents showed improved psychological functioning and better social functioning after temporary puberty suppression. In a recent study, Sorbara and colleagues found that the late pubertal stage in gender dysphoric youth was associated with more mental health problems. Concerning biological maturation, the treatment with GnRHa is fully reversible [25-28].
There is a paucity of studies of patients who detransition after intake of GnRHa. In the study of Brik and colleagues, 5 adolescents (3.5%) did not continue with gender-affirming treatment due to various reasons. The effect on gender identity development was not further explicated. The percentage of discontinuation of GnRHa is small (1.9%-3.5%), thus systematic studies are missing. These studies were conducted in specialized gender clinics which include a comprehensive assessment before medical treatment is started, thus the number of discontinuation can be underestimated. In an opposing position to current international treatment guidelines, some authors argued that puberty suppression by itself may increase the likelihood of persistence because gender dysphoric adolescents may be alienated from the chance to “reconcile” with their “original” gender by gradually adjusting to their sexually maturing bodies. A qualitative study by vrouenrats and colleagues [29-33] found that there is a lively debate about the pros and cons of puberty suppression among mental health professionals working in GD treatment teams which shows that there a still open question concerning the use GNRHa and gap between guidelines and the current practice.
The above-mentioned opposing position was endorsed by a recent public debate concerning a decision of the High Court of Justice in England and Wales in 2020 which had ruled that minors under 16 would not be competent to give legal consent to the administration of GnRHa because they were not able to oversee the long-term consequences of this treatment. This court had further ruled that puberty blockers should only be applied between the age of 16 and 18 with the permission of a Family Court. Meanwhile, this court decision has been overruled by the British Court of Appeal, which clarified that decisions for or against endocrine treatment options in gender dysphoric minors should fully stay within the responsibility of physicians given that there is valid informed consent by patients and if applicable - their legal caregivers. In clinical practice, a shared and fully informed co-consent of gender-dysphoric minors and their legal caregivers is recommended both for legal and psychological reasons [34]. This informed co-consent is to be developed together with health professionals in a careful process of shared decision making.
Case Presentation
In 2017, CS (12;4 years) was seen for the first time in our specialized gender outpatient service. See figure 1 for the timeline of episode of care.
Being female by birth-assigned sex, he introduced himself as a boy and reported gender dysphoric feelings which had started six months ago as well as the desire to live in the male gender role. Follow-up appointments together with his parents were made on a low-frequency basis (every two months) to jointly explore the course of these recent onset complaints. After 9 months of clinical observation, the diagnosis of GD was given according to DSM 5 criteria. In October 2017 CS completed his female-to-male social transition in all important areas of everyday life. In January 2018 he additionally started high-frequent psychotherapy with weekly sessions with a psychotherapist. He suffered from conflicts with his parents and started to injure himself. In March 2018, after 12 months of clinical observation and after his completed social transition, treatment with GnRHa was started based on child-parent coconsent to halt female maturation from which CS was suffering enormously. In November 2019 (age 15) the attending psychotherapist recommended an inpatient admission for more intensive psychotherapy because of the aggravation of CSS depressive symptoms and upcoming doubts about his transgender transition.
At hospital admission CS reported various depressive symptoms: he experienced permanent low mood and most of the time he felt tired and exhausted and had no motivation to engage in things or hobbies he had enjoyed before. He described a feeling of hopelessness and repetitive thoughts mainly about his gender transition.
Along with these ruminating cognitions he had difficulties in making decisions in his daily life and he had withdrawn almost completely from his social life. He reported self-injuring by cutting and scratching himself over already 2,5 years. He experienced suicidal ideations, however, negated suicide attempts or concrete suicidal plans.
Family, development, and social history.
CSS’s parents are married and are working in the field of public administration. He has a younger sister (8 years) with whom he got along well. CS attended secondary school, and in the last year, his grades worsened. Psychological disorders are unknown in family history.
Physical examination and laboratory investigations.
The physical examination showed a good state of health. Their physical appearance was spruce and their body shape was slim (weight 49.5 kg; height 168.5 cm; BMI 17.4 kg/m² [7P, -1.45z, female norms). Laboratory tests were within normal limits, with no somatic or endocrinological diseases.
Psychological tests at admission.
In the Becks Depression Inventory (BDI) CS showed a total score of 22, representing moderate depression at admission [35].
The Eating Disorder Inventory-2 (EDI-2) is standard for the assessment of attitudinal and behavioral dimensions relevant to anorexia and bulimia nervosa. CS had elevated scores (PR >/= 75 < 90) on the subscales body dissatisfaction, ineffectiveness, interpersonal distrust, and maturity fears and clinically relevant sores (PR >/= 90) on the subscales drive for thinness, bulimia, interoceptive awareness, and asceticism.
The Social Phobia and Anxiety Inventory for Children (SPAI-C)[37] is a 26-item self-report instrument that measures a range of potentially anxietyprovoking situations as well as symptoms associated with social phobia. CS showed elevated scores in social interactions and performance situations (PR = 96-99 and t-value= 68-73).
The Life Problems Inventory (LPI) [38] measures borderline features in adolescents. CS showed elevated scores on the subscales identity confusion and emotion dysregulation.
Diagnosis and treatment
At admission, the diagnostic criteria of a major depressive disorder, single episode, moderate (F32.1), and GD (according to DSM 5) were met.
CS was admitted to our psychotherapy ward for adolescents (focus on emotion regulation) and received over 14 weeks of individual psychotherapy sessions (twice a week), family sessions (every second week), music- and art therapy (every week) as well as multiple pedagogical groups and individual interventions focusing on emotional and social competencies. The therapeutic setting was based on dialectical behavior therapy for adolescents [39].
At the beginning of treatment, CS was timid and reluctant and avoided contact with peers. During treatment, he gradually built trust, initiated conversations with the staff and peers, and was liked by them.
During individual psychotherapy sessions, it was easier for CS to open up because of his prior experiences in psychotherapy. Based on a CBT approach, first, behavioral analysis was undertaken and then an individual biopsychosocial model for understanding his depression and gender dysphoria was set up with a focus on the evolvement and maintenance of symptoms. From a biological perspective, CS reported that his menstruation began very early (at 10 years) and that he experienced it as a drastic and overwhelming event. He could not accept that his body was changing; he did not like either his breasts or voice. Furthermore, he reported that he learned in a documentary on television that a low weight can cause amenorrhea which was why he set his weight gain limit up at 50 kg.
From a social perspective, CS reported that at the age of 11 he had a massive conflict with female friends which led to his exclusion from the girls’ peer group. Then he joined a boy’s peer group and felt relieved from the conflict. One year later in the summer vacation of 2016, he started to ruminate extensively and concluded for himself that a boy would not have that kind of social problems and menstruation. After that summer vacation, at the age of 14 and 8, he disclosed his gender problem to his teacher and parents. He cut his hair short and wore loose clothes. In spring 2017, he started transitioning socially and got himself a male name. The social transition was accompanied by a huge relief, resulting in a better mood and motivation. In 2018 he started ruminating about his transition and accused himself of making the wrong decision. The rumination came along with strong feelings of insecurity regarding his further proceeding (beginning of cross-sex hormone treatment or not) and self-hate, which worsened the selfinjury. Further, he began to feel insecure about daily decisions and therefore withdraw from family, and friends, avoidance of activity, and was passive in many life areas.
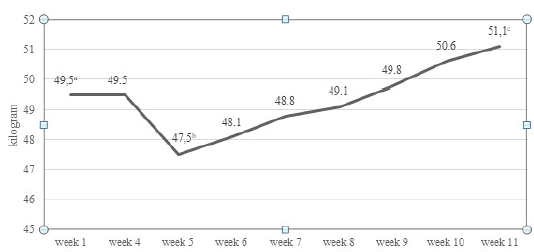
In the inpatient therapeutic milieu, CS was able to talk frankly about the development and maintenance factors of his depressive and gender dysphoric feelings and about his fear of gaining weight and physical maturation. These factors were identified and addressed in therapy. Finally, after a shared decision-making process CS decided to stop puberty suppression which was recommended from a professional perspective. The decision caused CS major distress because he was afraid not to have any control over the physical change of his body, especially the menses. He also feared weight gain and for a short period started restrictive eating and lost weight. The restrictive eating was treated with psychoeducation and an eating protocol. See Figure 2 for the weight curve for treatment from week 1 to week 11.
Throughout therapy, he gained insight into dysfunctional thoughts, emotions, and behaviors. At the end of the treatment, he accepted his femalesex body, identified himself as non-binary, and kept his male name and male pronoun. He did not regret the developmental pathway of the past two years anymore, which he could appreciate as a necessary diversion of finding out about his gender identity. He did not feel easy with his menses but accepted and coped with it without major suffering from it anymore. He continued psychotherapy every week. CSS’s parents supported the treatment, in family therapy sessions CS increasingly opened up to his parents, talking more frankly about his emotional problems and his attempts to cope with them. At hospital discharge, the diagnosis of a mild depressive disorder was still present (F32.0). The diagnosis of GD was changed into sexual maturation disorder (F66.0).
Follow-up– 1.5 years later
At a follow-up assessment, CS reported that in summer 2020 she decided to alter her name and pronouns back to female. She reported that she would define her gender as non-binary. Since hospital discharge she still struggled with her menses, thus she is taking now a gestagen drug to suppress it. CS mentioned that she still had depressive thoughts and behaviors from time to time but could manage her daily life. She could not report her actual weight, however, restrictive eating did not occur anymore. She did not need psychotherapy sessions anymore. Regarding the GnRHa treatment she does not regret anything, she rather sees it as part of her process of finding out her own gender identity. CS’s mother confirmed CS’s statement.
Psychological tests
In the BDI CS showed a total score of 11, representing mild depression [35].
The subscales of the EDI-2 were in the normal range, except for the subscale maturity fears ((PR >/= 90) [36].
CS showed on the SPAI-C no elevated scores in social interactions and performance situations (PR = 26-50 and t-value= 44-50).
Regarding the LPI, all scores were in the normal range for adolescents [38].
Discussion
Systematic studies and in-depth studies on the phenomenon of resistance from GD after the beginning of puberty suppression in adolescence are lacking. Little is known about the psychological processes behind such desisting outcomes. This case report illustrates that after the beginning of treatment with puberty blockers desistance from GD can occur and that gender identity is often more dynamic and less binary than supposed. This supports the hypothesis that the development of gender identity based on ongoing self-exploration and reflection is not „automatically“ impaired or even haltered by suppressing the secretion of sex hormones with GnRHa. Rather psychosexual development including gender identity development can progress despite suppressed sex hormone levels. On the one hand, this case illustrates the potential benefit of puberty suppression as a medically reversible treatment option in cases of GD in early adolescence, in which later resistance may occur despite careful and sufficient clinical assessment before starting this treatment. On the other hand, this case underlines the necessity of careful assessment and profound information of young patients with GD and their parents or legal guardians before starting endocrine treatment. This includes information about the possibility of later resistance, as well as diverse outcomes, in particular not only binary ones. Non-binary gender identity appears to be becoming more common among adolescents presenting at gender clinics [40]. Non-binary youths are highly vulnerable and have important health care needs [19]. For health professionals, it underlines the necessity of careful case monitoring and reassessment after starting treatment with puberty blockers in gender dysphoric youths and before starting partially irreversible interventions, such as gender-affirming hormone treatment.
In the case of CS, the ongoing pubertal maturation with increasing feminizing bodily features led to major distress and psychological symptoms. The gender dysphoric and depressive symptoms decreased under the treatment with puberty blockers, CS felt temporarily relieved. This observation is in line with findings that early medical interventions improve the psychosocial functioning and well-being in gender dysphoric adolescents [40,41]. In the vast majority of cases, in which GD persists into adulthood, the life-long mental health-related gain of preventing irreversible masculine or feminine body features can be considered substantial. However, in CS’s case, a medically caused “irreversible consolidation” of the transgender pathway by the endocrine intervention of administering puberty blockers was not observed. CS could make use of a reflecting “moratorium” with her maturing body to find out that the perspective of masculinization of her body appearance through gender-affirming hormone treatment would be incongruent with her gender identity. CS expressed feelings of doubt, fear, and shame regarding the option of social retransition, however, she was able to reflect on this as coping with her process of gender identity development. In her retrospect the use of GnRHa ‘had bought’ time which enabled her to further explore her gender identity and to critically question her desire for somatic sex-reassigning procedures. Through psychological treatment, it was possible to support CS in her individual decisions. She could develop a perspective in which she did not regret her “transitional transition”, rather seeing it as a coherent process of her gender identity formation. Thus, the conclusion of this case report is in line with the WPATH standards of care which suggest an affirmative treatment approach for GD in adolescents in which medical treatment options should be offered to patients step by step after careful clinical as. However, the ethical dilemma remains in any treatment decisions with gender-diverse youths. Potential long-term consequences of medical interventions in cases of later resistance from GD have to be carefully weighed against potentially harmful consequences of irreversible masculinization or feminization of the bodily appearance on the mental health of gender dysphoric youths. To improve security in treatment decisions, longitudinal follow-up studies on larger cohorts of transgender adolescents treated with GnRHa are needed.
Furthermore, this case reminds us that gender cannot be understood as a binary concept. In the treatment and counseling of children and adolescents with GI or GD gender variety and multiple pathways should be considered. The primary goal of treatment should be to promote a person’s mental health and well-being and not a binary identification as male or female.
Conclusion
To sum up, this case study demonstrates that under the treatment with puberty blockers, desistance from GD in adolescence can occur. It further demonstrates that GnRH analogs, while blocking sex hormone secretion, do not at the same time „block“the ongoing process of gender identity development. This case report supports the standards in current treatment guidelines, in which puberty suppression with GnRHa can be offered as a treatment option for minors with GD after the first stages of puberty (minimum Tanner stage 2) have been reached and if gender-affirming hormone treatment cannot be recommended yet. This treatment should be based on a careful comprehensive assessment as well as fully informed consent by both the young patients and their parents or legal guardian.
References
- Nitsuwat S, Paoin W. Development of ICD-10-TM ontology for a semi-automated morbidity coding system in Thailand. Methods of information in medicine. 2012; 51(06):519-28.
Google scholar Crossref - Carter MJ. Diagnostic and statistical manual of mental disorders. Therapeutic recreation journal.2014; 48(3):275.
Google scholar Crossref - Arcelus J, Bouman WP, Van Den Noortgate W et al. Systematic review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry. 2015;30(6):807-15.Google scholar Crossref
- Collin L, Reisner SL, Tangpricha V et al. Prevalence of transgender depends on the â??caseâ? definition: a systematic review.J Sex Med.2016;13(4):613-26.
Google scholar Crossref - Ã?hs JW, Dhejne C, Magnusson C et al. Proportion of adults in the general population of Stockholm County who want gender-affirming medical treatment. PLoS One.2018;5;13. Google scholar Crossref
- Clark TC, Lucassen MF, Bullen P et al. The health and well-being of transgender high school students: results from the New Zealand adolescent health survey (Youth'12).J Adolesc Health.2014;55(1):93-9.
Google scholar Crossref - Aitken M, Steensma TD, Blanchard R et al. Evidence for an altered sex ratio in clinicâ?referred adolescents with gender dysphoria. The journal of sexual medicine. 2015; 12(3):756-63. Google scholar Crossref
- Becker I, Gjergji-Lama V, Romer G et al. Merkmale von Kindern und Jugendlichen mit Geschlechtsdysphorie in der Hamburger Spezialsprechstunde. Praxis der Kinderpsychologie andKinderpsychiatrie.2014;63(6):486-509. Google scholar Crossref
- De Graaf NM, Cohen-Kettenis PT, Carmichael P et al. Psychological functioning in adolescents referred to specialist gender identity clinics across Europe: a clinical comparison study between four clinics. Eur Child Adolesc Psychiatry. 2018 Jul;27(7):909-19.Google scholar Crossref
- Holt V, Skagerberg E, Dunsford M. Young people with features of gender dysphoria: Demographics and associated difficulties. Clin Child Psych Psychiatry.2016; 21(1):108-18. Google scholar Crossref
- Connolly MD, Zervos MJ, Barone II CJ et al. The mental health of transgender youth: Advances in understanding. J Adolesc Health. 2016;59(5):489-95. Google scholar Crossref
- Ristori J, Steensma TD. Gender dysphoria in childhood. Int Rev Psychiatry. 2016; 28(1):13-20. Google scholar Crossref
- Singh D, Bradley SJ, Zucker KJ. A follow-up study of boys with gender identity disorder. Front psychiatry.2021:287. Google scholar Crossref
- Wallien MS, Cohen-Kettenis PT. Psychosexual outcome of gender-dysphoric children. J Am Acad Child Adolesc Psychiatry.2008 ;47(12):1413-23. Google scholar Crossref
- Drescher J, Byne W. Gender dysphoric/gender variant (GD/GV) children and adolescents: Summarizing what we know and what we have yet to learn. J Homosex.2012;59(3):501-10. Google scholar Crossref
- De Vries AL, McGuire JK, Steensma TD, et al. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics.2014;134(4):696-704. Google scholar Crossref
- De Vries AL, Steensma TD, Doreleijers TA et al. Puberty suppression in adolescents with gender identity disorder: A prospective followâ?up study.J Sexual Med.2011;8(8):2276-83.
Google scholar Crossref - Littman L. Rapid-onset gender dysphoria in adolescents and young adults: A study of parental reports. PloS one. 2018;13(8). Google scholar Crossref
- Chew D, Tollit MA, Poulakis Z et alYouths with a non-binary gender identity: a review of their sociodemographic and clinical profile. Lancet Child Adolesc Health.2020;4(4):322-30.
Google scholar Crossref - Coleman E, Bockting W, Botzer M et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version. Int J Transgenderism.2012;13(4):165-32. Google scholar Crossref
- Romer G, Möller B. Geschlechtsinkongruenz und Geschlechtsdysphorie im Jugendalter.�rztliche Psychotherapie.2020;15(2):87-94.
Google scholar Crossref - Ethikrat D. Trans-Identität bei Kindern und Jugendlichen: Therapeutische Kontroversenâ??ethische Orientierungen. Ad-hoc-Empfehlung. Berlin: Deutscher Ethikrat. 2020. Google scholar
- Hembree WC, Cohen-Kettenis PT, Gooren L et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine society clinical practice guideline. J Clin Endocrinol Metab.2017; 102(11):3869-903. Google scholar Crossref
- De Vries AL, Cohen-Kettenis PT. Clinical management of gender dysphoria in children and adolescents: the Dutch approach. J Homosexual.2012;59(3):301-20.
Google scholar Crossref - Costa R, Carmichael P, Colizzi M. To treat or not to treat: puberty suppression in childhood-onset gender dysphoria.Nat Rev Urol.2016;13(8):456-62.
Google scholar Crossref - Becker-Hebly I, Briken P, Schulte-Markwort M et al.Transgender in Adolescence: State of the Art and Future Research Needs. Psychother Psychosom Med Psychol.2020;8;70(3-04):151-62.
Google scholar Crossref - Van der Miesen AI, Steensma TD, de Vries AL et al. Psychological functioning in transgender adolescents before and after gender-affirmative care compared with cisgender general population peers. J Adolescent Health. 2020;66(6):699-704.
Google scholar Crossref - Sorbara JC, Chiniara LN, Thompson S et al. Mental health and timing of gender-affirming care. Ped.2020;146(4).
Google scholar Crossref - Brik T, Vrouenraets LJ, de Vries MC, Hannema SE. Trajectories of adolescents treated with gonadotropin-releasing hormone analogues for gender dysphoria. Arch Sex Behav.2020;49(7):2611-8.
Google scholar Crossref - Wiepjes CM, Nota NM, de Blok CJ et al. The Amsterdam cohort of gender dysphoria study (1972â??2015): trends in prevalence, treatment, and regrets. J Sex Med. 2018 Apr 1;15(4):582-90.Google scholar
- Korte A, Beier KM, Bosinski HA et al . Behandlung von Geschlechtsidentitätsstörungen (Geschlechtsdysphorie) im Kindes-und Jugendalterâ??Ausgangsoffene psychotherapeutische Begleitung oder frühzeitige Festlegung und Weichenstellung durch Einleitung einer hormonellen Therapie? Sexuologie. 2016;23(3-4):117-32.Google scholar
- Richards C, Maxwell J, McCune N et al. Use of puberty blockers for gender dysphoria: a momentous step in the dark. Arch Dis Child.2019
Google scholar Crossref - Vrouenraets LJ, Fredriks AM, Hannema SE et al. Perceptions of sex, gender, and puberty suppression: A qualitative analysis of transgender youth. Archives of sexual behavior.2016;45(7):1697-703.
Google scholar Crossref - Mahfouda S, Moore JK, Siafarikas A et al. Puberty suppression in transgender children and adolescents. Lancet Diabetes Endocrinol. 2017;5(10):816-26.Google scholar Crossref
- Hautzinger M, Bailer M, Worall H et al. Beck-depressions-inventar (BDI). Bern: Huber. 1994.
Google scholar - Paul T, Thiel A. Eating Disorder Inventory-2 (EDI-2): deutsche Version. Hogref; 2005.
Google scholar - Beidel DC, Turner SM, Morris TL. A new inventory to assess childhood social anxiety and phobia: The Social Phobia and Anxiety Inventory for Children. Psych Assess. 1995;7(1):73. Google scholar Crossref
- Rathus JH, Wagner D, Miller AL et al. Psychometric evaluation of the life problems inventory, a measure of borderline personality features in adolescents. J Psychol Psychother.2015;5(4):1-9.
Google scholar - Von Auer AK, Bohus M et al . Interaktives Skillstraining für Jugendliche mit Problemen der Gefühlsregulation (DBT-A): Das Therapeutenmanual-Akkreditiert vom Deutschen Dachverband DBT. Klett-Cotta;2018.
Google scholar Crossref
- Butler G, De Graaf N, Wren B et al . Assessment and support of children and adolescents with gender dysphoria. Arch Dis Child.2018;103(7):631-36.
Google scholar
- Costa R, Dunsford M, Skagerberg E et al . Psychological support, puberty suppression, and psychosocial functioning in adolescents with gender dysphoria. SexMed; 2015 ;12(11):2206-14
Google scholar Crossref