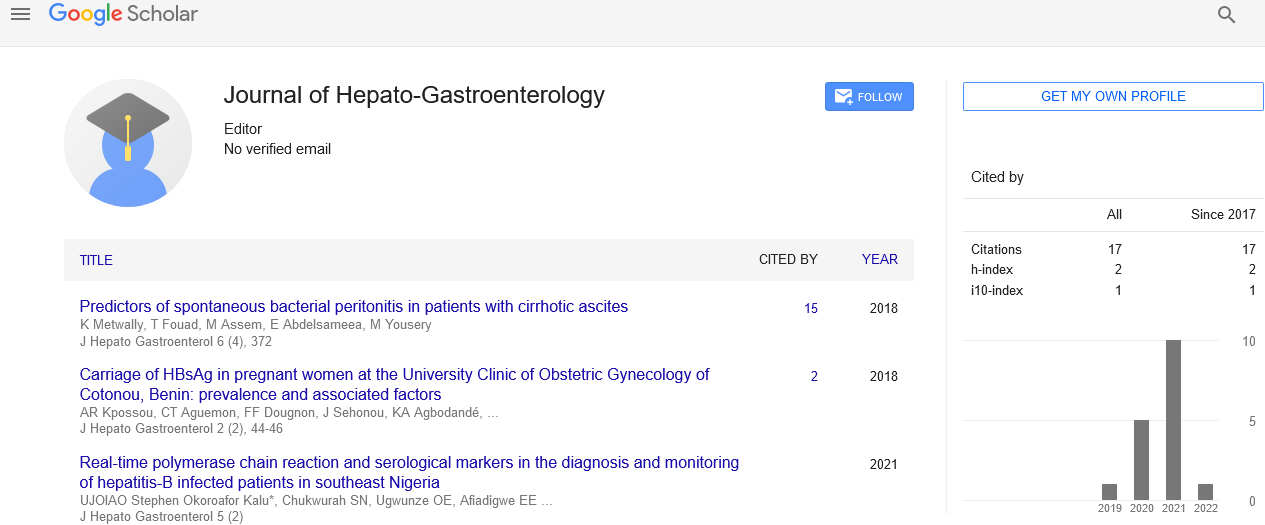
Detailed description on laparoscopic pancreatectomy
Received: 08-Nov-2021 Accepted Date: Nov 22, 2021; Published: 29-Nov-2021
Citation: Wagner D. Detailed description on laparoscopic pancreatectomy. J Hepato Gastroenterol 2021;5(2):9.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Description
Pancreatic surgical operation continues to be related to an incredibly excessive morbidity and mortality as compared with different specialties. This is a result of the complicated nature of the organ, the difficult access because of the retroperitoneal function and the variety of technically difficult anastomoses required. Nevertheless, the past years have witnessed a consistent development in morbidity and a decrease in mortality accomplished through changes of technique (especially referring to the pancreatic anastomoses) collectively with hormonal manipulation to decrease pancreatic secretions. Recently minimally invasive pancreatic surgical operation has been tried with the aid of using several centers round the world which has inspired significant interest on this technique. The majority of the cases tried had been distal pancreatectomies, because of the more trustworthy nature of the resection and the shortage of a pancreatic ductal anastomosis, however more lately reviews of laparoscopic pancreaticoduodenectomy have begun to appear.
Laparoscopic distal pancreatectomy, with or without keeping the spleen, is technically simpler than the Whipple procedure, and is extra widely accepted. Indications for laparoscopic distal pancreatectomy consist of cystic neoplasms and islet-cellular tumors positioned within the pancreatic body or tail. Complications of acute and chronic pancreatitis can be dealt with the usage of surgical laparoscopy. When inflamed necrotizing pancreatitis is found, surgical intervention for drainage and debridement is required. However, the indication to minimally invasive technique for pancreatic surgical operation is regularly benign or low-grade malignant pathologies.
Laparoscopic pancreatic surgical treatment has a few technical barriers for surgeons and tumor identity can be challenging. Image-guided strategies offer intraoperative margin evaluation and visualization methods, which can be high quality in guiding the healthcare professional to acquire healing resections and consequently enhance the surgical outcomes. The application to pancreatic surgical procedure of minimally invasive method has only lately emerged: each Laparoscopic Distal Pancreatectomy (LDP) and Laparoscopic Pancreaticoduodenectomy (LPD) may be adequately performed. LDP and LPD are endorsed to advanced perioperative outcomes, along with reduced blood loss, shorter duration of stay, decreased postoperative pain and expedited time to practical recovery. Despite the apprehensive use and recognition of laparoscopic distal pancreatectomy, numerous case collection and comparative cohort research have cautioned that laparoscopic approaches to distal pancreatic resection offer comparable advantages which have been verified for different minimally invasive procedures.
Conclusion
Pancreatic disorders consist of inflammation (pancreatitis) or the formation of pancreatic cysts or pancreatic cancer. Traditional pancreatic surgical procedure is achieved through an extended incision, and is frequently associated with an extended hospital stay and recovery. Laparoscopic surgery permits certain approaches to be carried out through smaller incisions with much less ache which shortens clinic stay, the chance of a few headaches and a faster recovery. Laparoscopic pancreatic surgery is frequently carried out for tumors or cysts of the left side of the pancreas. Potential dangers of laparoscopic pancreatic surgery are like open surgical treatment and consist of bleeding, infection, damage to surrounding organs and leakage of pancreatic fluid. Indications for pancreatic resection do not vary for laparoscopic or open surgical treatment; whether or not a pancreatic resection may be completed laparoscopically relies upon at the surgeon's training and experience. Laparoscopic pancreatic surgical treatment is related to a significant learning of curve effect, necessitating based introduction with the aid of using skilled surgeons and considerable case volumes according to center.