Difficulty during pulmonary arterial catheterization caused by retrosternal thyroid gland*
Nimet Senoglu1*, Alptekin Yasim2,Hafize Oksuz1, Gokce Gisi1 and Nazan Okur3
1Kahramanmaras Sutcu Imam University, Faculty of Medicine, Department of Anesthesiology and Reanimation,Kahramanmaras, Turkey.
2Cardiovascular Surgery,Kahramanmaras, Turkey.
3Cardiovascular Surgery and Radiology,Kahramanmaras, Turkey.
- *Corresponding Author:
- Nimet Senoglu, MD
Assistant Professor of Anesthesiology, Kahramanmaras Sutcu Imam University, Faculty of Medicine, Department of Anesthesiology and Reanimation, 46050 Kahramanmaras,Turkey.
Tel: +90 344 2212337
Fax: +90 344 2212371
E-mail: nimetsenoglu@hotmail.com
Date of Received: December 3rd, 2008
Date of Accepted: March 19th, 2009
Published Online: March 24th, 2009
© IJAV. 2009; 2: 38–40.
[ft_below_content] =>Keywords
retrosternal thyroid,pulmonary arterial catheterizationd,central catheterization
Introduction
Catheterization of the central vein is commonly attempted to obtain central venous access for hemodynamic monitoring, management and administration of fluids in some surgical procedures [1]. Pulmonary arterial catheterization (PAC) is a central catheterization technique and an important part of the management of cardiac surgical procedures, accepted for treating patients with shock states. Complications from PAC may be classified into 2 main categories: technical problems and misinterpretation of data. The technical complications are difficulties of establishing central venous access, complications of the catheterization procedure, and complications of the catheter residence [2]. Complications that result from patient characteristics, for example anatomical variations, are important factors to experience difficulty in central venous access. Principally, after the insertion of central venous catheters, chest radiographs are obtained to ensure correct positioning of the catheter tip in the superior vena cava and to exclude mechanical complications, such as pneumothorax. The presented case had a big retrosternal thyroidal mass, which led to anatomical variations in main vascular structures, and caused difficulty in central venous access and PAC.
Case Report
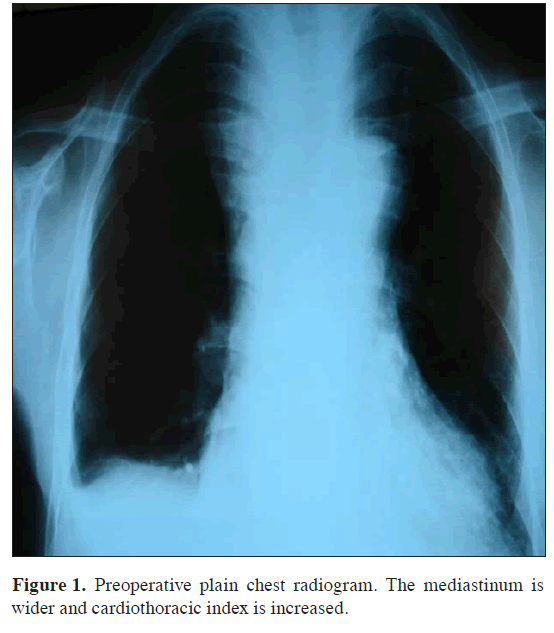
Sixty-three years old male patient admitted to the operation room for coronary by-pass surgery. During the physical examination a big thyroidal mass was noticed. Thyroidal function tests were euthyroid in laboratory analysis, and ejection fraction was 35% in echocardiography. Mediastinum and cardiac shadow were increased in the plain chest radiograph (Figure 1).
After the induction of anesthesia, pulmonary arterial catheterization was attempted, so that the right internal jugular and subclavian venipuncture were tried. Venous puncture was succeeded but guide-wire could not be advanced. The ‘introducer’ needle (18-G, 6-3 cm) freely aspirated, it was thought to be venous blood. The ‘J’ tip of the guide wire (0.81mm_60cm) was inserted, but failed to advance. The guide wire was removed and reinserted, but again failed to advance. The needle and guide wire were then removed and digital pressure was applied to the site.
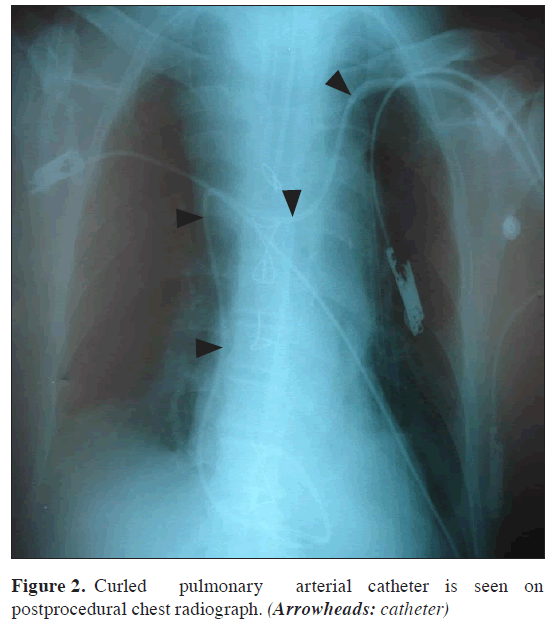
After then, left subclavian vein was punctured and catheter could be inserted via this route. During the progression of the catheter, controlled by the pressure curves, it was difficult to pull it forward or backward. Then the procedure was stopped and a radiological examination was performed. In the plain chest radiograph, the catheter was seen as curled around the upper mediastinum (Figure 2).
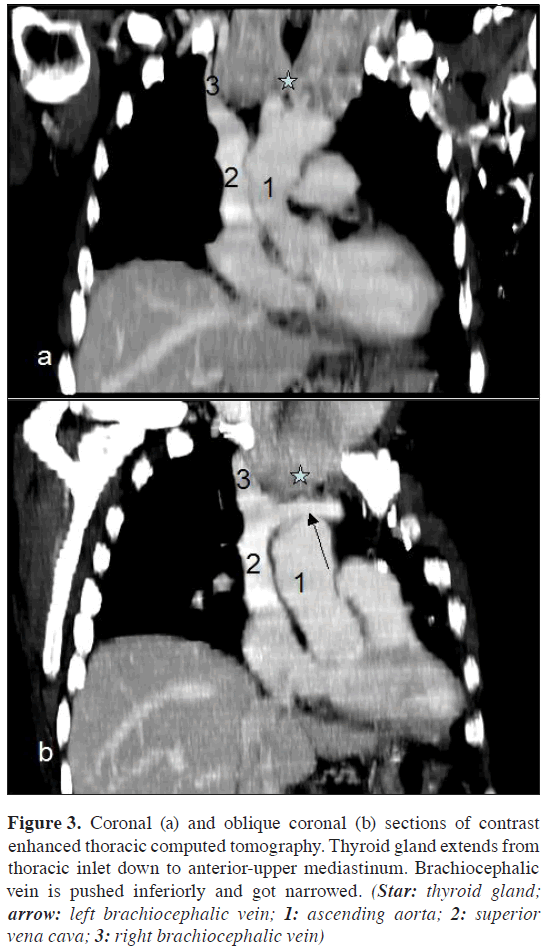
Figure 3: Coronal (a) and oblique coronal (b) sections of contrast enhanced thoracic computed tomography. Thyroid gland extends from thoracic inlet down to anterior-upper mediastinum. Brachiocephalic vein is pushed inferiorly and got narrowed. (Star: thyroid gland; arrow: left brachiocephalic vein; 1: ascending aorta; 2: superior vena cava; 3: right brachiocephalic vein)
Postprocedure contrast enhanced thoracic computed tomography revealed a multinodular goiter, which reached the retrosternal space, and bilaterally pushed and narrowed the brachiocephalic veins (Figure 3).
Discussion
Pulmonary artery catheterization has been accepted worldwide for treating critical patients in shock states. It produces precise measurements under some technical limitations, makes the diagnosis easier, provides a better evaluation of grade, and reduces the doubts of the intensive care provider [2]. It is first incorporated into clinical practice in 1970, allows for direct measurement of pressures in the right atrium, right ventricula, pulmonary arteria and allows more accurate determinations of volume status and cardiac performance than cardiac venous pressure alone. It provides a large amount of information on cardiovascular physiology, usually inserted via the superior vena cava into the right atrium following cannulation of either the internal jugular or subclavian vein [3].
The anatomical landmark method for catheterization of pulmonary arteria via central venous access remains but anatomical variations make the landmark method less reliable. It is reported that use of two-dimensional real-time ultrasound during internal jugular vein access is associated with better success, lower complication rate, and faster access [4,5].
This case clearly shows how a retrosternal thyroid may grossly alter the blood vessels caliber and their anatomical relationships, may lead to difficulty in internal jugular and/or pulmonary arterial catheterization. Ultrasound-guided insertion of a central line is a helpful technique for venous access in such cases; avoiding complications that can be serious, even fatal. The use of ultrasound in this patient would have revealed the anomalous of both jugular veins and the reduced caliber of the left (making it almost impossible to cannulate), and would have prevented arterial puncture [6]. Also, in case of any doubt about the correct position of a central catheter, a chest radiograph should be obtained after the procedure [7]. In our case, we have seen that thyroidal hyperplasia was the reason for difficulty in central cannulation andlocalization PAC, especially in retrosternal cases. To our opinion, it is important to know that retrosternal thyroid can cause to displacement of main vascular structures and lead to difficulties central catheter insertion. Chest radiography and thoracic computed tomography are helpful methods to detect such cases.
References
- Sznajder JI, Zveibil FR, Bitterman H, Weiner P, Bursztein S. Central vein catheterization. Failure and complication rates by three percutaneous approaches. Arch Intern Med. 1986; 146: 259–261.
- Lopes MC, de Cleva R, Zilberstein B, Gama-Rodrigues JJ. Pulmonary artery catheter complications: report on a case of a knot accident and literature review. Rev Hosp Clin Fac Med Sao Paulo. 2004; 59: 77–85.
- McGee WT, Mailloux P, Jodka P, Thomas J. The pulmonary artery catheter in critical care. Semin Dial. 2006; 19: 480–491.
- Jensen MO. Anatomical basis of central venous catheter fracture. Clin Anat. 2008; 21: 106–110.
- Eisen LA, Narasimhan M, Berger JS, Mayo PH, Rosen MJ, Schneider RF. Mechanical complications of central venous catheters. J Intensive Care Med. 2006; 21: 40–46.
- Karakitsos D, Labropoulos N, De Groot E, Patrianakos AP, Kouraklis G, Poularas J, Samonis G, Tsoutsos DA, Konstadoulakis MM, Karabinis A. Real-time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006; 10: R162.
- Gladwin MT, Slonim A, Landucci DL, Gutierrez DC, Cunnion RE. Cannulation of the internal jugular vein: is postprocedural chest radiography always necessary? Crit Care Med. 1999; 27: 1819–1823.
Nimet Senoglu1*, Alptekin Yasim2,Hafize Oksuz1, Gokce Gisi1 and Nazan Okur3
1Kahramanmaras Sutcu Imam University, Faculty of Medicine, Department of Anesthesiology and Reanimation,Kahramanmaras, Turkey.
2Cardiovascular Surgery,Kahramanmaras, Turkey.
3Cardiovascular Surgery and Radiology,Kahramanmaras, Turkey.
- *Corresponding Author:
- Nimet Senoglu, MD
Assistant Professor of Anesthesiology, Kahramanmaras Sutcu Imam University, Faculty of Medicine, Department of Anesthesiology and Reanimation, 46050 Kahramanmaras,Turkey.
Tel: +90 344 2212337
Fax: +90 344 2212371
E-mail: nimetsenoglu@hotmail.com
Date of Received: December 3rd, 2008
Date of Accepted: March 19th, 2009
Published Online: March 24th, 2009
© IJAV. 2009; 2: 38–40.
Abstract
In this report, we present a case of large retrosternal thyroid mass causing difficulty in pulmonary arterial catheterization. It is emphasized that retrosternal thyroid can cause variation of major vascular structures and difficulty in central catheterization techniques. Imaging modalities like plain chest radiography and thoracic computerized tomography are important to display such cases.
-Keywords
retrosternal thyroid,pulmonary arterial catheterizationd,central catheterization
Introduction
Catheterization of the central vein is commonly attempted to obtain central venous access for hemodynamic monitoring, management and administration of fluids in some surgical procedures [1]. Pulmonary arterial catheterization (PAC) is a central catheterization technique and an important part of the management of cardiac surgical procedures, accepted for treating patients with shock states. Complications from PAC may be classified into 2 main categories: technical problems and misinterpretation of data. The technical complications are difficulties of establishing central venous access, complications of the catheterization procedure, and complications of the catheter residence [2]. Complications that result from patient characteristics, for example anatomical variations, are important factors to experience difficulty in central venous access. Principally, after the insertion of central venous catheters, chest radiographs are obtained to ensure correct positioning of the catheter tip in the superior vena cava and to exclude mechanical complications, such as pneumothorax. The presented case had a big retrosternal thyroidal mass, which led to anatomical variations in main vascular structures, and caused difficulty in central venous access and PAC.
Case Report
Sixty-three years old male patient admitted to the operation room for coronary by-pass surgery. During the physical examination a big thyroidal mass was noticed. Thyroidal function tests were euthyroid in laboratory analysis, and ejection fraction was 35% in echocardiography. Mediastinum and cardiac shadow were increased in the plain chest radiograph (Figure 1).
After the induction of anesthesia, pulmonary arterial catheterization was attempted, so that the right internal jugular and subclavian venipuncture were tried. Venous puncture was succeeded but guide-wire could not be advanced. The ‘introducer’ needle (18-G, 6-3 cm) freely aspirated, it was thought to be venous blood. The ‘J’ tip of the guide wire (0.81mm_60cm) was inserted, but failed to advance. The guide wire was removed and reinserted, but again failed to advance. The needle and guide wire were then removed and digital pressure was applied to the site.
After then, left subclavian vein was punctured and catheter could be inserted via this route. During the progression of the catheter, controlled by the pressure curves, it was difficult to pull it forward or backward. Then the procedure was stopped and a radiological examination was performed. In the plain chest radiograph, the catheter was seen as curled around the upper mediastinum (Figure 2).
Figure 3: Coronal (a) and oblique coronal (b) sections of contrast enhanced thoracic computed tomography. Thyroid gland extends from thoracic inlet down to anterior-upper mediastinum. Brachiocephalic vein is pushed inferiorly and got narrowed. (Star: thyroid gland; arrow: left brachiocephalic vein; 1: ascending aorta; 2: superior vena cava; 3: right brachiocephalic vein)
Postprocedure contrast enhanced thoracic computed tomography revealed a multinodular goiter, which reached the retrosternal space, and bilaterally pushed and narrowed the brachiocephalic veins (Figure 3).
Discussion
Pulmonary artery catheterization has been accepted worldwide for treating critical patients in shock states. It produces precise measurements under some technical limitations, makes the diagnosis easier, provides a better evaluation of grade, and reduces the doubts of the intensive care provider [2]. It is first incorporated into clinical practice in 1970, allows for direct measurement of pressures in the right atrium, right ventricula, pulmonary arteria and allows more accurate determinations of volume status and cardiac performance than cardiac venous pressure alone. It provides a large amount of information on cardiovascular physiology, usually inserted via the superior vena cava into the right atrium following cannulation of either the internal jugular or subclavian vein [3].
The anatomical landmark method for catheterization of pulmonary arteria via central venous access remains but anatomical variations make the landmark method less reliable. It is reported that use of two-dimensional real-time ultrasound during internal jugular vein access is associated with better success, lower complication rate, and faster access [4,5].
This case clearly shows how a retrosternal thyroid may grossly alter the blood vessels caliber and their anatomical relationships, may lead to difficulty in internal jugular and/or pulmonary arterial catheterization. Ultrasound-guided insertion of a central line is a helpful technique for venous access in such cases; avoiding complications that can be serious, even fatal. The use of ultrasound in this patient would have revealed the anomalous of both jugular veins and the reduced caliber of the left (making it almost impossible to cannulate), and would have prevented arterial puncture [6]. Also, in case of any doubt about the correct position of a central catheter, a chest radiograph should be obtained after the procedure [7]. In our case, we have seen that thyroidal hyperplasia was the reason for difficulty in central cannulation andlocalization PAC, especially in retrosternal cases. To our opinion, it is important to know that retrosternal thyroid can cause to displacement of main vascular structures and lead to difficulties central catheter insertion. Chest radiography and thoracic computed tomography are helpful methods to detect such cases.
References
- Sznajder JI, Zveibil FR, Bitterman H, Weiner P, Bursztein S. Central vein catheterization. Failure and complication rates by three percutaneous approaches. Arch Intern Med. 1986; 146: 259–261.
- Lopes MC, de Cleva R, Zilberstein B, Gama-Rodrigues JJ. Pulmonary artery catheter complications: report on a case of a knot accident and literature review. Rev Hosp Clin Fac Med Sao Paulo. 2004; 59: 77–85.
- McGee WT, Mailloux P, Jodka P, Thomas J. The pulmonary artery catheter in critical care. Semin Dial. 2006; 19: 480–491.
- Jensen MO. Anatomical basis of central venous catheter fracture. Clin Anat. 2008; 21: 106–110.
- Eisen LA, Narasimhan M, Berger JS, Mayo PH, Rosen MJ, Schneider RF. Mechanical complications of central venous catheters. J Intensive Care Med. 2006; 21: 40–46.
- Karakitsos D, Labropoulos N, De Groot E, Patrianakos AP, Kouraklis G, Poularas J, Samonis G, Tsoutsos DA, Konstadoulakis MM, Karabinis A. Real-time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006; 10: R162.
- Gladwin MT, Slonim A, Landucci DL, Gutierrez DC, Cunnion RE. Cannulation of the internal jugular vein: is postprocedural chest radiography always necessary? Crit Care Med. 1999; 27: 1819–1823.