Dissection of spinalis capitis and implications for osteopathic treatment
2 Lake Erie College of Osteopathic Medicine, Erie, Pennsylvania, USA
3 Department of Osteopathic Principles and Practices, Lake Erie College of Osteopathic Medicine, Erie, Pennsylvania, USA
Received: 03-Oct-2017 Accepted Date: Oct 21, 2017; Published: 28-Oct-2017
Citation: Labranche L, Quinette J, Hendryx JT, et al. Dissection of spinalis capitis and implications for osteopathic treatment. Int J Anat Var. 2017;10(4):73-4.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The spinalis cervicis and capitis muscles are small components of the erector spinae group. These muscles are highly variable, and when present, they are typically asymmetric and often fused with other muscles. Herein, we provide a description of our dissection of a well-developed and unilateral discrete spinalis capitis muscle. This muscle arose from the ligamentum nuchae and attached superiorly along the inferiorly nuchal line. While this muscle is infrequent, it is positioned to cause unique patterns of somatic dysfunction and may play a role in the development of cervical and/or occipital headaches. Such a muscle should therefore be of unique interest to osteopathic physicians.
Keywords
Spinalis capitis; Anatomical variation; Cervical myology; Cervical somatic dysfunction; Cervicogenic headache
Introduction
A thorough understanding of the structure and function of back musculature is of particular significance to osteopathic physicians, as somatic dysfunction of these muscles may lead to back pain and irregular movement of the vertebral column. Although infrequently identified, the spinalis cervicis and capitis muscles are minor components of the erector spinae muscle group but have the potential to cause unique patterns of somatic dysfunction. We describe herein the presence of a unilateral spinalis capitis muscle, identified during cadaveric dissection, and potential implications of this finding. The Erector Spinae (ES) muscles are a major component of the deep or intrinsic back muscles and functionally serve as the chief extensors and side benders of the vertebral column. The ES group consists of three long, vertical muscular columns: Iliocostalis, longissimus, and spinalis (lateral to medial, respectively). All three erector spinae muscles arise from a common inferior attachment at the iliac crest, posterior sacrum, sacroiliac joints, supraspinous ligament, and inferior lumbar spinous processes. From this common attachment, the ES group can be divided based on their superior attachments. The spinalis muscle column is subdivided into three regional components: spinalis thoracis, spinalis cervicis, and spinalis capitis. Spinalis thoracis is typically the most developed, consisting of fascicles that insert segmentally onto thoracic spinous processes. Alternatively, spinalis cervicis and spinalis capitis are described as irregularly and poorly developed. When present, spinalis cervicis arises from the inferior portion of the ligamentum nuchae and spinous process of CV7, and attaches superiorly to the spinous processes of the upper cervical vertebrae. Spinalis capitis is not well characterized in modern anatomy textbooks and atlases, and is often omitted from anatomical illustration [1-4]. However, it can be identified as fibers that extend from the spinous processes of TV1 and CV7 to the cranium, often blending with semispinalis capitis [1].
In a case study involving 142 cadavers, spinalis capitis was absent in the majority of the sample population. When present, this muscle typically blended with the semispinalis capitis muscle. Only three unilateral examples of a distinct spinalis capitis were found, with the proximal attachment being either the ligamentum nuchae or spinous processes of CV6-TV2, and distal attachment being the occiput [2]. Additionally, Martin reported a case of a unilateral muscle that appeared to be closest to the description of spinalis capitis, although its attachments did not match any existing descriptions of spinalis capitis. The described muscle extended from the spinous and left transverse processes of CV6, to the occiput, with weak fascial attachments to the ligamentum nuchae. At CV2, the muscle bifurcated over semispinalis cervicis. In addition, the spinous processes of CV3-6 appeared to be shifted to the right [5].
Regardless, the spinalis capitis muscle appears to be frequently absent or when it is present, it is poorly developed and fused/incorporated into other muscle bellies. Furthermore, when spinalis capitis is found as a distinct muscle, it most often is unilateral. Based on these observations, we suggest that the presence and dysfunction of this muscle may lead to unique physical exam findings and may be of particular interest to osteopathic physicians. The purpose of the present study is to discuss the identification of a rare cervical muscle, and its potential clinical significance.
Case Report
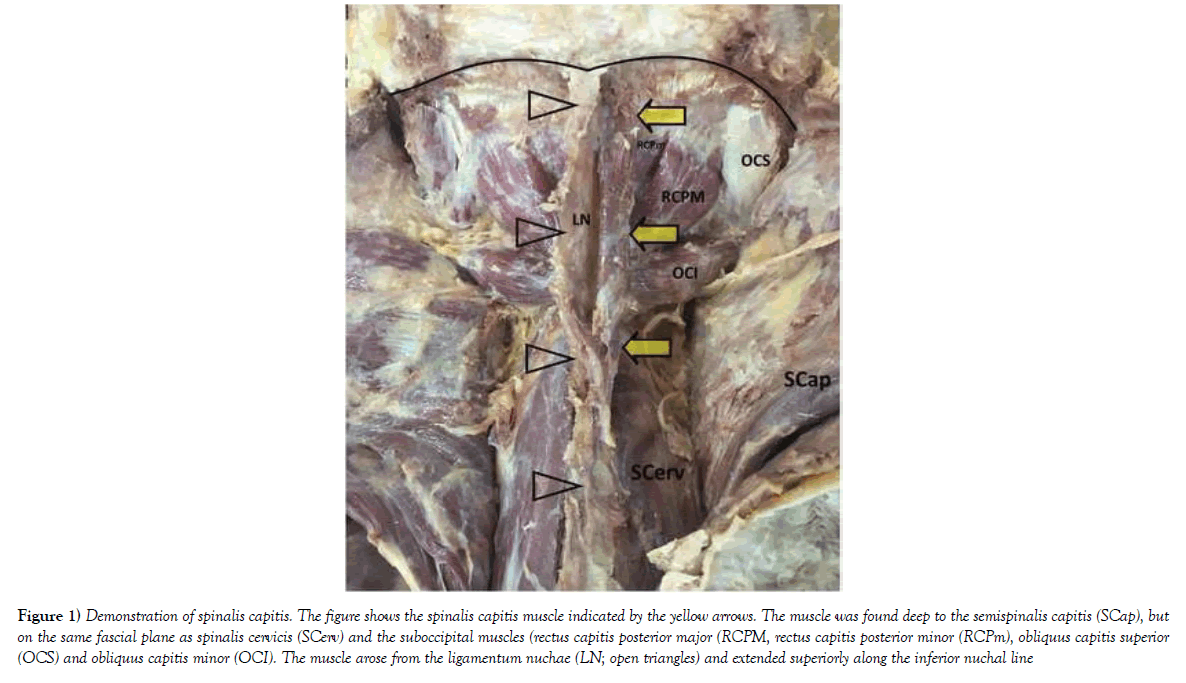
During routine dissection of the back and posterior neck of a 63-year-old male anatomical donor, superficial back and cervical musculature was identified and reflected. Deep to semispinalis capitis, we observed a discrete muscle arising from the right side of the ligamentum nuchae at the level of CV3/4, and attaching unilaterally to the occiput just superficial to rectus capitis posterior minor at the inferior nuchal line (Figure 1). This muscle was well developed, distinct from the right semispinalis capitis, and enclosed in cervical fascia. Although these findings are incongruous with classical descriptions, this muscle appears most consistent with spinalis capitis.
Figure 1) Demonstration of spinalis capitis. The figure shows the spinalis capitis muscle indicated by the yellow arrows. The muscle was found deep to the semispinalis capitis (SCap), but on the same fascial plane as spinalis cervicis (SCerv) and the suboccipital muscles (rectus capitis posterior major (RCPM, rectus capitis posterior minor (RCPm), obliquus capitis superior (OCS) and obliquus capitis minor (OCI). The muscle arose from the ligamentum nuchae (LN; open triangles) and extended superiorly along the inferior nuchal line
Discussion
Multiple studies discuss the presence of accessory cervical muscles in various forms [2,5,6]. Development of such muscles may be due to asymmetrical embryonic development of occipital and/or cervical somites [6]. Evidence suggests that while spinalis capitis is uncommonly identified as a discrete muscle, it is often unilateral when it is identified [4]. The presence of asymmetry in the musculature responsible for extension, lateral flexion, and rotation of the cervical spine [7] presents opportunity for asymmetric cervical motion. Although the size of spinalis capitis relative to larger, parallel muscles would likely limit its impact on cervical movement, altered or impaired function of the spinalis capitis and other deep cervical musculature may result in unique patterns of somatic dysfunction. Such patterns may include restricted flexion and sidebending of the cervical spine, or possible activation of myofascial trigger points [8]. It is likely that tissue texture changes as a result of spinalis capitis hypertonicity would be palpable to an osteopathic physician. Awareness of the potential for spinalis capitis to be present, particularly asymmetrically, should be a consideration in osteopathic evaluation and treatment.
Spinalis capitis is innervated segmentally by cervical posterior rami [1]. An earlier anatomy textbook also describes a branch of the CV3 posterior ramus that courses between spinalis capitis (when present) and semispinalis cervicis [9,10]. Somatic dysfunction of spinalis capitis could result in a compressive neuropathy of cervical posterior rami, either as they innervate or bypass the muscle. Compression or entrapment of upper cervical dorsal rami may result in tension headaches and occipital neuralgia [8,11].
Furthermore, there is recent evidence that muscles in the suboccipital region have myofascial connections to the dura mater [12,13]. The ligamentum nuchae has also shown continuity with the posterior spinal dura via the atlanto-occipital and atlanto-axial membranes [1,8,14,15]. The functions of these connections are believed to involve anchoring of the spinal cord and dura, and possibly circulation of cerebrospinal fluid in the vertebral canal [12,13,15]. It is suggested that such dural connections in the occipital and upper cervical areas may contribute to cervicogenic headaches [7,8,13,14]. Unilateral strain from spinalis capitis on the ligamentum nuchae may result in abnormal tension on the cervical dura mater as a result of this dura-fascial connection, potentiating the development of a cervicogenic headache. It remains unclear if the rarely occurring spinalis capitis makes any direct myofascial connections to the cervical dura. However, the asymmetry typical of this muscle along with dysfunction might lead to more widespread cervical dysfunction, abnormal tension on the cervical dura and cervical or occipital headaches. Understanding the possible etiology of cervicogenic headaches and potential structures involved would make treatment more targeted and thus more effective.
Conclusion
We report the presence of a distinct unilateral muscle in the posterior cervical region with attachments that are most consistent with previous descriptions of spinalis capitis. This muscle is poorly described in current literature and texts and, when identified, is often fused or inseparable from semispinalis capitis. This muscle has received little attention because it is highly variable and often asymmetric. However, we suggest that such a muscle should be of special interest to anatomists and osteopathic physicians, as it might contribute to the development of cervical dysfunction or cervicogenic and occipital headache syndromes.
Acknowledgements
The authors would like to thank the donor and his family for their generous donation.
REFERENCES
- Standring S. Gray’s anatomy: the anatomical basis of clinical practice. 41st edn. London, UK: Elsevier, 2016;739-41.
- Greiner TM, Bedford ME, Walker RA. Variability in the human M. spinalis capitis and cervicis: frequencies and definitions. Ann Anat. 2004;186:185-191.
- Gilroy AM, MacPherson BR, Ross LM. Atlas of anatomy. 3rd edn. New York, NY: Thieme Medical Publishers, Inc., 2016;33.
- Moore KL, Dalley AF, Agur AMR. Clinically oriented anatomy. 7th edn. Baltimore, MD: Lippincott Williams & Wilkins, 2014;486.
- Martin A. Spinalis capitis, or an accessory paraspinous muscle? (short report). J Anat. 1994;185:195-8.
- Stanchev S, Iliev A, Malinova L, et al. A rare case of bilateral occipitoscapular muscle and literature review. Acta Morphol Anthropol. 2017;24:74-7.
- Kuchera ML, Kuchera WA. Osteopathic considerations in HEENT disorders. 1st edn. Dayton, OH: Greyden Press, LLC, 2011;259-68.
- Chaitow L, Delaney J. Clinical application of neuromuscular techniques volume 1: the upper body. 2nd edn. London, UK: Churchill Livingstone, 2008;253-93.
- Travell JG, Simons JG. Myofascial pain and dysfunction: the trigger point manual volume 1: the upper extremities. Baltimore, MD: Lippincott Williams & Wilkins, 1983;305:310.
- Mancall EL, Brock DG. Gray’s clinical neuroanatomy: the anatomical basis for clinical neuroscience. Philadelphia, PA: Elsevier, 2011;125.
- Chila AG. Foundations of osteopathic medicine. 3rd edn. Baltimore, MD: Lippincott Williams & Wilkins, 2011;493.
- Enix DE, Scali F, Pontell ME. The cervical myodural bridge, a review of literature and clinical implications. J Can Chiropr Assoc. 2014;52:184-92.
- Hack GD, Kortizer RT, Robinson WL. Anatomic relation between the rectus capitis posterior minor muscle and the dura mater. Spine. 1995;20:2484-6.
- Dean NA, Mitchell BS. Anatomic relation between the nuchal ligament (ligamentum nuchae) and the spinal dura mater in the craniocervical region. Clin Anat. 2002;15:182-5.
- Zheng N, Yuan XY, Li YF, et al. Definition of the to be named ligament and vertebrodural ligament and their possible effects on the circulation of csf. PLOS ONE. 2014;9:e103451.