Do not be fooled by appearances when N-STEMI is a TIMI 0-1 blood grade flow: Definition, prevalence, and predictive factors of total occlusion-NSTEMI
2 Public Health department, University of Poitiers, Poitiers, France, Email: Pierreingrand@yahoo.fr
Received: 14-Jun-2020 Accepted Date: Jul 15, 2020; Published: 22-Jul-2020
Citation: Roumegou P, Garcia R, Ingrand P, et al. Do not be fooled by appearances when N-STEMI is a TIMI 0–1 blood grade flow: Definition, prevalence, and predictive factors of total occlusion-NSTEMI. Clin Cardiol J 2020;4(2):7-15.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
BACKGROUND: Owing to chest pain units, rates of cardiovascular mortality due to acute coronary syndrome have decreased. However, some patients present as ACS without ST-segment elevation but with total arterial occlusion on invasive coronary angiography. This study aimed to identify the prevalence of total occlusion-NSTEMI and identify predictive factors compared to other true NSTEMI for early treatment.
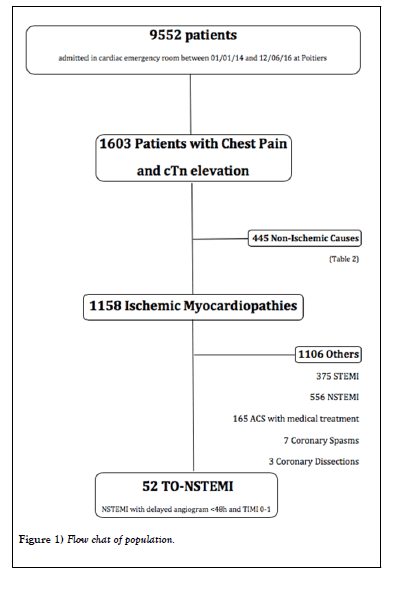
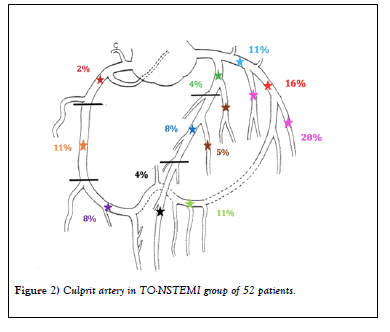
METHODS: This observational retrospective study analyzed 9552 patients admitted to the cardiac emergency room of Poitiers University Hospital between January 2014 and June 2016: among them, 1603 presented for chest pain with cardiac troponin elevation. Fifty-two patients were identified as having TO-NSTEMI. The circumflex artery was the most frequently occluded coronary artery (58%).
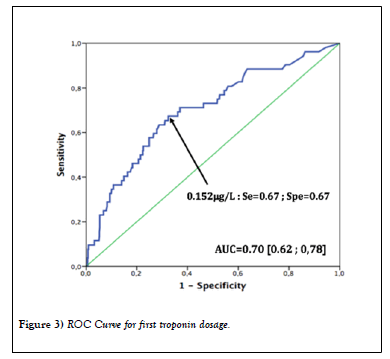
RESULTS: Multivariate analysis demonstrated that the first troponin dose was already much higher for the TO-NSTEMI group than for the NSTEMI group (P < 0.001) and that the Global Registry of Acute Coronary Events (GRACE) score was lower in the TO-NSTEMI group (P=0.01). The probability of TO-NSTEMI occurrence was significantly greater in patients with a first troponin dose >0.152 μg/L (sensitivity, 67%; specificity, 67%).
CONCLUSION: TO-NSTEMI, representing 3.2% of our acute coronary syndrome population, is not a rare diagnosis. These patients have no specific characteristics compared to NSTEMI. GRACE score does not seem predictive at all. A first troponin dose greater than ten times the normal dose must make us suspect the diagnosis. According to our study, any persistent chest pain, although slight, with abnormal ECG findings, should be considered as STEMI requiring immediate coronary angiography.
Keywords
Acute total coronary occlusion; Acute coronary syndrome; Chest pain unit; Coronary artery; Non-ST-elevation myocardial infarction; ST-elevation myocardial infarction
Abbreviations
ACS: Acute Coronary Syndrome; CPU: Chest Pain Unit; Ctn: Cardiac Troponin; CX: Circumflex Artery; ECG: Electrocardiogram; ESC: European Society Of Cardiology; GRACE: Global Registry Of Acute Coronary Events; LAD: Left Anterior Descending Artery; MI: Myocardial Infarction; NSTEMI: Non-ST-Elevation Myocardial Infarction; RCA: Right Coronary Artery; STEMI: ST-Elevation Myocardial Infarction; TTE: Trans-Thoracic Echocardiography; TO-NSTEMI: Total Occlusion-NSTEMI
Introduction
Acute coronary syndrome (ACS) is the major cause of mortality and morbidity worldwide, with 15.2 million deaths in 2016 [1]. Its management has improved notably thanks to the creation of chest pain units (CPU) in the late 1990s in the United States, which has reduced mortality rates significantly. The effectiveness of these units in the management of myocardial infarction (MI) has been demonstrated with a 50% decrease in mortality and cardiovascular events [2-5]. The concept of these units was imported into Europe in the 2000s.
Resting 18-lead electrocardiography (ECG) is the first-line diagnostic tool in the assessment of patients with suspected ACS. ACS includes ST-segment elevation myocardial infarction (STEMI), non-ST segment elevation myocardial infarction, and unstable angina according to ESC guidelines. Analysis of the ECG is therefore fundamental to differentiation between STEMI and NSTEMI and thus modifies the emergency care [6,7]. According to ESC guidelines [8], ST-segment elevation on ECG helps with the recognition of coronary occlusion and indicates emergency coronary angiography and revascularization. Furthermore, the measurement of a biomarker of cardiomyocyte injury, preferably high-sensitivity cardiac troponin (cTn), is mandatory in all patients with suspected ACS [9-11].
ST-segment elevation (measured at the J-point) is considered suggestive of ongoing coronary artery acute occlusion in the following cases: at least two contiguous leads with ST-segment elevation >2.5 mm in men aged <40 years, >2 mm in men aged >40 years, or >1.5 mm in women in leads V2–V3 and/or >1 mm in the other leads (in the absence of left ventricular hypertrophy or left bundle branch block). In patients with inferior MI, recording of the right precordial leads (V3R and V4R) seeking ST-segment elevation is recommended to identify concomitant right ventricular infarction. Likewise, ST-segment depression in leads V1 – V3 suggests myocardial ischemia, especially when the terminal T-wave is positive (STsegment elevation equivalent), and confirmation by concomitant STsegment elevation >0.5 mm recorded in leads V7–V9 should be considered a way to identify posterior MI.
However, in clinical practice, some patients present as ACS with elevated troponin but have complete occlusion on non-emergent invasive coronary angiography without ST-segment elevation. This diagnostic error leads to a significant management delay and increased mortality and major adverse cardiac event rates according to the Khan and Al. meta-analysis of 2017[12]. Several studies have shown the deleterious short and long term impact of total occlusion artery in acute NSTEMI [13-19].
Many studies have aimed to highlight indirect ECG signs that make it possible to suspect coronary occlusion [20-26]. The De Winter ECG pattern is an anterior STEMI equivalent that presents with ST depression and T wave peaks in the precordial leads and is seen in nearly 2% of acute left anterior descending coronary occlusions: “ Instead of the signature STsegment elevation, the ST-segment showed a 1- to 3-mm upsloping ST segment depression at the J point in leads V1 to V6 that continued into tall, positive symmetrical T-waves” [27].
Today, the cardiac emergency room integrated in the Cardiac Intensive Care Unit of Poitiers University Hospital can be assimilated to form a CPU to provide direct access to specialized management of chest pain among other cardiac pathologies and full technical equipment with quick access to all invasive and non-invasive cardiac diagnostic tests. This study aimed to identify the prevalence of NSTEMI with an occluded artery, also known as total occluded NSTEMI (TO-NSTEMI), on invasive coronary angiography, and search for predictive factors compared to other NSTEMI.
Research Methodology
The data, analytic methods, and study materials will be made available to other researchers for the purpose of reproducing the results or replicating the procedure.
Study design
The current observational retrospective study analysed 9552 patients including 1603 who came to the cardiac emergency room of Poitiers University Hospital between January 1, 2014 and June 12, 2016 for chest pain with cTn elevation. The study was conducted according to the ethical principles stated in the Declaration of Helsinki. There were no exclusion criteria.
Data collection
Data were collected using hospital archives and hospital software archiving medical data (Telemaque 3.7; Poitiers University Hospital, Poitiers France). All hospitalization and consultation reports were examined. If necessary, the general practitioners were contacted by phone and the reports of the referring cardiologists were obtained by fax. Sociodemographic, clinical characteristics, medical history, laboratory results, ECG description, and trans-thoracic echocardiography (TTE) reports were collected. GRACE score was systematically recalculated if all necessary data were available. Cardiologic test reports and their completion date, final diagnosis, and date of last follow-up were also collected.
Diagnosis
The TO-NSTEMI group included every patient with a NSTEMI clinical presentation at inclusion (chest pain, high-sensibility troponin elevation without ST segment elevation on ECG) but with coronary occlusion on coronary angiography (TIMI 0–1 grade flow).
Electrocardiography
All TO-NSTEMI ECG were specifically reread by 2 cardiologists and classified as normal, abnormal, ST-segment elevation, or uninterpretable. All patients benefited from an 18-lead ECG on arrival.
High-sensibility troponin
Troponin elevation was defined by an increase beyond the 99th percentile according to 2015 ECS guidelines (>0.014 μg/L in our laboratory). We collected the first dosage on arrival in cardiological emergencies, the second dosage 3 hours after the first one, and the peak level during hospitalization. TIMI grade flow
TIMI 0–1 grade flow patients were considered the TO-NSTEMI group who would benefit from earlier coronary angiography.
The coronary segments were defined according to the nomenclature of the American Heart Association and the Serruys et al. study in 1999 [28], which divided the coronary arteries into 15 segments. All coronarographies of the TO-NSTEMI group were reread specifically by 2 coronarographists [29].
Statistical analysis
Categorical variables are expressed as number and percentage, while continuous variables are shown as mean ± SD. Intergroup comparisons were performed using the chi square test for categorical variables and Student’s t-test for quantitative variables. Test characteristics and accuracy of troponin for predicting TO-NSTEMI were calculated. Univariate logistic regression was used to calculate the areas under the receiver operator characteristic curves; the troponin cutoff value was chosen as the value maximizing the likelihood ratio. The association of troponin values and occurrence of TO-NSTEMI was evaluated in univariate and multivariate logistic regression analyses. The proportional hazards assumption was confirmed as valid for each test using log-log plots. Regarding multivariate analysis, we applied a backward manual procedure performed on a maximal model including all factors that were associated with TO-NSTEMI with values of P < 0.20 in univariate logistic analysis. Analyses were performed using SPSS 22 (SPSS, Inc., Chicago, IL, USA). Two-sided P values < 0.05 were considered statistically significant.
Results
Population
Population characteristics: A total of 9552 consecutive patients came to the cardiac emergency room of Poitiers University Hospital between January 1, 2014 and June 12, 2016. Among them, 1603 patients (1112 men; mean age, 68 ±16 years) had chest pain and troponin elevation and were included (Figure 1). The patients’ baseline characteristics are summarized in Table 1.
TABLE 1: Univariate analysis of baseline characteristics between TO-NSTEM1 versus NSTENIT groups, and TO-NSTENIL versus STEM! groups.
| TO-I STEMI | NSTEMI | TO-NSTEIVII vs. NSTEIVII | STEIVII (N=375) | TO-NSTEIVII vs. NSTEIVII | ||||
|---|---|---|---|---|---|---|---|---|
| (N=S 2) | (N=566) | OR [95% CI] | Univarlate P value | OR [95% CI] | Univarlate | |||
| P value | ||||||||
| General | ||||||||
| Age (years) | 63.7 ± 10,7 | 69.6 ± 13.5 | 0.97 [0.95 - 0.99] | <0.001 | 63.6 ± 143 | 1.00 [0.98 -1.02] | 0.91 | |
| Female Sex, n (%) | 12 (23.1) | 133 (23.9) | 0.95 [0.49 - 1.87] | 0.89 | 82 (21.9) | 1.07 [0.54 - 2.14] | 0.84 | |
| GRACE Score | 128.3 ± 26.0 | 141.1 ± 33.7 | 0.99 [0.98 - 1.00] | 0.005 | 156.0 ± 34.8 | 0.97 [0.96 - 0.98] | <0.001 | |
| Cardiovascular Risk Factors | ||||||||
| Diabetes Mellitus, n (%) | 9 (17.3) | 160 (28.8) | 0.52 [0.25 - 1.09] | 0.077 | 54 (14.4) | 1.24 [0.57 - 2.70] | 0.58 | |
| Hypertension, n (%) | 25 (481) | 374 (67.3) | 0.45 [0.25 - 0.80] | 0.005 | 172 (45.9) | 1.09 [0,61 - 1.95] | 0.76 | |
| Current smoking, n (%) | 18 (34.6) | 143 (25..7) | 1.53 [0.84- 2.79] | 0,16 | 151 (40.3) | 0.79 [0.43 - 1.44] | 0.43 | |
| Medical History | ||||||||
| Atrial fibrillation, n (%) | 0 (0) | 65 (11.7) | 0 [0.00 - 0.46] | 0.009 | 13 (3.5) | 0 [0.00 - 1.86] | 0.38 | |
| Coronary artery dIsease, n (%) | 11 (21.2) | 218(39.2) | 0.42 [0.21 - 0.83] | 0.01 | 42 (11.2) | 2.12 (L01 - 4.44] | 0.042 | |
| Coronary artery bypass, n (%) | 1 (1.9) | 46 (8.3) | 0.22 [0.03 - 1.69] | 0.1 | 6 (1.6) | 1.21 [0.14 - 10.2] | 0.6 | |
| Utology | ||||||||
| First Tropontn [[/L] | 0.63 ± 0.84 | 0.25 ± 0.57 | 1.80 [1.28 - 2.52] | <0.001 | 1.46 IF 3.84 | 0.81 [0.64 -1.02] | 0.92 | |
| Second Iroponin (pg/L) | 1.38 s 1.69 | 0.45 ± 0.95 | 1.55 [1.28 - 1.88] | <0.001 | 437 ± 5_67 | 0.66 [0.54 - 0_80] | <0.001 | |
| Troponin, peak (p.g/L) | 1.93 ± 1.85 | 0.65 ± 1.13 | L59 [1.35 - 1.87] | <0.001 | 5.09 ± 6.18 | 0.71 (0.61 - 0.84] | <0.001 | |
| Transthoracic Echocardiography | ||||||||
| Simpson b [plan LVEF (%) | 561 ± 7.8) | 55.7 + 10.4 | 1.01 [0.98- 1.03] | 0.88 | 55.7 ± 10.4 | 1.04 [101 - 1,07] | 0.002 | |
| Segmentary kinetic abnormality, it (%) | 28 (5.3.8) | 278 (50) | 1.17 [0.66 - 2.06] | 0.59 | 322 (85.9) | 0.19 [0.10 - 0.36] | <0.001 | |
| Coronarography | ||||||||
| Delay after consultation (days) | 12.3 ± 1.35 | 2.90 ± 8.72 | 0.70 [0.54 - 0.89] | 4:0A01 | 0.72 ± 1.82 | 1.13 [0.99 - 1.28] | <0.001 | |
The most common cardiovascular risk factor was hypertension (935 patients [58.3%]). One-third of the population who consulted the hospital for cardiac emergencies, chest pain, and positive troponin already had known ischemic heart disease (485 patients [30.3%]). Only 396 patients (24.7%) initially had normal ECG findings.
Cardiologic tests: Most of the patients (1579 patients [98.5%]) underwent TTE. The most commonly used other cardiac examination was coronary angiography (1147 patients [71.5%]). It was first performed in 67% of patients and permitted diagnosis in 989 patients (61.7%). A total of 78 patients (4.8%) underwent coronary computed tomography in the first intention, 36 patients (2.2%) underwent myocardial scintigraphy, 24 patients (1.5%) underwent cardiovascular magnetic resonance, and 4 patients (0.2%) underwent stress echocardiography. A total of 259 patients did not undergo any cardiac examination other than TTE because of an echography or clinical diagnosis, refusal to undergo an examination, or decision to pursue non-invasive treatment due to advanced age or significant morbidity.
Diagnosis: Among our enrolled population of 1603 patients, 1158 patients (72.2%) had an ischemic cause, with NSTEMI (TIMI 2–3) in 556 patients (34.7%) and TO-NSTEMI (TIMI 0–1) with 52 patients (3.2%). A total of 291 patients (18.1%) had a cardiac but non-ischemic cause, rhythm disorder (4.8%), pulmonary embolism (4.1%), and heart failure (3.2%), while 6.3% remained undiagnosed. The diagnoses of all patients are summarized in Table 2.
TABLE 2: Final diagnostic of total chest pain and positive troponin population.
| Total Population (N=1603) | |
|---|---|
| Ischemic | 1158 (72.2%) |
| STEMI, n (%) | 375 (23.4) |
| TO-NSTEMI, n (%) | 52 (3.2) |
| NSTEMI, n (%) | 556 (34.7) |
| ACS Medical Treatment, n (%) | 165(103) |
| Coronary Dissection, n (%) | 3(0.2) |
| Cardiac Non-1schemic | 291 (18.1%) |
| Rhythm disorder, n (%) | 76 (4.8) |
| Rubmanary embolism, n (%) | 66 (4.1) |
| Severe valvular disease, n (%) | 26 (1.7) |
| Myocarditis, n (%) | 25 (1.5) |
| Tako-Tsuho syndrome, n (%) | 26 (1.6) |
| Cardiac tamponadc, n (%) | 8 (0.5) |
| Acute aortic syndrome, n (%) | 11 (117) |
| Heart Failure, n (%) | 51 (3.2) |
| Extra Cardiac Disease | 55 (3.4%) |
| No Diagnosis | 99 (6.3%) |
TO-NSTEMI
Population characteristics
During this period, 52 patients presented with TO-NSTEMI, representing 3.2% of the 1603 patients with chest pain and elevated troponin. The circumflex artery (CX) was the most frequently occluded coronary artery, with 30 cases (58%), distributed in 6 proximal CX (Segment 11), 8 mid-CX (Segment 13), 6 distal CX (segment 15), and 10 marginal branches (Segments 12 and 14). The left anterior descending artery (LAD) was occluded in 11 patients (21%), distributed in 2 proximal LAD (Segment 6), 4 mid-LAD (Segment 7), 2 distal LAD (Segment 8), and 3 diagonal branches (Segments 9 and 10). The right coronary artery (RCA) was occluded in 11 patients (21%), distributed in 1 proximal RCA (Segment 1), 6 mid-RCA (Segment 2), and 4 distal RCA (Segments 3 and 4) (Figure 2) [30-32].
Predictive factors
Except for hypertension (P=0.005), there was no clinical differences between the TO-NSTEMI and NSTEMI groups.
In medical history, patients in the TO-NSTEMI group had less atrial fibrillation (0 versus 65 patients [11.7%], P=0.009).
On the biological side, all troponin dosages, but principally the first, were significantly higher in the TO-NSTEMI group (P < 0.001). The first troponin dosage to predict TO-NSTEMI is shown in Figure 3. The troponin cutoff value of 0.152 μg/L (more than 10 times normal) showed a 67% sensitivity and specificity for predicting TO-NSTEMI. For TTE, the two groups did not differ in left ventricular ejection fraction (P=0.88) or segmental kinetic abnormality (P=0.59). The mean GRACE score was lower in the TO-NSTEMI group (128.3 ± 26 versus 141.1 ± 33.7; P=0.005).
According to univariate Cox proportional hazard model analysis, younger age, lower GRACE score, absence of hypertension, atrial fibrillation or coronary artery disease, and high first troponin level were significantly predictive factors of TO-NSTEMI. On multivariate analysis, lower GRACE score, high first troponin, and hypertension remained significantly and independently associated with TO-NSTEMI (odds ratio [OR], 2.26, 95% confidence interval [CI], 1.53–3.35, P < 0.001; OR, 0.98, 95% CI, 0.97– 0.99, P=0.01; and OR, 2, 95% CI, 1.08–3.70, P=0.03) for hypertension (Tables 3 and 4).
TABLE 3: Multivariate analysis of predictive factors of TO-N STEMI vs. NSTEMl.
| Variables | OR | 95% CI | P-value |
|---|---|---|---|
| Hypertension (Yes vs. No) | 2.07 | 1.12 - 3.82 | 0.02 |
| First Troponin (1 unit increment) | 2.21 | 1.52 - 3.22 | 0.001 |
| GRACE Score (1 point increment) | 0.986 | 0.976 - 0.996 | 0.405 |
TABLE 4: Multivariate analysis of predictive factors of TO-NSTEM vs. STEMI.
| Variables | OR | 95% CI | P-value |
|---|---|---|---|
| Age (1 year increment) | 1.1 | 1.06 - 1.14 | <0.001 |
| Segmentary kinetic abnormality (Yes vs. No) | 4.56 | 2.22- 9.36 | <0.001 |
| GRACE Score (1 point increment) | 0.938 | 0.920 - 0.955 | <0.001 |
| Logistic model c-index=0.865 |
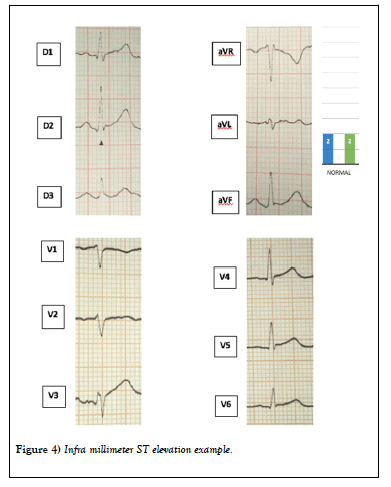
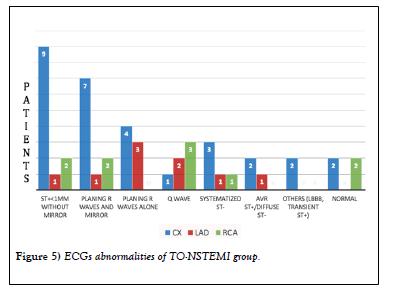
Electrocardiography: We reviewed all ECGs performed at initial management in these TO-NSTEMI patients to identify potential diagnostic errors or atypical ECG signs to allow for faster revascularization. No ECG findings strictly corresponded to the electrical description of STEMI of the ESC Guidelines. The main ECG modification was infra-millimetre ST segment elevation without mirror, especially for the CX (Figure 4).
The other most common repolarization disorder was planning R waves with or without mirror. Only 4 ECG were strictly normal at initial management (Figure 5).
Three ECG could not be recovered for further reading. Two occlusions of the LAD and one of the RCA were noted.
Discussion
A total of 52 patients presented with TO-NSTEMI between 2014 January and 2016 June at the Poitiers CPU, representing 3.2% of all consultations for chest pain with elevated troponin at the Poitiers’s CPU.
The principal culprit coronary occluded is the CX, primarily its marginal branches. The lateral territory is poorly discriminated by ECG. We could not identify a common ECG anomaly for all patients, even if the inframillimetre ST elevation segment without mirror seemed more frequent with planing R waves. The De Winter pattern was found in only 2 cases of LAD occlusion. It is important to emphasize that less than 10% of ECG are normal [33]. The lack of reliability of echocardiography concerning a segmental kinetic abnormality is an additional marker of the difficulty highlighting these occluded coronaries. We observe indeed, that TTE has the same limits as ECG to discriminate the circumflex territory kinesis abnormality. Several reasons can explain it: differences of experience according to the examiner, the myocardial territory affected often restricted, the earliness of examination without kinesis abnormalities yet, a poor echogenicity for some patients, or a difficulty to evaluate the antero lateral area because of the papillary muscle.
Troponin seems to be an essential marker for suspected TO-NSTEMI and should lead to rapid coronary angiography. We are often alerted by this second troponin dosage, which rises abruptly for the TO-NSTEMI group and leads us to perform coronary angiography; however, while waiting for this second troponin level, it is already too late for myocardial necrosis. We must be very vigilant and reactive about the patient’s clinical evolution, dynamic repolarization disorders, and the first troponin level (even sometimes before first troponin). Specifically, we should not wait for the second troponin level to consider revascularization in cases of strong suspicion. In the 2015 ESC guidelines, there is no troponin cutoff for NSTEMI to perform immediate coronary angiography. According to this study, we propose an immediate invasive strategy for all NSTEMI presentations with a first troponin level that is more than 10 times the normal level. GRACE score does not seem discriminating enough for this particular population, possibly due to a younger population of patients with TO-NSTEMI and a lack of consideration of troponin value and its positivity.
In the ESC guidelines, persistent chest pain is an indication for early revascularization since acute coronary syndrome is considered a STEMI. However, patients are often treated in the emergency room with high doses of morphine to control chest pain, making it impossible to clinically monitor the persistence of myocardial ischemia.
We must be very attentive to the patient’s symptoms: in particular, we must remain vigilant for patients who had severe chest pain that then reduced significantly with a simple sensation of persistent pain or heaviness but that was much better tolerated by the patient and falsely reassuring. It is not normal for chest discomfort to persist, even if it is very moderate: early angiography must be performed.
Total analgesic control is also essential: after a first chest pain episode, even slight remaining discomfort is not normal. We must be very vigilant of this, as it is currently impossible to leave our patients with myocardial ischemia in the CPU. These TO-NSTEMI cases should not be trivialized but considered diagnostic failure, even more so when we observe that this population has increased mortality and morbidity rates compared to those with NSTEMI.
This study also demonstrated no significant intergroup difference in terms of coronary angiography delay: At the time of revascularization, most infarcts in the TO-NSTEMI group were already constituted. With the development of interventional invasive cardiology, we can also support all future ACS cases like STEMI cases. With the current technical progress, it seems more prudent to perform coronary angiography in cases of doubt than to let a patient experience myocardial necrosis in CPU.
Limitations
This study was limited by its monocentric retrospective nature based on the analysis of hospitalization and consultation reports with information bias. The notation of persistent chest pain was not found in many reports.
Conclusion
TO-NSTEMI is not a rare diagnosis, as it affected 3.2% of our enrolled population. It is important to improve the diagnosis of these cases to continue to reduce ACS-related mortality and morbidity rates. Our study confirmed the difficulty highlighting these TO-NSTEMI cases with identical clinical characteristics to those of NSTEMI and the lack of reliability of the GRACE score and TTE findings. A first high troponin must indicate the diagnosis, especially if it is 10 times higher than normal. According to our findings, every persistent chest pain, even the slightest, with minor ECG abnormalities should be considered STEMI and subjected to immediate coronary angiography.
REFERENCES
- WHO (World Health Organization). Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000-2016.
- Storrow AB, Gibler WB. Chest pain centers: Diagnosis of acute coronary syndromes. Ann Emerg Med. 2000;35(5):449-61.
- Furtado MV, Cardoso A, Patrício MC, et al. Influence of implementation of a chest pain unit on acute coronary syndrome outcomes. J Emerg Med. 2011;40(5):557-64.
- Keller T, Post F, Tzikas S, et al. Improved outcome in acute coronary syndrome by establishing a chest pain unit. Clin Res Cardiol, 2010;99(3):149-55.
- Puymirat E, Simon T, Cayla G, et al. Acute myocardial infarction: Changes in patient characteristics, management, and 6-month outcomes over a period of 20 years in the FAST-MI Program (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) 1995 to 2015. Circulation, 2017;136(20):1908-1919.
- Nikus K, Pahlm O, Wagner G, et al. Electrocardiographic classification of acute coronary syndromes: a review by a committee of the International Society for Holter and Non-Invasive Electrocardiology. J Electrocardiol. 2010;43(2):91-103.
- Roffi M, Patrono C, Collet JP, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(3):267-315.
- Ibanez B, James S, Agewall S, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC), European Heart Journal, 2017;39(2):119-177.
- Thygesen K, Mair J, Giannitsis E, et al. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur Heart J. 2012;33:2252-57.
- Rokos IC, French WJ, Mattu A, et al. Appropriate cardiac cath lab activation: optimizing electrocardiogram interpretation and clinical decision-making for acute ST-elevation myocardial infarction. Am Heart J. 2010;160(6):995-1003.
- Parmacek MS and Solaro RJ. Biology of the troponin complex in cardiac myocytes. Prog Cardiovasc Dis. 2004;47(3):159-76.
- Khan AR, Golwala H, Tripathi A, et al. Impact of total occlusion of culprit artery in acute non-ST elevation myocardial infarction: a systematic review and meta-analysis. Eur Heart J. 2017;38(41):3082-9.
- Wang TY, Zhang M, Fu Y, et al. Incidence, distribution, and prognostic impact of occluded culprit arteries among patients with non-ST- elevation acute coronary syndromes undergoing diagnostic angiography. Am Heart J. 2009;157:716-23.
- Bahrmann P, Rach J, Desch S, et al. Incidence and distribution of occluded culprit arteries and impact of coronary collaterals on outcome in patients with non-ST-segment elevation myocardial infarction and early invasive treatment strategy. Clin Res Cardiol. 2011;100:457-67.
- Kim MC, Ahn Y, Rhew SH, et al. Impact of total occlusion of an infarct-related artery on long-term mortality in acute non-ST-elevation myocardial infarction patients who underwent early percutaneous coronary intervention. Int Heart J. 2012;53:160-4.
- Shin DI, Chang K, Ahn Y, et al. Impact of occluded culprit arteries on long-term clinical outcome in patients with non-ST-elevation myocardial infarction: A 48-month follow-up results in the COREA-AMI Registry. J Interv Cardiol. 2014;27:12-20.
- Warren J, Mehran R, Yu J, et al. Incidence and impact of totally occluded culprit coronary arteries in patients presenting with non-ST- segment elevation myocardial infarction. Am J Cardiol. 2015;115:428-33.
- Karwowski J, Polonski L, Gierlotka M, et al. Total coronary occlusion of infarct-related arteries in patients with non-ST-elevation myocardial infarction undergoing percutaneous coronary revascularization. Kardiol Pol. 2017;75:108-16.
- Setianto BY, Taufiq N, Hernawan H. Left Circumflexus Coronary Artery Occlusion with Clinical Presentation as NSTEMI and Acute Pulmonary Oedema. Acta Med Indones. 2017;49(1):52-56.
- De Winter RW, Adams R, Verouden NJ, et al. Precordial junctional ST-segment depression with tall symmetric T-waves signifying proximal LAD occlusion, case reports of STEMI equivalence. J Electrocardiol. 2016;49(1):76-80.
- Abdelwahed A, Eskola M, Kosonen P, et al. Electrocardiographic findings during ballon angioplasty of the left circumflex coronary artery-influence of location of the ischemic segments with respect to the obtuse margin of the left ventricle. J Electrocardiol. 2017;50(1):102-110.
- Wall J, White LD, Lee A. Novel ECG changes in acute coronary syndromes. Would improvement in the recognition of 'STEMI-equivalents' affect time until reperfusion? Intern Emerg Med. 2018;13(2):243-9.
- Vives-Borras M, Moustafa AH, Alvarez-Garcia J, et al. Clinical and Prognostic Value of the Electrocardiogram in Patients with Acute Occlusion of the Left Circumflex Artery. Am J Cardiol. 2017;120(9):1487-94.
- Verouden NJ, Koch KT, Peters RJ, et al. Persistent precordial “hyperacute” T-waves signify proximal left anterior descending artery occlusion. Heart. 2009;95(20):1701-6.
- Massobrio L, Scarrone A, Valbusa A. ECG pattern of STEMI equivalent without coronary occlusion. J Electrocardiol. 2016;49(2):248-9.
- Sadowski M, Gutkowski W, Raczyński G, et al. Acute myocardial infarction due to left main coronary artery disease in men and women: does ST-segment elevation matter? Arch Med Sci. 2015;11(6):1197-204.
- De-Winter RJ, Verouden NJ, Wellens HJ, et al. A new ECG sign of proximal LAD occlusion. N Engl J Med. 2008;359(19):2071-3.
- Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: A method for prognostication and therapeutic decision making. JAMA. 2000;284:835-42.
- Serruys PW, Unger F, Van Hout BA, et al. The ARTS study (Arterial Revascularization Therapies Study). Semin Interv Cardiol. 1999;4:209-19.
- Karwowski J, Poloński L, Gierlotka M, et al. Total coronary occlusion of infarct-related arteries in patients with non-ST-elevation myocardial infarction undergoing percutaneous coronary revascularization. Kardiol Pol. 2017;75(2):108-116.
- Karwowski J, Gierlotka M, Gąsior M, et al. Relationship between infarct artery location, acute total coronary occlusion, and mortality in STEMI and NSTEMI patients. Pol Arch Intern Med. 2017;127(6):401-411.
- Dixon WC 4th, Wang TY, Dai D, et al. Anatomic distribution of the culprit lesion in patients with non-ST segment elevation myocardial infarction undergoing percutaneous coronary intervention: findings from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2008;52:1347-1348.
- Spaulding CM, Joly LM, Rosenberg A, et al. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med. 1997;336:1629-1633.