Driving safety following open heart surgery
2 Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
3 Occupational Therapy Department, Rabin Medical Center, Beilinson Hospital, Petah Tikva, Israel
Received: 12-Apr-2021 Accepted Date: May 12, 2021; Published: 19-May-2021
Citation: Josefson EK, Weiss P, Ankonina ON, et al. Driving safety following open heart surgery. Clin Cardiol J. 2021;5(3):1-13.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Cardiovascular diseases and their complications are a principal cause for morbidity and mortality worldwide. There is an increase among the elderly population undergoing open heart surgery with a valid driving license. There are no guidelines and regulations regarding when is it safe to return driving following open heart surgery.
The aim of this study was to test the ability of patients post open heart surgery in order to determine the optimal time interval after which driving will be considered as safe.
Methods: Patients following heart surgery, completed a test battery at either two week (N=50) or three months (N=90). Study participants, filled out questionnaires and completed a driving simulation. Simulation score was calculated according to the severity of the number of traffic violations normalized to participants’ age.
Results: Average age of study participants was 63.94 (SD=9.58) years. Three months post-surgery, patients presented significant improvement in the ability to carry out physical activities (p<0.001), were in an improved emotional state (p<0.05), and displayed less pain (p<0.001). Regarding their driving ability patients exhibited improved handling of vehicle controls (p=0.01) and safer driving (p<0.05), compared to two weeks postsurgery.
Conclusion: Our findings show for the first time that it is safer to return to driving after three months and not after two weeks. We suggest that Medical guidelines for post open heart surgery should include a recommendation of returning to drive only after three months. Future randomized trials should be conducted in order to confirm the results of this study.
Keywords
Driving; Cardiac surgery; CABG
Abbreviations
CABG: Coronary Artery Bypass Grafting; CCS: Canadian Cardiology Society; ESC: European Society of Cardiology; SSQ: Simulator Sfickness Questionnaire
Introduction
Driving is considered a common and valued daily activity in all developed countries. It has been estimated that drivers of private vehicles, depending upon age and occupation, may spend an average of 250 hours a year behind the wheel [1]. For professional drivers this figure is much higher. Car driving is a highly regarded privilege, yet it is also an inherently dangerous one, associated with significant mortality and morbidity. Because the global population is gradually aging, older drivers, especially because of their age-related frailty, are likely to make up an increasing proportion of fatality statistics [2]. Acute medical conditions that may impair driving may contribute to these statistics. The actual contribution of medical causes to motor vehicle accidents is unknown. Data from Canada and the US suggest that about 5% of accidents involving commercial vehicles can be attributed to cardiovascular disease [3,4]. Driving regulations for patients with heart disease are not unanimous across Europe nor in the USA. There is a relative lack of hard scientific data and strong socio-economic dimensions of determining medical fitness to drive complicate this issue even more.
Heart disease is the first leading cause of death in the US [5]. Furthermore, there is an increase among the elderly population holding valid driving licenses undergoing open heart surgery. Nevertheless, the hospitalization period is relatively short, five days on average, and therefore acute care medical staff may not professionally relate to the pace of returning to all previous activities, amongst them driving. An additional factor that increases the problem is the aging of the population. This leads to an increase from year to year in the percentage of elderly drivers [6]. In Israel, according to the central bureau of statistics, at the end of 2009, 35% of the elderly population (age 65 years or above) were licensed to drive [7]. At the end of 2019 the percentage increases to 53% [8]. In the U.S. as well, the growth in life expectancy leads to a rise of more eligible drivers who are over 65 years of age [9].
Nevertheless, policies and guidelines for driving with heart disease or post open heart surgeries, lack a base of evidence.
In the case of CABG (coronary artery bypass grafting), both the CCS (Canadian Cardiology Society) and the ESC (European Society of Cardiology) recommend that noncommercial drivers should wait for a period of at least 1 month after discharge, however this time period was never backed up by comprehensive research indicating that the patient is capable of safe driving at that time. Additionally, it is most probable that this directive relates primarily to the recovery of scar tissue, and not necessarily to the functional ability of the individual as it relates to driving. Regarding commercial drivers the CCS recommends a period of three months before the patient can return to drive [10].
Both the European and the Canadian guidelines permit non-commercial driving in all patients following heart failure except those with symptoms at rest or at the wheel. According to the CCS, patients who have undergone a heart transplant are eligible for (re-) licensing for commercial driving six months after discharge, if the LV ejection fraction is >35% and there are no signs of ischemia [10].
The goal of this study was to set guidelines for the optimal time interval after which driving post open heart surgery will be considered safe, for the patients and others in their surroundings. We aimed to standardize the period of time considered unsafe for driving and hence contribute to the reduction of motor vehicle accidents.
Methods
Patients post open heart surgery was included in a clinical trial following approval by the institutional review board. Study participants filled out study evaluation questionnaires at two different times: two weeks and three months post-surgery. In addition, their driving performance was evaluated using a STISM simulator.
Patient’s data collection/Study design
The study population consisted of patients who were scheduled to undergo bypass surgery. As this surgery is more common in males we chose to focus on the male gender for this study. Patient population was examined at two time points; two weeks (50) and three months (90) post-surgery (The time point the CCS has set safe for commercial drivers to return to drive). Patients filled out various questionnaires, history and driving routine, quality of life and assessment of mental state. In addition, patients underwent computerized driving simulation either at time one or time two, this to eliminate potential learning effect of simulator use. Blood samples were taken from all patients (Serum Creatinine and hemoglobin indicating renal function and blood volume) to ensure that there were no confounding factors that could have affected the results (data not shown). A control group consisted of men over the age of 65 who had not gone through open-heart surgery but had a similar psychosocial background. These participants answered questionnaires and performed the computer simulation. No laboratory tests were taken in the control group.
Exclusion criteria
1. Post-operative complications
2. Patients scoring over 6 points on Simulator sickness Questionnaire.
3. Occupational therapist observation - patient that had difficulties to operate the simulator were excluded from the study.
Data Collection
Patients found eligible for the study, signed a consent form for participation in the study. Each patient’s medical condition, background illnesses, and other psychometric data were entered into the study’s database.
Driving habits Questionnaire
This questionnaire was developed by occupational therapists involved in the field of driving rehabilitation (Israeli Ministry of Health, 2005). The questionnaire is based on a review of existing literature and questionnaires in the field. The questionnaire examines: the importance of driving for driver, driving characteristics, frequency of driving, driving purposes, review of accidents and self-awareness questions. The questionnaire consists of both qualitative and quantitative items. The questionnaire has been used in several studies, yet no psychometric data has been published as of yet for this questionnaire [11,12]. Patients were asked to answer the questionnaire when performing the simulation at both time points
SF36 Questionnaire
This questionnaire includes 36 items, which address both physical and mental quality of life. Physical and Mental Health Composite Scores (PCS & MCS) are computed using the scores of 36 questions and range from 0 to 100, where a zero score indicates the lowest level of health measured by the scales and 100 indicates the highest level of health. These two values were calculated in the current study to examine interventions effect on participants’ health related quality of life [13].
SSQ - Simulator sickness Questionnaire
The Simulator Sickness Questionnaire was developed by Kennedy and colleagues in 1993 [14] in order to determine if simulation causes simulator sickness, as there is documentation regarding this phenomenon, due to the gap between the non-movement bodily experience, and the movement experienced by the visual input on the brain. The questionnaire includes a list of 27 symptoms which are commonly experienced by users of virtual reality systems. Each item is rated on a 4 point Likert scale ranging from none, slight, moderate to severe. Four representative scores can be calculated. Nausea-related subs-core (N), Oculomotor-related sub-score (O), Disorientation-related sub-score (D) are the scores for the symptoms of specific aspects. Total Score (TS) is the score representing the overall severity of cybersickness experienced by the users of virtual reality systems. Simulator Sickness Questionnaire is a widely applied measurement tool in research studying simulator sickness and cybersickness. In the current study, patient whose total score was over 6 were excluded from the study.
Driving simulator observation form
A structured observation form was developed to register cognitive aspects, such as decision making and adherence to rules as well as additionally physical, verbal and non-verbal reactions to the simulation. This form was developed by Lee [15], translated and adapted into four categories, with internal reliability assessed for three categories: Bodily reactions to pedestrians, road signs, vehicles and accidents α=.74. The second category included physical use of simulator accessories- wheel and pedals in relation to the first category criteria, α=0.76. The third category included cognitive behavioral areas, such as working memory, attention, learning, and control of virtual environment α=0.81. An additional category was the evaluation of driving ability in a simulator [11]. This form was filled out by either an occupational therapist or research coordinator who had undergone specialized training on simulator assessment and observation for the current study.
Driving simulation
Driving Simulator (STISIM - System Technologies Inc. SIMulator) - This is an interactive computer software designed to evaluate driving in a simulated environment. The system is installed on a flat wide stationary computer screen and includes controls- a steering wheel and pedals. The subject performs two driving scenarios, the first enabling familiarizing the patient with the system. The second is a test scenario, which evaluates driving on urban and intercity roads. Each offense receives a quantitative score based on the number of times a particular one (high velocity, collision, leaving road margin, non-compliance with traffic light, etc.) was performed during the test, and is expressed by a total score (called total sim). Therefore, a lower score indicates better driving. Previous work has found that the driving simulator has high ecological validity for predicting actual driving ability as well as criterion validity [15,16].
At the end of each simulation, the system generates a report listing all of the participants traffic offenses. For the purpose of the current study and to normalize the offenses in relation to actual traffic conditions, we developed an adjusted violation score which takes into account the participants age and the severity of driving offenses according to the “point system” that is applied in Israel. The amount of points is given according to the violation severity. Over 12 accumulated points entails a mandatory refresher course on driving safety and regulations [17] The adjusted calculated score for the simulation is presented below. We multiplied the violation as recorded on simulator results by the number of points allocated by the Israeli scoring system, and divided the total sum of adjusted violations by age of testee.
Traffic offense calculated in the simulation score:
A- Centerline Crossing
B- Road edge excursion
C- Vehicle collisions
D- Collision with pedestrian
E- Speeding tickets
F- Traffic light tickets
G- Stop sign tickets
Score= A×6+ B×6+ C×8+ D×15+ E×8+ F×10+ G×10/participant age
Statistical analysis
One way ANOVA was conducted for a comparison of three groups followed by post hock comparison. T-test was applied for comparison of two groups.
Results
Demographic characteristics and driving performance scores for all study participants are presented in Table 1. The control group age was 76 ± 6.38 years vs. the post-op two weeks patients age that were 62.72 ± 8.43 years and the post-op three months patients that were 63.03 ± 8.83 years. Control group driving seniority was 46.17 ± 12.64 years vs. the post-op patients that were 40.67 ± 9.86 and 41.38 ± 8.77 years for the two weeks and three months groups respectively. All study participants drive approximately six days a week and estimate them self as good drivers. There was no statistical difference between hospitalization duration among the patient’s group.
| Variables | Control group (7) | Two weeks post—surgery group (50) | Three weeks post—surgery group (90) |
|---|---|---|---|
| Age (years) Mean ± SD | 76.00 ± 6.38 | 62.72 ± 8.43 | 63.03 ± 8.83 |
| Gender (male) | 100% | 100% | 100% |
| Driving seniority (years) | 46.17±12.64 | 40.67 ± 9.86 | 41.38 ± 8.77 |
| Average driving days per week, Mean ± SD | 6.2 ± 1.79 | 6.21 ± 1.28 | 6.05 ± 1.5 |
| Driving abilities estimated by participant (good) | 100% | 83.72% | 93.67% |
| Hospitalization during (days) Mean ± SD |
0 | 6.26 ± 1.36 | 6.62 ± 2.91 |
| Smoker* | 0% | 36.17% | 29.41% |
| Alcohol* | 14% | 0% | 1.17% |
| Drugs* | 0% | 2.12%) | 1.17% |
Table 1: Demographic characteristics and driving habits for all study participants (*p<0.05).
Driving habits Questionnaire
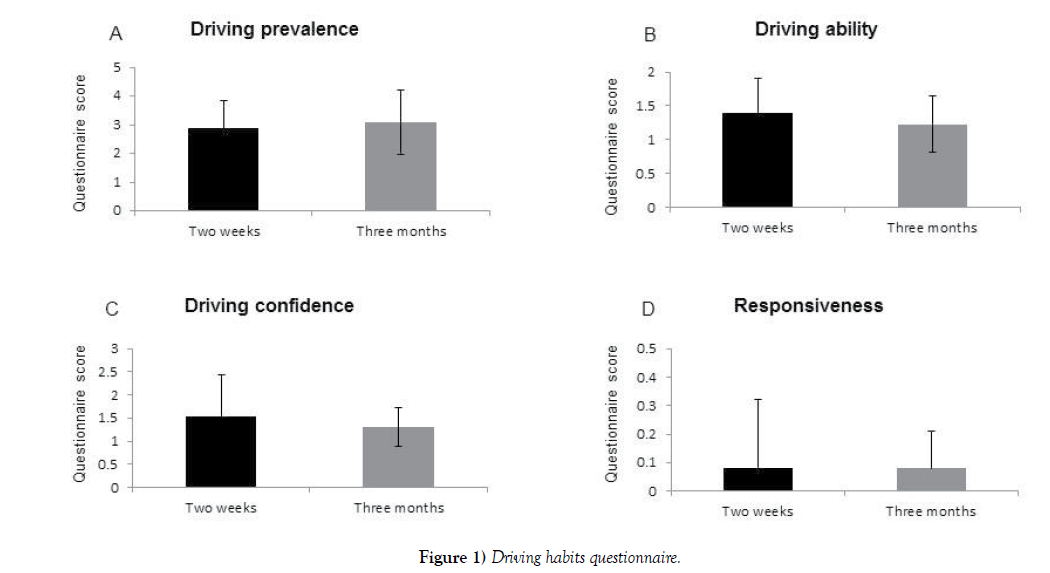
In this self-filled questionnaire, the subject indicates what kind of a driver he perceives himself to be. Each participant was asked to answer the following questions: (Partial list – Supplementary 1, Figure 1).
• Which way do you prefer to get around; Drive yourself/have someone drive you/use public transportation?
• How fast do you usually drive compared with the general flow of traffic? Much faster/somewhat faster/about the same/somewhat slower/much slower.
• In an average week haw many days per week do you normally drive? 1-2 days/3-4 days/5-7 days.
• During the past 3 months, have you driven while it has been raining? Yes/no
• Would you say that you drive alone with: no difficulty at all/a little difficulty/moderate difficulty/extreme difficulty?
• During the past 3 months, have you parallel parked? Yes/no.
• During the past 3 months, have you driven at night? Yes/no.
Three months post-op the questionnaire score was no different than the score achieved at the two-week’s time point; In both times points the patients were feeling confidence regarding their ability to drive (Figures 1A-1D).
SF36 - Quality of life questionnaire (Appendix 2)
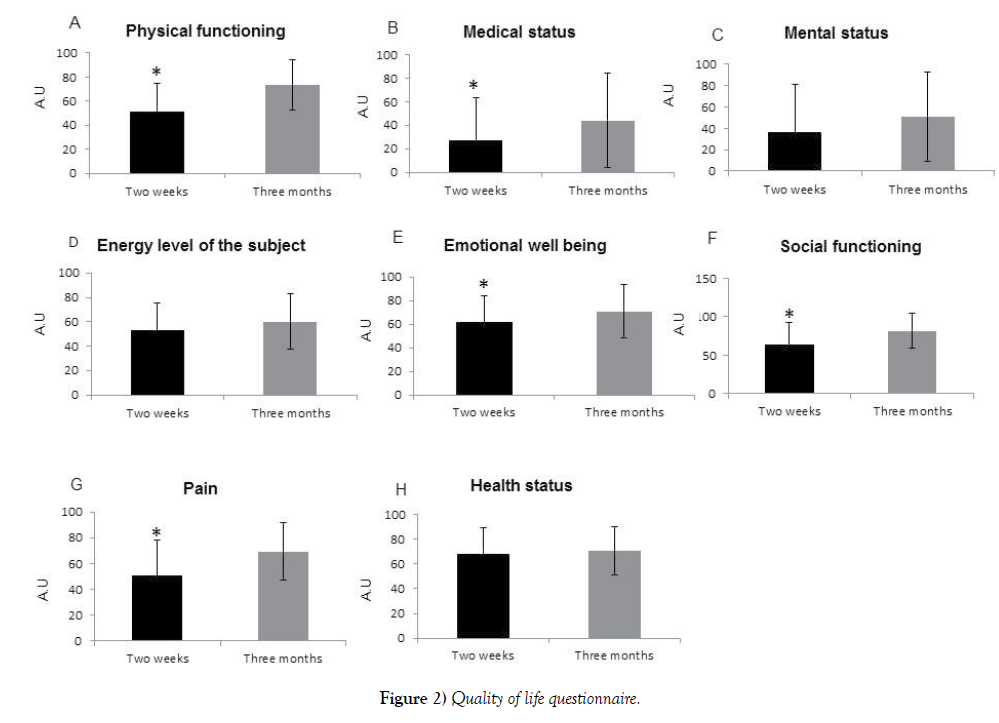
In this questionnaire, the subject has to answer how much physical or mental restriction he experiences. The questionnaire was delivered at the two time points to examine whether there is an objective improvement after three months. Three months after surgery participants felt less physically restricted, and able to perform more physical activities P< 0.01(Figure 2A), they felt less restricted due to their medical status, P=0.027 (Figure 2B) and less depressed, P = 0.05 (Figure 2E). Moreover, after three months patients felt that their social activities are less limited p<0.001 (Figure 2F) by their medical condition. Additionally, they report that they do not suffer from pain and pain does not interfere with their ability carrying out daily activities (P<0.001) (Figure 2G). No difference was found in patient mental status, energy level and health status (Figures 2C, 2D, 2H)
Observation of simulation by examiners
The examiners observe each subject during the simulation. Three months after surgery, the subject’s ability to use and control the simulator controls were found to be better (Figures 3A-3D); e.g. Their ability to use the simulator was also found to be better P=0.01 (Figure 3A) and their body response to the simulation was more precise; P = 0.013 (Figure 3B).
Driving simulator
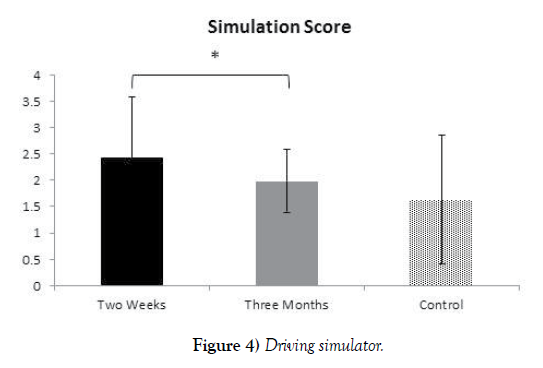
All participants underwent a driving simulation at two weeks and three months post-surgery. Participants performed two driving scenarios; the first enabled familiarizing with the system. The second was a test scenario, which evaluated driving on urban and intercity roads. Each offense received a quantitative score based on the its repeatability (high velocity, collision, leaving road margin, non-compliance with traffic light, etc.) simulation ‘total score’ was normalized as described in methods. Driving evaluation on simulator was significantly better three months post open heart surgery compared to driving ability two weeks post-surgery, p=0.04 (Figure 4). Furthermore, the control groups driving abilities did not significantly differ from the driving abilities of the participants evaluated three months postsurgery, thus attesting to the full return to driving ability three months postsurgery.
Discussion
Undergoing CABG surgery raises questions regarding the correct time frame in which it is safe and recommended to reassume driving. Complete sternal healing after coronary artery bypass grafting may take over three months [18]. Furthermore, during the healing process one gradually regains energy, overcoming tiredness, endurance. In some cases, the effect on driving safety and hence on license status needs to be individually assessed [19]. Nevertheless, physicians and medical staff have a legal and ethical obligation to be able to advise post-surgical patients on discharge regarding their ability to return to drive. Guidelines on this topic are vague and not evidence based. The current study is innovative in its field. This study examines the ability and safety of male patients to drive after bypass surgery.
Patients were examined at two post-operative time points and assessed using both questionnaires as well as using a driving simulation. Participants were required to fill out questionnaires- one related to physical and emotional/ mental quality of life (SF-36) and one that is focused on driving habits. Three months post-surgery participants self-identified a significantly improved physical and mental state, according to the SF-36 questioner (Figure 2). Furthermore, Participants experienced less restriction in their daily activities and were significantly more capable of performing physical actions comfortably. Moreover, they experienced an improved emotional state, were more energetic and felt less fatigue and pain (Figure 2). Regardless of the participants improved state of health, according to their driving habits questionnaire, the participants assessed that their driving ability was similar both at two weeks and three months post-surgery (Figure 1). Although feeling weaker and less physically competent at two weeks, they did not self regulate their driving in order to match the constrictions they were experiencing. Selfregulation of driving behavior depends on self-monitoring and subsequently, on the need to change driving behavior, in order to maintain an acceptable level of safety [20]. In order for self-regulation to be successful (i.e. to reduce crash involvement but not unnecessarily hinder mobility), it is important that self-regulation be practiced by those drivers who are likely to have a greater than average crash risk, while those drivers with a low risk of crashing can impose less self-restriction on their driving behavior [20]. Older adults perceive themselves as good drivers; however, their perception may not be accurate, and could negatively affect their driving safety. A study that examined the accuracy of older drivers’ self-awareness of driving ability in their everyday driving environment by determining the concordance between the perceived and actual driving performance, found that most older adults over estimated their driving ability [21]. Considering this detail, it is clear that “handing over” the decision making of determining driving fitness to the drivers themselves, is not recommended. This points to the important role physicians and medical staff plays in guiding and instructing patients regarding their returning to drive.
In the current study, actual driving was significantly improved three months post-surgery, as compared to two weeks post-surgery, with less involvement in MVAs (Figure 4). This provides additional evidence to the fact that participants were still in a compromised condition for driving two weeks post-surgery. Patients were seen to be more confident in their driving and rated themselves as better drivers three months post-surgery compared to the two-week postoperative time point (Figure 2). In addition, patients demonstrate that they are better able to respond to diverse driving scenarios after three months (Figure 4). Thus implying that the skills required for making swift decisions, coping with diverse situations improves with time. These skills are inherent and crucial for safe driving at both tactical and maneuvering levels of vehicle control. Supporting data can be obtained from the observation of the patient during the simulation (Figure 3). This observation shows significant improvement, both in the physical use of the simulator itself (use of the steering wheel and pedals) and of the subject’s body reactions (shifting gaze, voice etc.). It should be noted that there is also an improvement in the overall impression of the evaluator regarding driving ability after three months.
Conclusion
In conclusion, the elaborate simulator score is consistent with all data gathered so far in the study. According to our refinement, there is a direct relationship between the amount of traffic offenses and the final score. Participants at the three-month time point can be seen to commit fewer traffic offenses than participants two weeks post-surgery (p=0.04). Simulation score of the threemonth patients group was not significantly different from the control group, thus it may be concluded that it is safe to return to driving three months post-surgery.
The purpose of this study was to create driving safety guidelines for patients planning to return to drive after open heart surgery. From the analysis of this study we can clearly conclude that it is safer to return to drive after three months. This conclusion is based on both subjective experience/description of the patients (questionnaires that the patient personally answered) and the objective research data (simulation and observation). It is important to note that this research is a breakthrough in its field and will form the basis for guidelines after heart surgery in the world and in Israel in particular.
Funding
This research was funded by the Research Fund on Insurance Matters Affiliated with the Israel Insurance Association (RA).
Conflict of Interest
The authors declare that they have no conflict of interest.
REFERENCES
- Petch MC. Driving and heart disease. Eur Heart J. 1998;19:1165-77.
- Spano G, Caffò A. Lopez A, et al. Validating Driver Behavior and Attitude Measure for Older Italian Drivers and Investigating Their Link to Rare Collision Events. Front Psychol. 2019;3389
- Epstein AE, Baessler CA, Curtis AB, et al. Personal and public safety issues related to arrhythmias that may affect consciousness: implications for regulation and physician recommendations. A medical/scientific statement from the American Heart Association and the North American Society of Pacing and Electrophysiology. Circulation. 1996;94:1147- 66.
- Simpson C, Dorian P, Gupta A, et al. Assessment of the cardiac patient for fitness to drive: Drive subgroup executive summary. Can J Cardiol. 2004;20:1314-20.
- Data from the National Statistical Service of United States of America. [Internet] 2020. Available from: https://www.cdc.gov/heartdisease/ Accessed on 10/10/2020
- National Center for Statistics and Analysis. (March, 2019). 2017 older population fact sheet. (Traffic Safety Facts. Report No. DOT HS 812 684). Washington, DC: National Highway Traffic Safety Administration.
- Data from the Israeli Central Bureau of Statistics.2013. Available from: https:// www.cbs.gov.il/ Accessed on 10.10.2020
- Data from the Israeli Central Bureau of Statistics. 2019. Available from: https://www.cbs.gov.il/en/publications/Pages/2019/Transport-and-Road-Safety-Statistical-Abstract-of-Israel-2019-No-70.aspx
- https://www.fhwa.dot.gov/policyinformation/statistics.cfm Accessed on 22.10.2020
- Zografos TA, Katritsis DG. Guidelines and regulations for driving in heart. Hellenic J Cardiol. 2010;51:226-34.
- Gotfried N. Correlations between driving simulator and paper and pencil test, computerized tests,and driving-on-road test. Unpublished Master Thesis, University of Haifa, Faculty of Social Welfare & Health Sciences, Department of Occupational Therapy. 2007.
- Nasser N. Effects of neurotoxic chemotherapy on cognition and driving safety in patients with malignant tumors with expected long term survival. Unpublished Master Thesis, Tel Aviv University, Occupational Therapy Department. 2019.
- Ware Jr JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical care. 1992;1:473-83.
- Kennedy RS, Lane NE, Berbaum KS, et al. Simulator Sickness Questionnaire: An enhanced method for quantifying simulator sickness. International Journal of Aviation Psychology.1993;3(3):203-20.
- Lee HC. The validity of driving simulator to measure on road driving performance of older drivers. Conference of Australian Institute of Transport Research. 2002.
- Bédard M, Parkkari M, Weaver B. Assessment of driving performance using a simulator protocol: Validity and reproducibility. Am J Occup Ther. 2010;64(2):336–340
- Beker A. The Point System in motor Vehicle Violations: Knesset Research and Information Center Report. 2015.
- Shin YC, Kim SH, Kim DJ, et al. Sternal healing after coronary artery bypass grafting using bilateral internal thoracic arteries: assessment by computed tomography scan. Korean J Thorac Cardiovasc Surg. 2015;48(1):33‐9.
- Austroads. Assessing Fitness to Drive. https://austroads.com.au/__data/assets/pdf_file/0022/104197/AP-G56-17_Assessing_fitness_to_drive_2016_amended_Aug2017.pdf
- Baldock MR J, Mathias J, McLean J, et al. Self-Regulation of Driving and Older Drivers' Functional Abilities. Clin Gerontol. 2006;30;53-70.
- Chen Y, Gélinas I, Mazer B, et al. Personal and Clinical Factors Associated with Older Drivers’ Self-Awareness of Driving Performance. Canadian Journal on Aging/La Revue Canadienne Du Vieillissement. 2020;1-15.