Emergency oral contraceptive use among undergraduate female Mizan campus students of Mizan-Tepi university, south nations nationalities and peoples regional state south west, Ethiopia, 2016
2 Department of Nursing, College of Health Sciences, Mizan-Tepi University, Ethiopia, Email: buchiatuog@gmail.com
Received: 22-Dec-2017 Accepted Date: Jan 18, 2018; Published: 30-Jan-2018
Citation: Yemaneh Y, Sayih A, Niguse W, et al. Emergency oral contraceptive use among undergraduate female Mizan campus students of Mizan-Tepi university, south nations nationalities and peoples regional state south west, Ethiopia, 2016. J Reprod Biol Endocrinol. 2018;2(1):35-40.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Unintended pregnancies are major public health concern in developing countries including Ethiopia. Female university students face unintended pregnancies because most of them are sexually active and exposed to unprotected sporadic premarital sexual intercourse. Emergency contraception is a drug or a device that prevents unintended pregnancy and its consequences. Emergency oral contraceptives are being increasingly used by unmarried young women to prevent unintended pregnancies following unprotected sexual intercourse. However, little is known about Emergency Oral Contraception (EOC) use among female students at higher education in Ethiopia.
Objective: The main objective of this study was to assess the prevalence of Emergency Oral Contraceptive (EOC) use among Mizan-Tepi University, Mizan campus undergraduate regular female student 2016.
Methods: Institution based cross-sectional study was conducted on 324 undergraduate female students of Mizan-Tepi University, Mizan campus. Data were collected from March 1-21, 2017. Study participants were selected using stratified sampling technique. Self-administered pretested structured and semi-structured questionnaire was used to collect the data. Descriptive analysis was applied to describe the Emergency oral contraceptive use.
Results: Regarding utilization of Emergency oral Contraceptives, among those who reported to have sexual intercourse, 78 (82.97%) reported use of Emergency oral Contraceptives and it was 76 (95%) among those who had unprotected sex.
Conclusion and recommendation: There is very high level of Emergency oral Contraceptives use among sexually active female undergraduate students who had unprotected sexual intercourse.
Given that Emergency oral Contraceptives use among female students is very high among those who reported sexual intercourse we recommend that zonal health department, town heath office, Mizan-Tepi University health Science College and Mizan-Tepi University HIV coordination should give reproductive health education, risk of unprotected sex.
Keywords
Emergency contraceptives; Oral
Emergency Contraception (EC) is a birth control that is used after unprotected sex, contraceptive failure and rape. Terms used to describe EC include post-coital contraception and the morning after pill. Emergency contraceptives are intended to provide second chance to prevent pregnancy for women who have been exposed to unprotected sexual intercourse and who don’t wish to become pregnant [1,2].
Emergency Oral Contraceptives (EOC) is a progestin only or pills containing a combination of a progestin and an estrogen. Effectiveness of EOC the progestin only regimen reduces the risk of pregnancy after a single act of sexual intercourse by about 60-93% and the combined regimen by about 56-89%. EOC reduces the risk of pregnancy by up to 95%. With respect to mechanism of action, EC works by preventing fertilization, implantation, tubal transportation of sperm and ovum [1,2].
Although hormonal contraceptives were developed since mid-1920s in the world [3] Emergency Contraceptives (EC) were first introduced to the Ethiopian public sector in 1997G.C [4].
The primary use of Emergency Oral Contraceptive is in reducing the need for abortions and the negative maternal health consequences associated unintended pregnancy [5].
Emergency oral contraceptive is found to be effective if used as soon as possible after unprotected sexual intercourse, especially within 72 h of unprotected sexual intercourse [6]. Lack of health services for young people and limited access to targeted reproductive health care contributes to and exacerbates many of their reproductive health problems. Over a quarter of all pregnant youth and adolescents report that their pregnancies are unplanned, reflecting this populations unmet need for family planning and reproductive health services [2,7].
Unavailability of family planning and reproductive health services has even more serious consequences for countries like Ethiopia where over 65% of its population is under 25 years of age with profound reproductive health needs. As a result, Ethiopian youth face many sexual and reproductive health problems including sexual coercion, unintended pregnancies, abortion, sexually transmitted Infections (STIs) including HIV/AIDS [8].
In response to this growing challenge the government of Ethiopia has introduced several reproductive health intervention targeting adolescents and youth.
One of the interventions to reduce unintended pregnancy and unsafe abortion outlined in the national adolescent and youth strategy is availing Emergency Contraceptive (EC). However, information about EOC use is limited [7].
Globally, there are about 210 million pregnancies each year, some 80 million of these are unintended and one in ten of these pregnancies end in an unsafe abortion. An estimated 529,000 girls and women die from pregnancy-related causes each year worldwide, of which 13% are due to unsafe abortion. It is estimated that two in five unsafe abortions occur among women under age 25 and about one in seven women who have unsafe abortions are under 20 [9,10].
In Africa, among the annual number of induced abortions (6.4 million), only 3% are performed under safe conditions. Eastern African countries contributed nearly 39.1% (2.5 million) of all induced abortions occurred in Africa in 2008, a higher proportion than in any other regions of the continent [11].
Based on the World Health Organization (WHO) estimate the level of Maternal Mortality Ratio (MMR) in Ethiopia is among the highest in the world with 412 maternal deaths per 100,000 live births [12]. One of the interventions to prevent maternal deaths particularly among young people is through preventing unintended pregnancies and abortion through use of Emergency Oral Contraceptive [13].
Most of the pregnancies among students in Ethiopian university are unintended. Unintended pregnancy either ends with unsafe abortion or early child bearing; it has a negative impact on educational progress, future careers and even social interaction of female students by forcing them to drop out of school. On the other hand, this segment of population is tomorrow’s generation in pipeline to take over the responsibilities of socioeconomic development of the country. Thus, they should be protected from unintended pregnancy that could have been considerably prevented by emergency contraception [14-18]. Despite high rate of unintended pregnancies among university students there is low uptake of contraceptive methods including emergency contraceptives [19-22]. So that this study focused on its magnitude and the various factors responsible for Emergency Oral Contraceptive use among Mizan Tepi University Mizan campus students.
Methods
Study design
Institution based descriptive cross-sectional Study design was employed.
Source population
All undergraduate regular female students of Mizan-Tepi University, Mizan campus.
Study population
Randomly Selected undergraduate regular female students of Mizan-Tepi University found during data collection period, Mizan campus, 2016/2017.
Inclusion criteria
The inclusion criteria for this study were all students who were all female students who were:
• Undergraduate
• Regular
In Mizan campus during the study period were included.
Exclusion criteria
The exclusion criteria for this specific study were all undergraduate regular female Mizan campus students of Mizan-Tepi University,
• Who cannot communicate and seriously ill during data collection time.
Sample size determination
The sample size was calculated using a single population proportion formula using the prevalence of emergency contraceptive use assumed to be 44% which is taken from research done in Wachamo University, 95% confidence interval and 5% margin of error to get the possible sample size n=378. Since the source population is less than 10,000 we have used the correction formula:
nf=n/1+(n/N)
Then, adding 10 % (31.1) non-response rate finally gave us total sample size of 342.
Sampling technique
Stratified sampling technique was used to select study participants from the source population.
Sampling procedure
First the students were divided in to two practical strata, which were health Science College and other colleges. The total sample size was allocated to each stratum, which was to college of health science and other colleges based on Proportional to their Size (PPS) of female students in each college. Again with in each college, we have merged each department within the college based on probability proportional to number of students found in each department. Finally study units were selected from each department using Simple Random Sampling (SRS) technique.
Data collection method and data quality management
Structured and semi-structured questionnaire was prepared in English after reviewing literature of similar survey that have been carried out previously, including Ethiopia Demographic Health Survey (EDHS). Data was collected using self-administered questionnaire. To maintain the quality of data, structured and semi-structured questionnaire was prepared in English language and then translated to Amharic language. To check the clarity, consistency, skipping pattern and order of questions, questionnaire was pre-tested on 5% [17] of the calculated sample size in Tepi campus computer science students. Then the questionnaire was modified based on information obtained from pre-test results. Data collection period were in the morning at the weekend after giving orientation. The questionnaire was self-administered since it is sensitive and majorly focused on private issue. Then each questionnaire was checked for completeness and provision of necessary data by principal investigators on daily basis
Data analysis
The collected data was cleared, and checked for completeness. Data was tallied and analyzed manually using digital calculator and computer. Additionally, the result of the study was presented using tables, different charts and texts.
Ethical consideration
A formal letter was obtained from Mizan-Tepi University, College of health science Department of Nursing. The purpose of study was explained to the study subject at the time of data collection and verbal consent was taken from participants to conform whether they are willing to participate. Those who are not willing to participate were given the right to do so. Confidentiality of respondents was ensured throughout the research process.
Results
Socio demographic characteristics
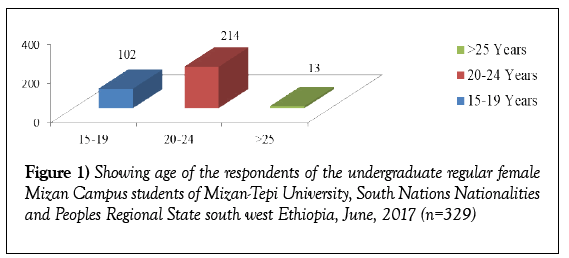
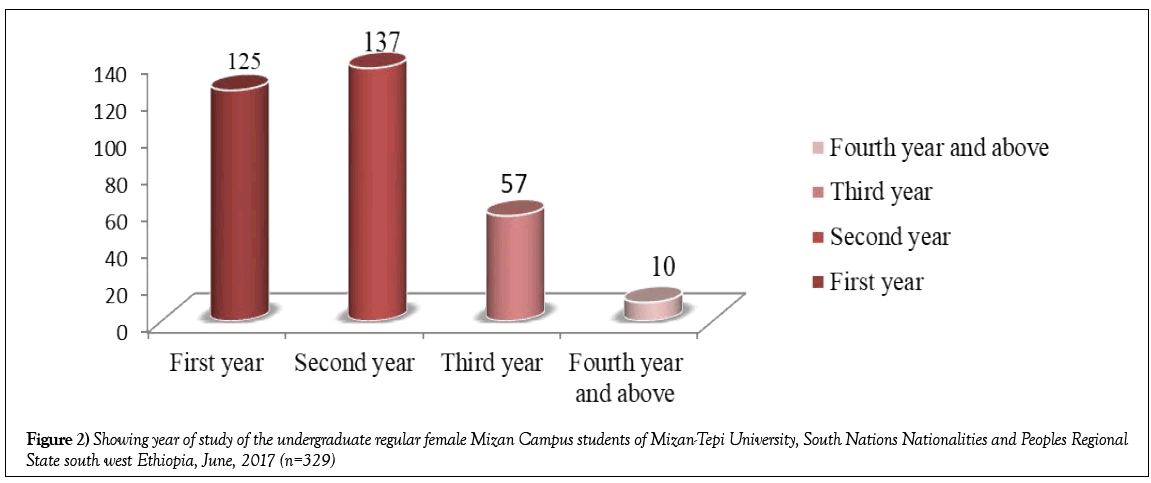
A total of 329 female students completed the questioner making a response rate of 329 (96.54%).Concerning the age, 214 (65.54%) of respondents are between 20-24 age group. More than half (53.19%) of the respondents were followers of the Orthodox Christianity followed Protestant and Muslim which accounted for 75 (22.79%) and 55 (16.71%), respectively. Regarding the marital status of the respondents 318 (96.65%) was single. With respect to current place of residence about 315 (95.74%) of the participants reported that they live inside the university dormitory (Figures 1 and 2 and Table 1).
| Variables | Number | Percent |
|---|---|---|
| Field of study | ||
| Other college | 250 | 75.98% |
| Health college | 79 | 24.04% |
| Religion | ||
| Orthodox | 175 | 53.19% |
| Protestant | 75 | 22.79% |
| Muslim | 55 | 16.71% |
| Catholic | 20 | 6.07% |
| Others | 4 | 1.20% |
| Ethnicity | ||
| Amhara | 115 | 34.95% |
| Oromo | 110 | 33.95% |
| Wolyita | 37 | 11.24% |
| Gurage | 25 | 7.59% |
| Tigray | 22 | 6.68% |
| Others | 20 | 6.07% |
| Marital status | ||
| Single | 318 | 96.65% |
| Married | 11 | 3.34% |
| Current residence | ||
| In campus | 315 | 95.74% |
| Out of campus with family | 9 | 2.73% |
| Out campus alone | 5 | 1.51% |
Table 1: Socio-demographic characteristics of undergraduate regular female Mizan Campus students of Mizan-Tepi University, South Nations Nationalities and Peoples Regional State, south west Ethiopia, June, 2017 (n=329)
Sexual and reproductive characteristics
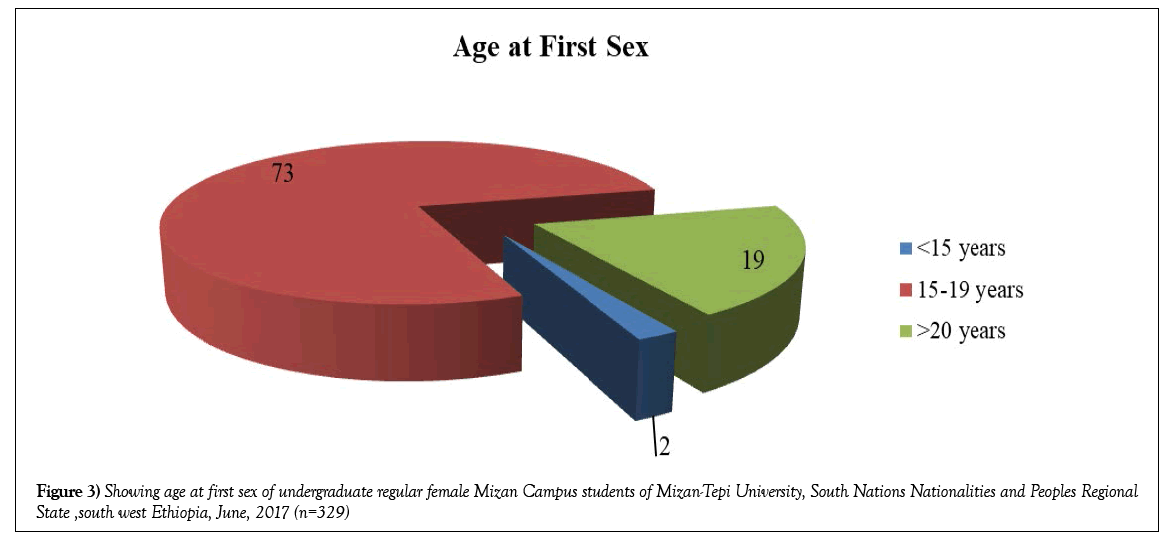
Among the total female students who participated in this study, 94 (28.57%) reported having had sexual intercourse. Of these, 73 (77.65%) had their first sexual intercourse before they were 19 years of age. Among sexually active respondents 80 (85.1%) had unprotected sexual intercourse and 17 (18.08%) had sex with two or more partners. 94 (28.57%) of those who had sexual intercourse, (11.70%) of all study participants were pregnant at least once and most (81.81%) of the pregnancies were unintended. Lack of knowledge about contraception 4 (44.44%), contraceptive failure 2 (22.22%) and forget to take contraceptive 3 (33.33%) were their reported main reasons for unintended pregnancies. The majority (72.72%) of pregnancies were terminated by induced abortion (Figure 3 and Table 2).
| Variables | Number | Percent |
|---|---|---|
| Ever had sex since in the campus (n=329) | ||
| No | 235 | 71.42% |
| Yes | 94 | 28.57% |
| Unprotected sex (n=94) | ||
| Yes | 80 | 85.10% |
| No | 14 | 14.89% |
| Multiple sexual partner (n=94) | ||
| One | 77 | 81.91% |
| Two or more | 14 | 18.08% |
| Frequency of sexual intercourse per week (n=94) | ||
| One time | 56 | 59.57% |
| Two times | 32 | 34.04% |
| Three or more times | 6 | 6.38% |
| Ever had STIs (n=94) | ||
| No | 88 | 93.61% |
| Yes | 6 | 6.38% |
| History of pregnancy (n=94) | ||
| No | 83 | 88.29% |
| Yes | 11 | 11.70% |
| Unintended pregnancy (n=11) | ||
| Yes | 9 | 81.81% |
| No | 2 | 18.18% |
| Experience of induced abortion (n=11) | ||
| Yes | 8 | 72.72% |
| No | 3 | 27.27% |
| Reasons for induced abortion (n=8) | ||
| Fear of discontinuing school | 4 | 50% |
| Fear of parents and family | 2 | 25% |
| Economic problem | 1 | 12.50% |
| Others | 1 | 12.50% |
Table 2: Sexual and reproductive history of undergraduate regular female Mizan Campus students of Mizan-Tepi University, South Nations Nationalities and Peoples Regional State, south west Ethiopia, June, 2017 (n=329)
Use of emergency oral contraception
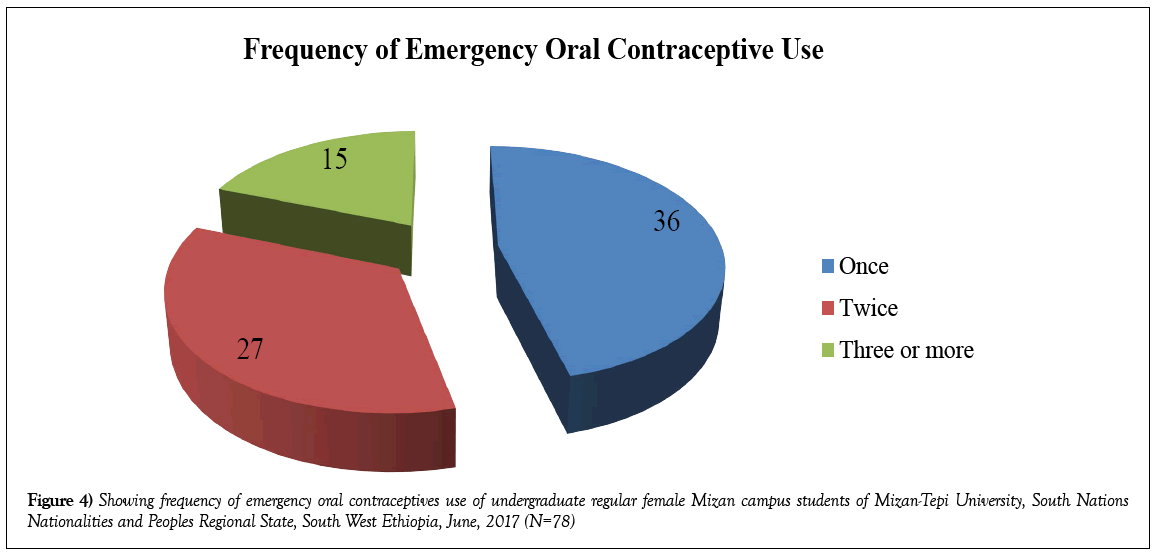
Regarding utilization of Emergency Oral Contraceptives, among those who reported to have sexual intercourse, 78 (82.97%) reported use of Emergency Oral Contraceptives (EOC)and it was 76 (95%) among those who had unprotected sex. From those respondents who were reported use of Emergency Oral Contraceptives (EOC), those from other college and health college are 55 (55.35%) and 26 (27.62%), respectively.
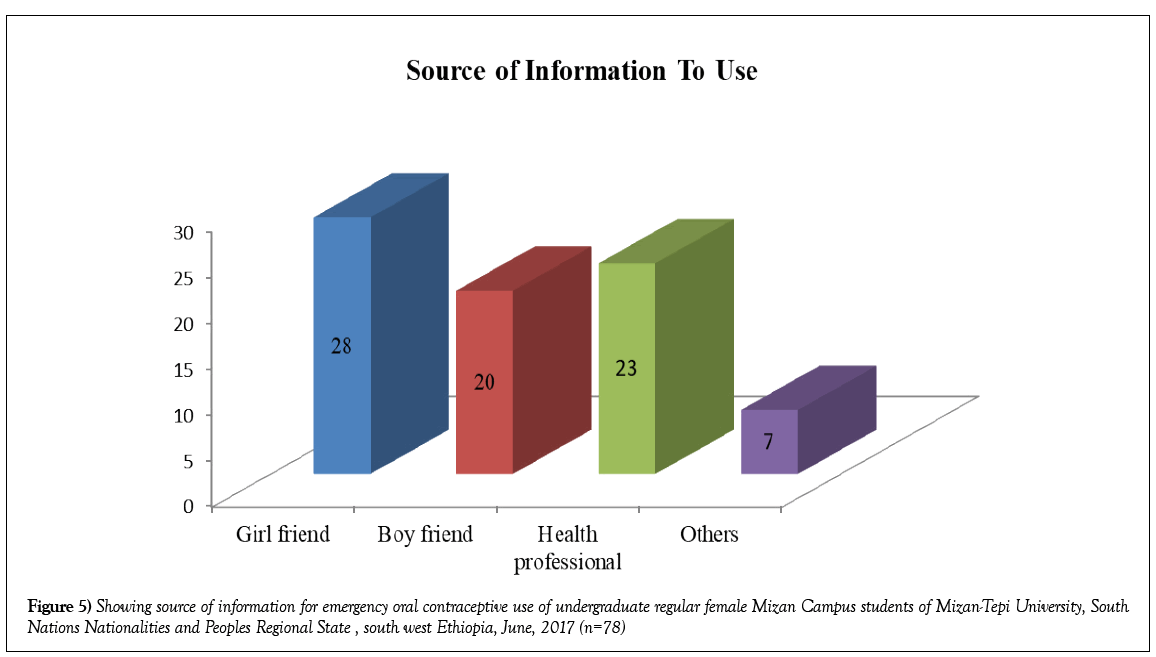
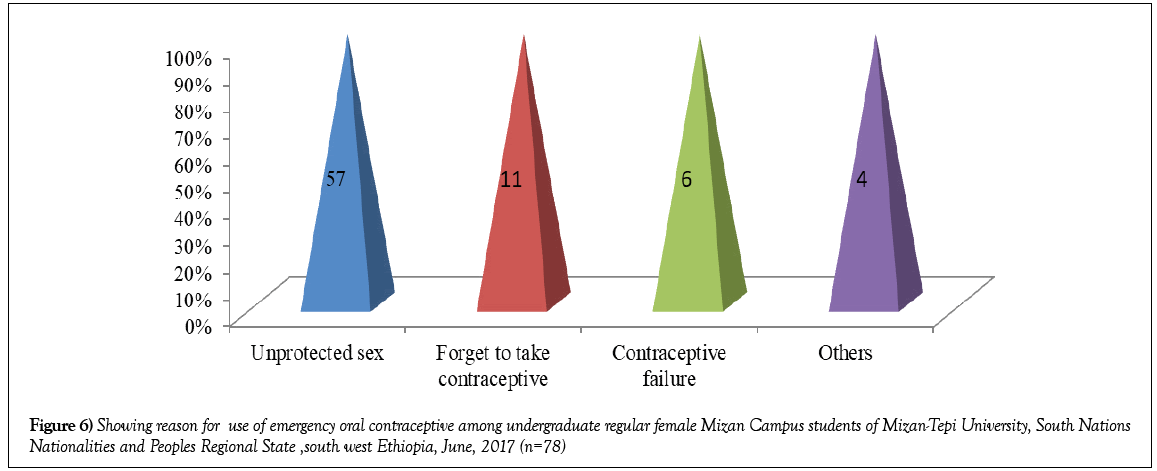
Respondents were asked who told them to use Emergency Oral Contraceptives (EOC). The majority of them (35.89%) mentioned their female friends followed by health professionals (29.48%) and boyfriends (25.64%). Unprotected sexual intercourse (73.07%), forgetting to take contraception (14.10%), failure of contraceptive (7.69%) and others (5.12%) were the main reasons to use Emergency Oral Contraceptives (Figures 4-6).
Discussion
This proportion is very high compared to Emergency Oral Contraceptive use reported by other studies [19,23-25]. The possible reasons for a high Emergency Oral Contraceptive practice observed in the studies might be partially explained by the fact that a higher proportion of sexually active students among the participants in the studies. The study also found that 78 (82.97%) of study participants practiced Emergency Oral Contraceptive since in the campus, which is higher compared to what have been reported by studies among university students in South Africa and Cameroon (21.2%, 7.4%) respectively [26]. The possible explanation for a higher Emergency Oral Contraceptive practice observed in this study might be related to difference in sample size between the two studies and level of awareness as the time of the study goes on might also be another possible explanation. Among the respondents who reported having ever had unprotected sexual intercourse almost all of them reported using Emergency Oral Contraceptive (95%).
In this study about 94 (28.57%) of the students reported that they are sexually active. This result is higher than similar study conducted in Adama and Addis Ababa University among female undergraduate students [18,20]. The difference could be due to cultural variation and economic status among study participants.
Limitations of the Study
The study employed a cross-sectional study design and can’t establish cause and effect associations. This study cannot guarantee that students provided honest answers to the questions, since the survey involved a sensitive matter. Therefore, it is important to remember that the reliability of results of this study is dependent upon the accuracy of the responses.
A prospective study design with follow up could have been more robust method to identify associated factors for Emergency Oral Contraceptive use this couldn’t be used because of the limitation in resource and time.
Conclusion
Emergency Oral Contraceptive use among undergraduate female university students who had reported unprotected sexual intercourse is very high.
There is very high rate of unintended pregnancies and induced abortion among sexually active female university students.
Recommendation
Despite the high use of Emergency Oral Contraceptive among the study participants the fact that relatively high proportions of students are sexually active and do not use barrier methods to prevent STI/HIV is a serious concern.
Use of Emergency Oral Contraceptive among almost all female university students who had unprotected sexual intercourse may indicate the lack of information and access to regular contraceptive methods which are more efficacious.
Given that Emergency Oral Contraceptive use among female students is very high among those who reported sexual intercourse we recommend that zonal health department, town heath office, Mizan Tepi University health Science College and Mizan Tepi University HIV coordination should give reproductive health education, risk of unprotected sex.
To prevent unintended pregnancy among sexually active female university students there is a need to improve reproductive health education and provision of services in the existing student health clinic in the campuses.
The current study employed cross sectional descriptive study design that doesn’t show cause and effect relationship between independent variables and Emergency Oral Contraceptive. Future researchers should consider prospective study with follow up to identify predictors of Emergency Oral Contraceptive use.
Acknowledgement
First and for most we would like to express our deepest gratitude and appreciation to our staffs for their unreserved all rounded, support and enriching comment throughout the research and to Mizan Tepi University, college of health science nursing department for giving us a chance to develop this research and for their scientific suggestions through selection of title. We would like to express our heartfelt gratitude to Mizan-Tepi University Students Academic and Alumni Management Directorate for their cooperation and provision of mandatory information. We would like to give a special gratitude to the entire study participants and the data collectors.
REFERENCES
- Zeiman M. Emergency contraception. Available from http://www.uptodate.com/contents/emergency-contraception [Accessed 10th August, 2015].
- Family planning: A global hand book for health care providers: A WHO family planning corner stone, 2011. Available from apps.who.int/iris/bits ream/pdf [Accessed 18th June, 2016].
- Charlotte E. History and efficacy of emergency contraception: Beyond coca cola. Fam Plan Perspect. 1996;28(2);44-8
- Ethiopian Ministry of health, Family Health Department. An assessment of reproductive health needs in Ethiopia. Research on the introduction and transfer of technologies for fertility regulation. Geneva: WHO, Special program of research, development and research training in human reproduction. 1999. Available from http://www.WHO/RHR/HRP/ITT/99.1pdf [Accessed 18th June, 2016].
- Lemma DA. Emergency contraception in Addis Ababa: Practice of service providers. University of South Africa. 2012.
- Szarewski A, Guilleband J. Contraception: A users giude. 2010.
- Federal Ministry Of Health. National reproductive health strategy in Ethiopia. 2006-2015. 2015. Available from http://www.phe.Ethiopia.org [Accessed 18th June, 2016].
- Altankhuyagiin G, Jane F, James B. Determinants of current contraceptive use and method choice in Mongolia. Journal of Biosocial Science. 2007:6(39)1-17 .
- http://www.who.int/reproductivehealth/publications/unsafe_ abortions/induced_abortion_2012.pdf
- Gettmacher Institute and World Health Organization. Facts on induced abortion worldwide, In brief: Fact sheet. 2012. http://www.gutmacher.org/pubs/fb_IAW.html
- Central Statistical Agency, Ethiopia and ORC Macro Ethiopia. Demographic and health survey (EDHS). Addis Ababa, Ethiopia and Calverton, Maryland, USA: Central Statistical Agency and ORC Macro. 2011.
- WHO, UNICEF, UNFPA. World Bank estimates: Trends on maternal mortality; 1990-2013. Available at http://www.who.int/maternal_child_adolescent/eth.pdf [Accessed on 26th June, 2016].
- Central Statistical Agency. Ethiopian demographic health survey (EDHS). Calverton, Mary kind USA. 2012. Available from http://www.Unicef.org [Accessed 18th June, 2016].
- Both R, Samuel F. Keeping silent about emergency contraception in Addis Ababa: A qualitative study among young people, service provider and key stake holders. Biomed Central. 2014.
- Tilahun D, Assefa T, Belachew T. Predictors of emergency contraception among regular female students at Adama University, Central Ethiopia. Pan Afr Med J. 2011;31.
- Worku A. Knowledge, attitude and practice of emergency contraceptives among female college students in Arba Minch. Ethiop J Health Dev. 2011;25:176-83.
- Tajure N. Knowledge, attitude and practice of emergency contraception among graduating female students of Jimma University, south west Ethiopia. Ethiop J Health Sci. 2010;20:91-7.
- Akani C, Enyindah C, Babutunde S. Emergency contraception: Knowledge and perception of female undergraduates in the Niger delta of Nigeria. Ghana Med J. 2008;42:68-70.
- Tilahun D, Assefa T, Belachew T. Predictors of emergency contraception among regular female students at Adama University, Central Ethiopia. Pan Afr Med J. 2011;31.
- Nibabe WT, Mgushine T. Emergency contraception amongst the female college students: Knowledge, attitude & practice. Afr J Prim Health Care Med. 2014;6(1):538-45.
- Miruts G, Yeman D, Abera K. Factors associated with emergency contraceptive use among female preparatory school students Adwa town, northern Ethiopia. Int J Pharm Sci Res. 2014;5 (10):665-9.
- Palermo T, Black J. Westley E. knowledge and use of emergency contraception: A multicountery analysis. Int Perspect Sex Reprod Health. 2014. Available from http://www.Jstor.org [Accessed 18th June, 2016].
- Haile Mariam GT, Tesfaye T, Melese T, et al. Sexual experience and emergency contraceptive use among female university students; A cross sectional study at Wachamo University, Ethiopia. Biomed Central Res Notes. 2015.
- Hoque ME, Ghuman S. Knowledge, attitudes and practice of emergency contraception among female university students in Kwa Zulu-Natal, South Africa. PLoS One. 2012.
- Ahmed FA, Moussa KM, Petterson KO, et al. Assessing knowledge, attitude and practice of emergency contraception: A cross sectional study among Ethiopian under graduate female students. Biomed Central Public Health. 2012.
- Eugene J, Negassa P, Fomulu N. A survey of knowledge, attitude and practice of emergency contraception among university students in Cameroon. BMC Emerg Med. 2007;7:7.