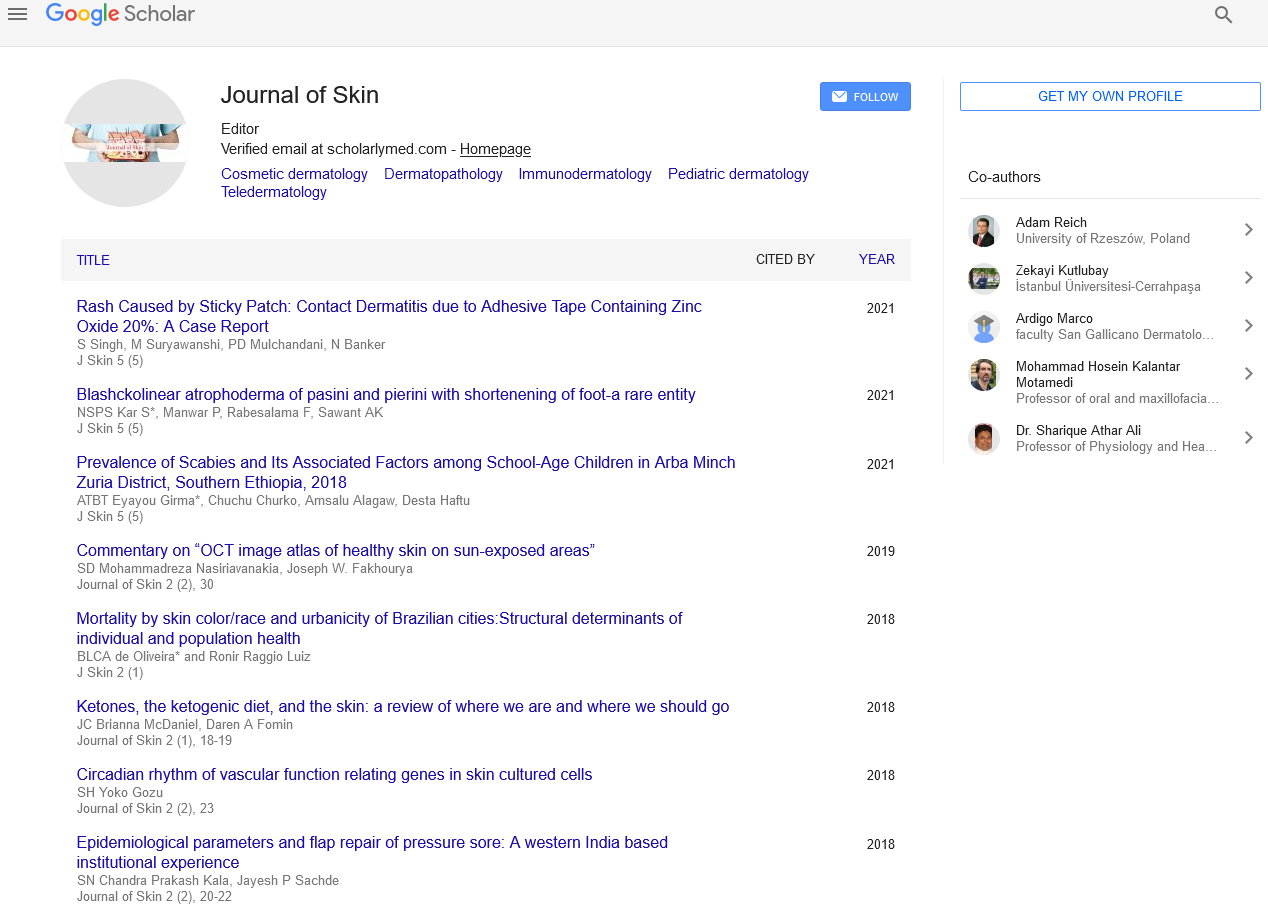
Epidemiological parameters and flap repair of pressure sore: A western India based institutional experience
Received: 10-Jan-2018 Accepted Date: Mar 12, 2018; Published: 19-Mar-2018
Citation: Kala P, Sachde JP, Narayan S. Epidemiological parameters and flap repair of pressure sore: A western India based institutional experience. J Skin. 2018;2(1):20-22
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Pressure ulcers are common complications for long standing hospitalized bed-ridden patients those are not able to move or move very little. In fact, the lesion forms in a skin and muscle region which undergoes a constant pressure between an underlying bone protrusion and a support structure such as a bed or a wheelchair. In this study author have focus epidemiological parameters and on various type of surgical treatment used for pressure, treatment outcome at one year and complication. This study was conducted at the Government Spine Institute at Civil Hospital Ahmedabad from October 2012 to September 2014. An analysis of patient care records of indoor patients of post traumatic spinal cord injury with pressure sore surgery was performed.
Keywords
Pressure sore; Flap repair; Spinal injury
DPressure sores are also described as pressure ulcers, decubitus ulcers and bed sores. Decubitus ulcer is derived from the Latin word ‘decumbere’ which means ‘to lie down’ [1], Means commonly seen over areas with underlying bony prominences when subjected to recumbent position, mainly sacrum, trochanters, heel and occiput, suggest that pressure breakdown of weight bearing areas like the sacral region and ischial tuberosity in lying down and sitting position respectively.
Pressure sores are classified by various systems. The first NPUAP-EPUAP International Pressure Ulcer Prevention and Treatment Guidelines (2009) further revised the staging system for international use by adding the term category/stage, which is frequently used outside the United States. The NPUAP Staging System was evaluated and revised to reflect current scientific and clinical understanding of the etiology of pressure injuries, as well as to clarify and make the system more accurate and easier to use [2]. NPUAP is a modification of Shea’s original classification.
Studies indicate that pressures between 60 and 580 mm Hg during a period of 1 to 6 h may cause a sore. In addition to pressure, shear and friction forces may act in synergy to the development of a sore in undernourished, incontinent, lying or mentally-ill patients. The diagnosis is usually straight forward. Other than routine investigations, MRI or bone biopsy may be occasionally required to diagnose underlying bony involvement [3]. Treatment of pressure sore depends upon the stage. According to the NPUAP classification, the Stage 3 and Stage 4 pressure ulcers that have to be surgically treated. In this study author have focus epidemiological parameters and on various type of surgical treatment used for pressure, treatment outcome at one year and complication [4]. The fundamental surgical principles for the management of pressure sores remain essentially unchanged since the report of Conway and Griffith in 1956. Debridement of the ulcer, underlying bursa and involved bone followed by soft tissue coverage remains the standard approach. The flap used for coverage should be designed as large as possible, with placement of the suture line away from the area of direct pressure; to preserve all future options for coverage, the flap design should not violate adjacent flap territories. The development of musculocutaneous flaps in the 1970s significantly altered the approach to and success of pressure sore reconstruction.
Material and Methods
This study was conducted at the Government Spine Institute at Civil Hospital Ahmedabad from October 2012 to September 2014. An analysis of patient care records of indoor patients of post traumatic spinal cord injury with pressure sore surgery was performed. All the demographic profile data collected for each patient. Only those patients who were medically fit and having hemoglobin more than 10 g/dl and serum albumin more than 3 g/dl were consider for flap coverage. The distribution of patient was done according to the type of treatment, surgical procedure, type of flap and Complications. All patients are followed up to 1 year and complications if any, noted and treated, counseling about life style modification, physiotherapy and nutritional support advised. The collected data analyzed, conclusions drawn and compared with relevant literature.
Results
After evaluating 96 patients (117 sores) within the period from October 2012 to September 2014 through a prospective study, we concluded that: from the epidemiological point of view: age: ranging from 11 to 68 years old, with an average of 32.20 years old (young adults), Maximum patients (59.37%) were from the age group 21-40 years as these are most active sections of the society. Males were predominantly affected as compared to females (5.4:1) as in the current society males are more involved in outdoor activity and high-risk situations. Patients from rural areas (2.1:1) seem to be affected more as compared to those from urban areas. While considering the fact that a higher percentage of population lives in the rural areas along with fewer specialized care institutions in the villages, the above result is open to further research. Risk factors for development of sores: 100% spinal cord injuries, predominance of paraplegics (54.6%), with the majority being due to road traffic accidents (RTA) 70.83%, most of the sores with Class IV lesions 88.50% (Classification according to the National Center of Spinal Cord Injuries Data), largest size sore in Sacral sores in their largest diameter (average 6.8 cm). The site-specific involvement is 40.33% sacral sores, 28.57% trochanteric sores, 23.52% ischial sores, including these sites of sore 10.41% were having combined site involvement and the average number of sores/ patient: 1.22 in this study.
While considering the treatment: Class III and IV 89.58% patient were included in study, all these patients underwent surgical treatment. Mainly the surgical procedures performed by the use of myocutaneous flaps (%). Treatment success rates of Sacral (81.25%), trochanteric sores (76.47%) and were higher than ischial sores (71.42%). In this study the Sores recurrence rate was 21.00%, Out of these 4.2% recurrence was at the same site while 16.8% was at newer sites. The post-operative complications: includes 36.00% for ischial sores, 28.00% for trochanteric sores, and 36.00% for sacral sores out of 25 patient recurrences (Same Site + New site lesions).
Discussion
Paraplegic patients are chronic bed ridden patients totally depended on relative for their activities of daily routine and general care. Special care includes feeding, frequent change in posture; personal hygiene as well as mental and emotional wellbeing needs to be addressed. Bed sores are a result of negligence and further lead to soiling of clothes, infection, osteomyelitis of underlying bone, necrosis of skin, subcutaneous tissue and muscle, loss of protein rich fluid from the body and so on. With early identification of pressure sores, timely and adequate treatment of the condition can be cured. These patients require medical, surgical as well proper nutritional support. Well trained nursing and para clinical staff is absolutely essential. Proper pre and post op physiotherapy is very important to prevent muscle atrophy in these patients. Proper treatment will help to handle with above problems and patients recover well [5,6].
Risk factors involved in the pathogenesis of ulcers may be intrinsic, extrinsic or both. Risk assessment can be performed using either the Braden or the Norton scale. Intrinsic factors relate to patient status. Several changes occur in the aging skin, including slower epidermal turnover and decreased vascularity, subcutaneous adiposity and collagen and elastin content. Consequently, the skin becomes susceptible to injury, infection and delayed wound healing [7].The inflammatory response is also blunted [2]. Impaired or restricted mobility is an intrinsic risk factor, as evidenced by the increased risk for pressure ulcers in patients with cerebrovascular disease, Parkinson’s disease, advanced dementia, contractures and (most commonly) orthopedic injuries. Other diseases that restrict mobility, such as diabetic neuropathy and spinal cord injuries, likewise increase the risk for pressure ulcers [8].
Pressure, friction, shearing and moisture are well recognized extrinsic factors in the pathogenesis of pressure ulcers. Unrelieved pressure appears to be the most necessary requirement for ulcer development. Normal arteriole, capillary and venule pressures are 32, 20 and 12 mm Hg, respectively [8]. Pressure generated under the ischial tuberosities while a person is seated can reach 300 mm Hg and sacral pressure can range from 100 to 150 mm Hg while a person lies on a standard hospital mattress. Excess pressure (i.e., above 32 mm Hg) results in occlusion of capillary flow, causing ischemic injury and extravasations of fluid, cells, and protein. Muscle can be damaged by pressures exceeding 60 mm Hg for more than an hour, although the skin is more resistant [9].
The NPUAP Pressure Ulcer Staging System was refined, beginning with the change in terminology from pressure injury to pressure injury in order to include soft tissue injury without ulceration (Stage 1 and DTPI). The revisions of the NPUAP Pressure Injury Staging System are intended to improve accuracy of pressure injury staging [10].
In the rare instance when a patient presents with a shallow, newly formed pressure sore (grade I or grade II), nonsurgical measures can be used to optimize conditions for wound healing without the need for surgical reconstruction. The primary objective is to secure a clean wound with beefy red granulation tissue at the base and to take steps to prevent sustained pressure over the wound site. Frequent dressing changes with wet-to-dry saline-soaked gauze dressings combined with daily sharp debridement at the bedside of any devitalized tissue and transfer of the patient to an air-fluidized bed or air mattress are the mainstays of treatment. Wound cultures can be helpful in instances of localized infection in trying to decide on topical therapy (e.g., silver sulfadiazine versus mafenide acetate [Sulfamylon]) or in tailoring the treatment of a systemic infection related to the pressure sore [11]. The evaluation for infection by clinical examination appropriate cultures (e.g. blood, tissue) and determining the leukocyte count, with obtaining radiographs, computed tomography scans and radioisotope scans, if osteomyelitis is suspected, performing bone biopsy and culture, if osteomyelitis is suspected.
The fundamental surgical principles for the management of pressure sores remain essentially unchanged since the report of Conway and Griffith in 1956. Debridement of the ulcer, underlying bursa and involved bone followed by soft tissue coverage remains the standard approach [12]. The flap used for coverage should be designed as large as possible, with placement of the suture line away from the area of direct pressure; to preserve all future options for coverage, the flap design should not violate adjacent flap territories. The development of musculocutaneous flaps in the 1970s significantly altered the approach to and success of pressure sore reconstruction [13]. However, despite high rates of flap survival, not all flaps are equally reliable in achieving coverage of the debrided pressure sore wound. Therefore, the most important step for early treatment success is appropriate flap selection. Because pressure sores that fail to heal while the patient is hospitalized virtually never heal after discharge, the immediate postoperative results will dictate future outcomes. Furthermore, the third or fourth option for flap coverage is as important as the primary choice; despite the best of efforts, recurrence rates after pressure sore reconstruction (>50% in the long term) have remained largely unchanged during the past 40 years. Therefore, a rationale for flap coverage designed to treat a patient during the long term is necessary from the time of initial evaluation. Many studies report the most common sites of occurrence to be the ischial (28%), sacrum (17-27%), trochanteric (12-19%) and heel (9-18%). [14] In this study the sequence of sore was respectively 50% at sacral region, 35% at trochanteric region and 29% at Ischial region.
In evaluation of most pressure sores, the wound is frequently underestimated before surgical debridement. Failure to debride the pressure sore site adequately is a significant factor in the overall morbidity that follows attempted flap reconstruction. Injection of a mixture of methylene blue and hydrogen peroxide directly into the wound cavity is helpful in defining the wound dimensions and determining the extent of debridement necessary. The peroxide aids in mechanical cleaning of the wound. Rarely, two different flaps are required to fill a defect. For all insensate patients (e.g. paraplegics, quadriplegics), the bone prominence at the base of the wound is a significant source of pressure sore recurrence; therefore, partial ostectomy is considered in all ischial, sacral, and trochanteric sores. A total unilateral ischiectomy, in an ischial pressure sore, is contraindicated because of the subsequent shift in maximum pressure to the contralateral ischial tuberosity from such an ischial resection (resulting in a high incidence of contralateral ischial pressure sores) [15]. Furthermore, bilateral total ischiectomies place the patient flat on the perineum, which may give rise to urethral fistulas and diffuse perineal ulcerations. In long-standing pressure sores, osteomyelitis may be present within the bone at the base of the wound. Therefore, care must be taken to debride all nonviable bone tissue before the reconstruction. Bone biopsy is indicated at the time of debridement if osteomyelitis is suspected to aid in diagnosis and to direct systemic antibiotic therapy. Bone viability is determined most accurately by active bleeding at the bone surface during operative debridement.
Conclusion
With suitable flap selection and the appropriate short- and long-term sequence of flap use, reconstruction can reliably be performed in a single stage with relatively short-term hospitalization. Furthermore, improved success rates occur when these principles are used. In caring for patients with pressure sores, flap procedures should be planned carefully, and social resources must be provided to reduce the risk of a negative outcome.
Conflict of Interest
Authors have no conflict of interest.
REFERENCES
- Bansal C, Scott R, Stewart D, et al. Decubitus ulcers: A review of the literature. Int J Dermatol. 2005; 44:805-10.
- National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers: Clinical practice guideline. Washington, DC: National Pressure Ulcer Advisory Panel. 2009.
- National Pressure Ulcers Advisory Panel. New 2014 prevention and treatment of pressure ulcers: Clinical practice guideline. 2014.
- Krasner D, Margolis DJ, Ordoña RU. Prevention and management of pressure ulcers. Treatment of chronic wounds. Number 6 in a Series.
- Goode PS, Allman RM. Pressure ulcers. In: Duthie EH Jr, Katz PR, editors. Practice of geriatrics. 3rd ed. Philadelphia: WB Saunders. 1998:228-35.
- Allman RM. Pressure ulcer prevalence, incidence, risk factors and impact. Clin Geriatr Med. 1997;13:421-36.
- Bennett RG. Pressure ulcers. In: Cobbs EL, Duthie EH Jr, Murphy JB, eds. Geriatric review syllabus. Iowa: Kendall/Hunt Publishing Co. 1999:154-9.
- Liao F, Burns’ S, Jan YK. Skin blood flow dynamics and its role in pressure ulcers. J Tissue Viability. 2013; 22:25-36.
- Goode PS, Allman RM. Pressure ulcers. In: Duthie EH Jr, Katz PR, editors. Practice of geriatrics. 3rd ed. Philadelphia: WB Saunders. 1998:228-35.
- Edsberg LE, Black JM, Goldberg M, et al. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised Pressure Injury Staging System. J Wound Ostomy Continence Nurs. 2016; 43:585-97.
- Dai T, Huang YY, Sharma SK et al. Topical antimicrobials for burn wound infections. Recent Patents on Anti-Infective Drug Discovery. 2010;5:124-51.
- Husain T. An experimental study of some pressure effects on tissues, with reference to the bed-sore problem. J Pathol Bacteriol. 1953; 66:347.
- Ger R, Levine SA. The management of decubitus ulcers by muscle transposition-an eight-year review. Plast Rcconstr Surg 1976;58:419.
- Hubay CA, Kiehn CC, Drucker WR. Surgical management of decubitus ulcers in the post-traumatic patient. Am J Surg. 1957;93:205.
- Garber SL, Rintala DH, Rossi CD, et al. Reported pressure ulcer prevention and management techniques by persons with spinal cord injury. Arch Phys Med Rehabil. 1996; 77:744-9.