Evaluation of cannabinoid eye drops on five patients with intractable hypertensive open angle glaucoma
2 Department of sense organs, Faculty of medicine and dentistry, University ‘La Sapienza’, Rome, Italy, Email: alessio.stefanucci@libero.it
3 Sooft Italia Spa, Catania, Italy, Email: salvatore.pezzino@sooft.it
Received: 18-Jan-2018 Accepted Date: Feb 10, 2018; Published: 17-Feb-2018
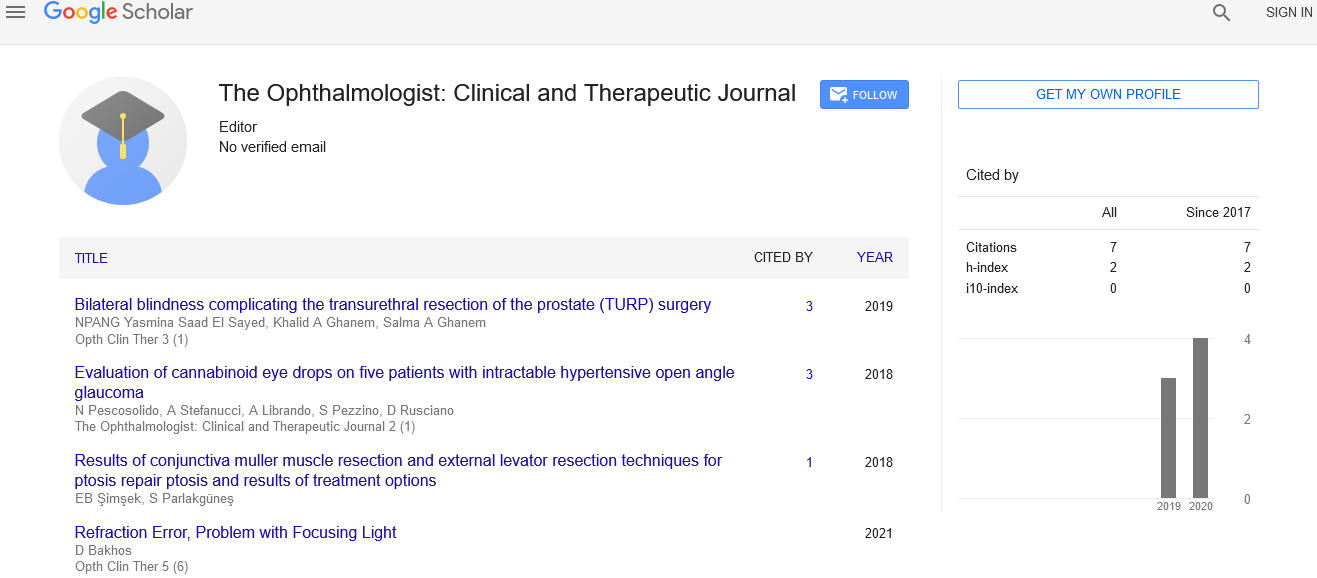
Citation: Citation: Pescosolido N, Stefanucci A, Librando A , et.al. Evaluation of cannabinoid eye drops on five patients with intractable hypertensive open angle glaucoma. Opth Clin Ther. 2018;2(1):1-4.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The aim of the present work was the evaluation of a topic application of cannabinoids in 5 patients affected by late stage open angle glaucoma (OAG) in which both surgical and medical therapies had failed to decrease the intraocular pressure (IOP) to acceptable levels, and were not suitable to further surgical intervention. Eye drops were formulated with Bediol (containing low amounts of tetrahydrocannabinol [THC] and cannabidiol [CBD]), and with Bedrocan (containing higher amounts of THC and lower amounts of CBD). Patients were treated first with Bediol eye drops for 30 days, and after a one-month washout period, they were treated with Bedrocan eye drops for a further 30 days. Four patients did not show any response to both products, while a fifth patient, affected by glaucoma secondary to Fuchs heterochromic iridocyclitis (a rare form of uveitis), showed a relevant antinflammatory effect and IOP decrease in the affected eye. These results suggest a use of THC as an antinflammatory agent in cases of glaucoma secondary to inflammatory events.
Keywords
Antinflammatory; Cannabidiol; Tetrahydrocannabinol
Introduction
Cannabis is a well-known plant, containing many compounds of medical interest, such as cannabinoids (84 different species have been described), and other non-cannabinoid compounds such as terpenes,flavonoids, alkaloids and many others, providing an impressive 483 elements so far described [1].
Among the different cannabinoids, the best known and most abundant are Δ-9-tetrahydrocannabinol (THC), cannabinol (CBN) and cannabidiol (CBD).THC is the main compound responsible for the psychoactive effect of marijuana: by triggering dopamine release in the brain it elicits an euphoric sensation of wellbeing [2].CBN has much lower potency than THC as a psychotropic agent, and CBD lacks psychotropic activity altogether.
The cannabinoid receptors CB1 and CB2 belong to the class of G protein-coupled receptors. CB1 receptors are mainly-but not only-found at central and peripheral nerve terminals, where they inhibit neurotransmitter release, thus also mediating an analgesic effect [3]. CB2 receptors are found on immune cells, where they modulate migration and cytokine release, and may thus exert antinflammatory effects [4].
CB1 receptors are widely present in eye tissues, including those involved in the regulation of intraocular pressure (IOP) [5], which may explain the IOP-decreasing and neuroprotective effects observed after cannabinoid treatment, either systemic or topical [6].
Therefore, given these effects of cannabinoids, the therapeutic use of which is allowed in Italy to treat drug-resistant and inoperable glaucoma (Ministry Decree of November 11,2015), we set out to evaluate the effects of cannabinoids in galenic eye drop formulations on a group of 5 patients having the above requirements.
Case Presentation
Different cannabis extracts were characterized by an HPLC (Shimadzu LC10A) equipped with a Li Chrosphere RP-8 (4x3 mm) pre-column on top of a Li Chrosphere RP-8 column (250x4mm x5μm), linked to two different detectors: a variable length (UV-visible) spectrophotometer, and a mass spectrometer (Finnigan mat LCQ ESI MS). An isocratic elution with acetonitrile: water (80:20) was used at a flow speed of 1 mL/min. The main cannabinoids present in the various extracts were dosed based on calibration curves with the corresponding standards (Table 1).
| Therapeutic cannabis extract | THC % (gr/100ml) |
CBD % (gr/100 ml) |
Cannabis type | Source |
|---|---|---|---|---|
| Bedrocan | 22 | <1 | Sativa | Holland |
| Bedrobinol | 12 | <1 | Sativa | Holland |
| Bediol | 6 | 7.5 | Sativa | Holland |
| Bedrolite | 0.4 | 9 | Sativa | Holland |
| Bedica | 14 | <1 | Indica | Holland |
| FM2 | 8 | 12 | Sativa | Italy |
| FM19 | 19 | <1 | Sativa | Italy |
Table 1: Cannabinoid content of cannabis extracts (THC and CBD content in the different extracts of therapeutic cannabis extracts available in Italy. CBN content is not reported, since it is always below 0.5%. FM: extracts prepared by the Italian Military Pharmaceutical Institute).
Oily-based, preservative-free, formulations of Bedrocan or Bediol, containing different amounts and proportions of cannabinoids (Table 2) and Tween 80 as a surfactant were prepared by the Italian Military Pharmaceutical Institute in Rome. The relative average amounts of THC and CBD range between 0.6 and 0.8 in Bediol, and between 13 and 14 in Bedrocan.
| BEDIOL | BEDROCAN | |||||
|---|---|---|---|---|---|---|
| Patient # | THC (mg/ml) | CBN (mg/ml) | CBD (mg/ml) | THC (mg/ml) | CBN (mg/ml) | CBD (mg/ml) |
| 1 | 3.35 | 0.51 | 5.03 | 20.13 | 0.33 | 1.45 |
| 2 | 3.15 | 0.49 | 4.88 | 23.88 | 0.25 | 1.71 |
| 3 | 4.66 | 0.28 | 6.86 | 18.49 | 0.32 | 1.37 |
| 4 | 6.13 | 0.17 | 7.82 | 18.63 | 0.26 | 1.28 |
| 5 | 5.33 | 0.18 | 6.98 | 18.49 | 0.32 | 1.37 |
Table 2: Cannabinoid content of individual formulations.(Cannabinoid titration of each single formulation given to each patient for the 30 days treatment cycle. Bediol contains low doses and similar amounts of THC and CBD, while Bedrocan contains higher levels of THC and lower levels of CBD. CBN concentration is always at low levels).
Formulations were freshly made soon before use, sterilized by micropore filtration in a laminar flow cabinet and poured into dark bottles to be stored tightly closed at 4°C during treatment time. Experiments on rabbits’ eyes have shown that topical administration of cannabinoids crosses the epithelial barrier and exerts a hypotonising effect [7].
Five patients were enrolled by prof. N. Pescosolido at his private praxis in Rome. They were affected by open angle glaucoma and under maximum tolerated medical therapy (MTMT: consisting of combined treatments with beta-blockers, alfa-agonists, CA inhibitors and prostaglandins), after repeated surgical procedures had failed to control their IOP (Table 3).
| Patient # | Gender | Age (years) | OAG type | Enrolment IOP (mmHg) | |
|---|---|---|---|---|---|
| 1 | Female | 73 | RE: Pseudoexfoliative LE: Hypertensive POAG |
RE: 33 | LE: 13 |
| 2 | Male | 84 | RE: Hypertensive POAG LE: Hypertensive POAG |
RE: 18 | LE: 23 |
| 3 | Male | 52 | RE: Hypertensive POAG LE: Hypertensive POAG |
RE: 23 | LE: 25 |
| 4 | Male | 63 | RE:Hypertensive POAG with macular pucker LE: Hypertensive POAG |
RE: 26 | LE: 30 |
| 5 | Male | 42 | RE:Hypertensive OAG secondary to heterochromic Fuchs iridocyclitis LE: No disease |
RE: 40 | LE: 12 |
Table 3: Characteristics of enrolled patients. (Diseased eyes of all patients had received at least one surgical intervention of trabeculectomy, which failed to decrease the IOP to safe levels, thus glaucoma was still progressing. All patients were under MTMT with several hypotensive drug associations (see text), also failing to completely control the IOP in one or both eyes).
Four patients had primary open angle glaucoma, and one patient had open angle glaucoma secondary to Fuchs heterochromic iridocyclitis in the right eye. Fuchs heterochromic iridocyclitis is a monocular pathology in which the main signs consist of a perikeratic hyperemia treatable with antinflammatory eye drops, diffuse precipitates on the endothelium, minimal Tyndall traces with rare cells in the aqueous humor and irideal hypochromic areas; the evolution of this pathology will trigger irideal heterochromia, cataract and vitreous humor opacity due to the presence of vitreal bodies. The etiopathogenesis of this disease is unknown, although recent data may suggest a link with infant diseases such as rubella [8]. IOP hypertension, often secondary to uveitis, is the critical event that determines a bad prognosis of this pathology, since it is rarely responsive to current medical treatments.
This study was conducted in accordance with the Declaration of Helsinki [9]. After having signed an informed consent, patients were treated first with the topical Bediol formulation, two instillations per day for 30 days. Then, after a 30 day washout period, during which the patients returned to their usual topical therapy, they were treated with the topical Bedrocan formulation, twice per day for a further 30 days. This treatment protocol was chosen in order to keep the same routine that patients were following with their usual treatments. A 30-day washout period is considered enough, since it has been shown that the persistency of cannabinoids in the urine is around 180 days [10]. IOP measurements by Goldman applanation tonometry and ophthalmoscopy with a slit lamp were performed in the morning (at around 9:00 a.m.) before and after each treatment cycle. Such procedure was considered to be adequate to establish whether the new treatment gave a useful clinical response, or no advantage over the old treatments was evident.
Table 4 reports the IOP values of the five patients measured at enrolment, and after each treatment cycle.
| Patient # | RIGHT EYE IOP (mmHg) | LEFT EYE IOP (mmHg) | ||||||
|---|---|---|---|---|---|---|---|---|
| T0 | BEDIOL | WASHOUT | BEDROCAN | T0 | BEDIOL | WASHOUT | BEDROCAN | |
| 1 | 33 | 33 | 27 | 26 | 13 | 13 | 13 | 11 |
| 2 | 18 | 14 | 13 | 18 | 23 | 31 | 24 | 28 |
| 3 | 23 | 23 | 23 | 23 | 25 | 23 | 23 | 19 |
| 4 | 26 | 30 | 19 | 19 | 30 | 38 | 25 | 26 |
| 5 | 40 | 41 | 40 | 33 | 12 | 10 | 12 | 12 |
Table 4: IOP values of enrolled patients. (IOP values measured by Goldman applanation tonometry at enrolment (T0), after 30 days of Bediol treatment, at the end of the washout period and then after a further 30 days of Bedrocan treatment. Relevant variations of IOP are highlighted in bold).
None of the patients showed an IOP decrease after Bediol treatment; rather, 2 patients had an IOP increase in their left eye. Bedrocan treatment too did not result in an IOP decrease in 4 patients, while the patient with Fuchs heterochromic iridocyclitis and untreatable hypertension in the right eye, showed a 20% IOP decrease, with an improvement of the inflammatory condition of the eye, as evidenced by ophthalmoscopy (not shown).
Decreased vision, due to macular involvement or hemorrhage, was noted by 18% of patients. Moreover, retinal detachment was rare and only found to be responsible for vision loss in two cases. Intriguingly, in cases with documented visual acuity, approximately 44% of patients had normal vision and only 13% of patients had visual acuity less than 20/200. Poor visual acuity was usually associated with macular involvement of the tumor as well as complications, such as retinal hemorrhage. Strabismus was reported in 11% of cases, while diplopia was identified in only 2 out of 96 patients. However, the galenic formulations could not be given as continuative therapy because of their experimental nature. Therefore, at the end of treatment periods, patients returned to their usual therapy.
DISCUSSION
IOP modulation by cannabinoids has been reported in rabbits [11] and in humans after systemic or topical cannabinoid treatment or marijuana smoking [12]. In 1980 Merritt and collaborators reported that inhalation of cannabis induced increased heart rate and decreased blood pressure, followed by an IOP decrease [13]. However, further occurrences of orthostatic hypotension, tachycardia, palpitations and psychotic effects discouraged the use of cannabis in glaucoma treatment. The same group [14] then tried a topical administration of THC (0.05% and 0.1% shown to be effective in rabbits) dispersed in mineral oil on 6 glaucoma subjects, however, there was no response. In 2002 a study was published [15] describing 9 glaucomatous subjects treated with either inhaled or oral THC. All 9 patients showed an initial response to THC treatment, which, however, was not long-lasting, while the collateral effects induced all patients to discontinue the treatment within 9 months from enrolment. Further studies also suggested that THC, either by systemic or topic administration, did not seem an efficient treatment for IOP control of glaucoma patients [12].
The possible effects of cannabinoids in the treatment of glaucoma is not limited to IOP control, since THC and CBD have been shown to also possess neuroprotective effects on retinal ganglion cells (RGC) due to their ability to inhibit toxic peroxynitrite formation on over stimulation of the NMDA glutamate receptor, a common mechanism triggering RGC death in glaucoma [6,16]. Moreover, LPS induced inflammatory reactions in Muller cells or in microglial cells is efficiently blunted by an agonist of cannabis receptors CB1 and CB2 such as the 2-Arachidonoyl glycerol (2- AG) [17] or by CBD [18], resulting in a decrease of pro-inflammatory cytokines and an increase of anti-inflammatory cytokine secretion.
Therefore, the failure of cannabinoid treatment on the 4 patients with POAG, and its moderate success on the patient with Fuchs heterochromic iridocyclitis is in line with the expectation that such treatment, used topically at the indicated doses, does not have a strong effect on the IOP control system (AH production and outflow). On the other hand, it may have a relevant antinflammatory effect, mainly due to the THC component (predominant in Bedrocan), finally resulting in an IOP decrease in the patient in which ocular hypertension was secondary to uveitis.
We do not have an explanation for the IOP increase observed in one eye only of 2 patients after Bediol treatment. Being only monolateral, it is unlikely to be a hypertensive effect of the product; rather, it might be that the product itself is not effective on IOP regulation, and that the suspension of the regular topical treatments resulted in such an increase.
In conclusion, we believe that these results pave the way for further studies that are necessary to address more precisely the antinflammatory and neuroprotective roles of cannabinoids (or their analogues, such as endogenous anandamide or synthetic palmitoyl-ethanol-amide) in the treatment of ocular pathologies by topical administration. This drug delivery method maximizes the therapeutic effects on eye structures, and minimizes undesired systemic effects.
Acknowledgement
Critical English proofreading of the manuscript by Dr.Antony Bridgewood is acknowledged.
REFERENCES
- Grotenhermen F, Russo E. Cannabis and cannabinoids: pharmacology, toxicology, and therapeutic potential. Haworth Integrative Healing Press 2002.
- Kuepper R, Morrison PD, van Os J, et al. Does dopamine mediate the psychosis-inducing effects of cannabis A review and integration of findings across disciplines. Schizophr Res. 2010;12(1-3)1:107-17.
- Rahn EJ, Hohmann AG. Cannabinoids as pharmacotherapies for neuropathic pain: from the bench to the bedside. Neurotherapeutics. 2009;6(4):713-37.
- Nagarkatti P, Pandey R, Rieder SA, et al. Cannabinoids as novel anti-inflammatory drugs. Future Med Chem .2009;1(7):1333-49.
- Yazulla S. Endocannabinoids in the retina: from marijuana to neuroprotection. Prog Retin Eye Res.2008;27(5):501-26.
- I Tomida, Pertwee RG , Azura BA. Cannabinoids and glaucoma. Br J Ophthalmol. 2004;88 (5):708-13.
- Green KE, Kearse CE. Ocular penetration of topical Delta9-tetrahydrocannabinol from rabbit corneal or cul-de-sac application site. Curr Eye Res 2000;21(1):566-70.
- tenBerge JC, van Daele PL, Rothova A. Rubella Virus-associated Anterior Uveitis in a Vaccinated Patient: A Case Report. Ocul Immunol Inflamm 2016;24(1):113-4.
- World Medical Association.World Medical Association Declaration of Helsinki:ethical principles for medical research involving human subjects. JAMA 2013; 27(20):2191-4.
- Huestis AM . Human Cannabinoid Pharmacokinetics. Chem Biodivers.2007;4(8):1770-804.
- ElSohly MA, Harland EC, Benigni DA, et al. Cannabinoids in glaucoma II: the effect of different cannabinoids on intraocular pressure of the rabbit. Curr Eye Res.1984;3:841-50.
- Panahi Y, Manayi A, Nikan M, et al. The arguments for and against cannabinoids application in glaucomatous retinopathy. Biomed Pharmacother 2017; 86:620-627.
- Merritt JC, Crawford WJ, Alexander PC. Effect of marihuana on intraocular and blood pressure in glaucoma. Ophthalmology.1980;87(3):222-8.
- Merritt JC, Perry DD, Russell DN, et al. Topical delta 9-tetrahydrocannabinol and aqueous dynamics in glaucoma. J Clin Pharmacol 1981;21(8-9): 467S-471S.
- Flach JA . Delta-9-tetrahydrocannabinol (THC) in the treatment of end-stage open-angle glaucoma. Trans Am Ophthalmol Soc. 2002;100:215-22.
- El-Remessy AB, Khalil IE, Matragoon S,et al. Neuroprotective effect of (-)Delta9-tetrahydrocannabinol and cannabidiol in N-methyl-D-aspartate-induced retinal neurotoxicity: involvement of peroxynitrite. Am J Pathol.2003;163(5):1997-2008.
- Krishnan G, Chatterjee N. Endocannabinoids alleviate proinflammatory conditions by modulating innate immune response in muller glia during inflammation. Glia.2012;1(11):629-45.
- Liou GI, Auchampach JA, Hillard CJ, et al. Mediation of cannabidiol anti-inflammation in the retina by equilibrative nucleoside transporter and A2A adenosine receptor. Invest Ophthalmol Vis Sci.2008;49(12):5526-31.