Exercise-based cardiac rehabilitation in patients with acute coronary syndromes
Received: 01-Oct-2020 Accepted Date: Nov 05, 2020; Published: 12-Nov-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
INTRODUCTION: Cardiac rehabilitation is a comprehensive program of patient evaluation, risk factor reduction, physical activity, and longitudinal care designed to reduce the effects of cardiovascular disease, and is an effective means of mitigating disease and disability. METHODS: The study was conducted on 50 patients presented by acute coronary syndrome. They were divided into group A, who were subjected to 8-weeks exercise based cardiac rehabilitation program using treadmill according to the Modified Bruce protocol, and group B who were given adequate medication. The outcomes of the participants included, triglyceride, HDL-cholesterol, LDL-cholesterol, HA1c, blood pressure, HR, EF, and METS. All parameters were measured before and after the exercise program. RESULTS: The intervention and control groups were similar at baseline. At the end of the study, the rehabilitation group showed a significant reduction in both SABP and DABP (p=0.001), heart rate (p= 0.001), significant reduction in triglycerides (p=0.004), LDL-C (p=0.006), and increase in HDL-C (p=0.004) and significant increase in functional capacity measured in METS (p= 0.001). Blood pressure and heart rate decreased significantly in control group with no significant change in lipid profile. HbA1c and left ventricular ejection fraction did not show significant change in both intervention and control groups. DISCUSSION: Comprehensive cardiac rehabilitation and secondary prevention programs were able to causes significant improvement of cardiovascular risk factors and functional capacity through optimization of medical treatment, risk factor control, prescribed exercise training and increasing physical activity.
Keywords
Cardiac rehabilitation; Acute coronary syndrome; Clinical cardioogy
Abbreviations
ACS: Acute Coronary Syndromes; UA: Unstable Angina; STEMI: ST Segment Elevation Myocardial Infarction; CHD: Coronary Heart Disease; ACEI: Angiotensin Converting Enzyme Inhibitors; ICD: Implantable Cardioverter Defibrillator; HOCM: Hypertrophic Obstructive Cardiomyopathy; CVD: Cardiovascular Disease; ECG: Electrocardiogram; HR: Heart Rate; BP: Blood Pressure; HRmax: Maximal Heart Rate; HRR: Heart Rate Reserve; RPE: Rate of Perceived Exertion; LDH: Low Density Lipoprotein; HDL: High Density Lipoprotein; TG: Triglycerides; SABP: Systolic Arterial Blood Pressure; DABP: Diastolic Arterial Blood Pressure; HgA1c: Glycosylated Haemoglobin; EF: Ejection Fraction; LVEF: Left Ventricle Ejection Fraction; Mets: Metabolic Equivalent Task; CHD: Coronary Heart Disease
Introduction
Acute, regional reduction in the coronary blood flow, resulting in myocardial ischaemia or necrosis describes acute coronary syndromes (ACS) which are a spectrum of clinical manifestations, including unstable angina (UA), non-ST segment elevation myocardial infarction, ST segment elevation myocardial infarction (STEMI) and sudden cardiac death [1]. Coronary heart disease (CHD) is a major cause of death and disability worldwide [2]. Each year more than 2.5 million hospitalizations worldwide are caused by acute coronary syndromes [3]. In Egypt, no accurate registries are available despite the overwhelming increase in the number of ischemic heart disease patients and the change in the natural history of the disease affecting young age and women in addition to the aggressive nature in many patients [4].
Guidelines for management of ACS patients recommend the prescription of antiplatelet drugs, statins, angiotensin converting enzyme inhibitors (ACEI) and involvement in a cardiac rehabilitation program at discharge [5]. Nowadays, rehabilitation programs constitute an important component of the contemporary management of patients with various presentations of heart diseases and should be conducted for long term care [6].
Cardiac rehabilitation programs include exercise training, and lifestyle modifications. The latter include diet control, smoking cessation, physical activity, and encouragement of adherence to medical therapy [7].
The main aims of rehabilitation programs are increasing the trend of secondary prevention, decreasing hospital readmission and mortality, improving lipid profiles and quality of life [8].
Methods
Patient selection
This prospective study included 50 patients with acute coronary syndrome: 25 patients who were enrolled in an 8 week, medically- supervised, tailored, exercise training group A, the intervention group) and 25 patients who did not undergo exercise training (group B, control group). Patients were selected from the Cardiology department, Tanta University Hospital during the period from May, 2015 to December, 2015.
None of the study participants were suffering from: heart valve surgery, cardiac resynchronization therapy or implantable cardioverter defibrillators (ICD), active pericarditis or myocarditis, symptomatic valvular heart disease, contraindication to exercise (e.g. severe aortic stenosis, severe HOCM), uncontrolled congestive heart failure, history of sustained ventricular arrhythmia, atrial fibrillation, physical or mental disability incompatible with exercise training, hepatic and/or renal failure, EF less than 40%.
Methods and interventions
All the study participants were subjected to the follow: 1) full clinical history including history of CVD risk factors (smoking, hypertension, diabetes, dyslipidemia, dietary habits and family history of cardiac disease), 2) thorough physical examination, 3) 12 lead ECG, 4) laboratory investigations (total cholesterol, low density lipoprotein cholesterol, high density lipoprotein cholesterol, triglycerides, fasting and post prandial blood glucose, HbA1c, complete blood picture, liver function tests. renal functions), 5) patient education (including the importance of control of risk factors, hazards of smoking, nutritional education and importance of physical activity) and 6) a symptom limited exercise test using treadmill according to the Modified Bruce protocol [9], to assess the functional capacity, hemodynamic adaptation to maximal and sub maximal levels of exercise, heart rate (HR) and blood pressure (BP), and cardiac arrhythmias induced or worsened by exercise. The test was repeated for all patients after 8 weeks of medication or exercise-based rehabilitation program.
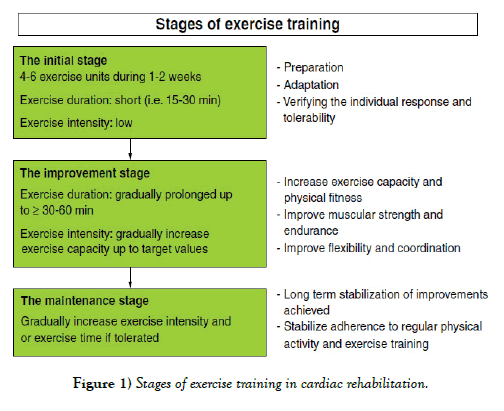
An individualized exercise prescription protocol was tailored for each of Group A patients. They exercised twice weekly for a period of 8 weeks at 60-75% of maximal heart rate (HRmax) or 40-60% of Heart rate reserve (HRR) (maximum heart rate – resting heart rate) (Figure 1) [10]. The Borg Scale (rate of perceived exertion, RPE) was used to subjectively assess how the individual perceived the intensity of the performed exercise on a scale from 6 to 20 (Figure 2) [10]. All the patients were evaluated after 8 weeks by: measuring the blood pressure, heart rate assessment, lipid profile (Triglyceride, LDL-c and HDL-c), HbA1c, ejection fraction evaluation and functional capacity evaluation.
Statistical Analysis
Results were expressed as means ±SD. Analysis of the data was performed by using the computer program SPSS version 20. Unpaired student t-test was used to test significance between two groups in quantitative data. P value < 0.05 was considered statistically significant. The chi-square test was used for comparison of qualitative data.
Results
Demographic data of participants
The study was conducted on 50 ACS patients, 47 males and 3 females with their ages ranging from 45-65 years. The patients were subdivided into two groups, 25 patients each. Group A patients (23 males and 2 females with a mean age 54.44 ± 3.63 years) underwent an 8 weak program of supervised exercise training using treadmill machine and group B (24 males and one female with a mean age 55.24 ± 4.68 years) who did not undergo exercise training and served as a control group.
Effect of exercise on clinical risk factors and cardiac parameters
The studied clinical risk factors and cardiac parameters of the studied groups before and after the 8-weeks exercise program in group A patients or medical treatment in group B participants are summarized in Tables 1 and 2.
TABLE 1
Distribution of the studied parameters in Group A patients before and after 8 weeks exercise-based cardiac rehabilitation.
| Group A | Range (mean ± SD) | P value | ||
|---|---|---|---|---|
| SABP | Before | 20-170 (143 ± 11.9) | 0.001* | |
| After | 80-153 (124.92 ± 16.87) | |||
| DABP | Before | 80-135 (91.2 ± 15.09) | 0.001* | |
| After | 70-95 (78.4 ± 6.73) | |||
| HR | Before | 70-95 (82.84 ± 5.74) | 0.001* | |
| After | 65-80 (72.48 ± 4.12) | |||
| LDL | Before | 80-200 (134.4 ± 31.88) | 0.006* | |
| After | 75-170 (110.92 ± 25.00) | |||
| HDL | Before | 27-53 (34.32 ± 5.91) | 0.004* | |
| After | 31-46 (38.64 ± 4.11) | |||
| TG | Before | 90-220 (153.64 ± 25.76) | 0.016* | |
| After | 78-197 (135.68 ± 25.20) | |||
| HbA1c | Before | 6.5-9 (7.48 ± 0.93) | 0.618 | |
| After | 6.5-9 (7.32 ± 0.71) | |||
| Group A | Range (mean ± SD) | P value | ||
| EF (%) | Before | 45-68 (56.4 ± 6.57) | 0.966 | |
| After | 45-69 (56.48 ± 6.58) | |||
| METS | Before | 6-9 (7.08 ± 0.81) | 0.001* | |
| After | 7-11 (8.72 ± 1.1) | |||
TABLE 2
Distribution of the studied parameters in Group B patients before and after 8 weeks of medications.
| Group B | Range (mean ± SD) | P value | ||
|---|---|---|---|---|
| SABP | Before | 110-160 (137.8 ± 11.91) | 0.001* | |
| After | 90-140 (124.60 ± 15.34) | |||
| DABP | Before | 70-140 (91.00 ± 16.77) | 0.002* | |
| After | 70-85 (78.4 ± 2.69) | |||
| HR | Before | 70-90 (80.60 ± 4.86) | 0.001* | |
| After | 70-80 (80.60 ± 3.73) | |||
| LDL | Before | 85-155 (110.12 ± 17.55) | 0.455 | |
| After | 83-145 (106.44 ± 16.99) | |||
| HDL | Before | 27-40 (31.04 ± 2.73) | 0.080 | |
| After | 29-40 (32.40 ± 2.65) | |||
| TG | Before | 79-200 (133 ± 32.67) | 0.262 | |
| After | 70-180 (123.2 ± 28.17) | |||
| HbA1c | Before | 6.5-9 (7.32 ± 0.71) | 0.278 | |
| After | 6.5-8.5 (7.06 ± 0.51) | |||
| EF (%) | Before | 38-65 (51.12 ± 5.93) | 0.228 | |
| After | 37-65 (49.00 ± 6.34) | |||
| METS | Before | 6-8 (6.84 ± 0.75) | 0.168 | |
| After | (6.48 ± 1.05) | |||
Regarding the effect of exercise training program on the clinical risk factors, there was a statistically significant reduction in SABP from 143.00 ± 11.90 mmHg to 124.92 ± 16.87 mmHg (p value=0.001). Similarly, Group B patients showed a significant reduction in SABP from 137.80 ± 11.91 to 124.60 ± 15.34 (p value=0.001) after medical treatment. Both exercise and medications significantly reduced DBP (from 91.20 ± 15.09 to 78.40 ± 6.73, P=0.001 in group A and from 91.00 ± 16.77 to 79.80 ± 2.69, P =0.002 in Group B.
A significant HR reduction was observed following exercise training from 82.84 ± 5.74 to 72.48 ± 4.12 (P=0.001), and from 80.60 ± 4.86 to 74.20 ± 3.73 (P=0.001) in patients on medical treatment.
As regards serum lipids, exercise-based rehabilitation significantly reduced LDL (from 134.40 ± 31.88 to 110.92 ± 25.00, p=0.006) and TG (from 153.64 ± 25.76 to 135.68 ± 25.20, p=0.004) and significantly increased HDL (from 34.32 ± 5.91 to 38.64 ± 4.11, p=0.004) compared to a non-significant reduction in LDL (from 110.12 ± 17.55 to 106.44 ± 16.99, p-value=0.455) and TG (from 133.00 ± 32.67 to 123.20 ± 28.17, p=0.262) and a non-significant increase in HDL (from 31.04 ± 2.73 to 32.40 ± 2.65, p=0.080) in group B patients.
HbA1c did not change significantly in both groups (reduction in group A following the exercise program from 7.48 ± 0.93 to 7.32 ± 0.71 [p=0.618], and reduction in group B from 7.32 ± 0.71 to 7.06 ± 0.51, p =0.278). Similarly, EF did not show significant improvement in both groups (negligible change in group A from 56.40 ± 6.57 to 56.48 ± 6.58, p=0.966 and from 51.12 ± 5.93 to 49.00 ± 6.34, p-value=0.228 in group B).
As regards METS, it has been significantly increased by the end of the 8-weeks exercise program from 7.08 ± 0.81 to 8.72 ± 1.10 (p-value=0.001), in contrast, group B showed a decrease from 6.84 ± 0.75 to 6.48 ± 1.05 which was statistically non-significant (p-value=0.168) following 8 weeks of adequate medication.
Comparison of the change in studied parameters before and after exercise and/or medication between both groups
Comparison of the change in studied risk factors and cardiac parameters between both groups are summarized in Table 3.
TABLE 3
Comparison of the change in studied parameters between both groups.
| Parameters | The change in the parameter in group A, range (mean ± SD) | The change in the parameter in group B, range (mean ± SD) | P value |
|---|---|---|---|
| SABP | 3-70 (18.08 ± 15.96) | 0-60 (13.20 ± 16.51) | 0.293 |
| DABP | 5.0 – 65.0 (12.80 ± 14.94) | 0.0 - 60.0 (11.20 ± 15.76) | 0.714 |
| HR | 0.0 – 20.0 (10.36 ± 4.96) | 0.0 - 15.0 (6.40 ± 3.39) | 0.002* |
| LDL | 5-47 (23.48 ± 12.74) | -14.0 - 11.0 (3.68 ± 6.79) | 0.001* |
| HDL | -10.0 – 9.0 (4.32 ± 3.38) | -1.0 - 5.0 (1.36 ± 1.44) | 0.001* |
| TG | 5.0 – 44.0 (17.96 ± 8.96) | -22.0 - 30.0 (9.80 ± 11.08) | 0.006* |
| HbA1c | 0.0 – 0.80 (0.25 ± 0.29) | -0.20 - 0.70 (0.14 ± 0.24) | 0.163 |
| EF % | -4.0 – 3.0 (0.08 ± 1.35) | -6.0 - 3.0 (-2.12 ± 2.11) | 0.001* |
| METS | 1.0 – 3.0 (1.64 ± 0.64) | -2.0 - 1.0 (-0.36 ± 0.70) | 0.001* |
Comparing the change in the studied risk factors and cardiac parameters induced by exercise-based rehabilitation in group A to that induced by medication alone in group B.
The reduction in SABP (18.08 ± 15.96 and 13.20 ± 16.51 in group A and group B respectively, p=0.293), and in DABP (12.80 ± 14.94 and 11.20 ± 15.76 in group A and group, respectively, p=0.714) between groups A and B was non- significant.
The difference in HR reduction between groups A & B was statistically significant (10.36 ± 4.96 in group A compared to 6.40 ± 3.39 in group) (p=0.002).
Regarding the serum lipid profile, exercise training significantly reduced LDL and TG in group A patients by 23.48 ± 12.74 and 17.96 ± 8.96 respectively compared to 3.68 ± 6.79 and 9.80 ± 11.08 LDL and TG reduction in group B following medical treatment (p < 0.005). Exercise training increased HDL in group A patients by 4.32 ± 3.38 compared to 1.36 ± 1.44 HDL increase in group B following medical treatment (p-value=0.001).
The reduction in HbA1c by the end of the study showed non-significant difference between both groups (0.25 ± 0.29 in groups A and 0.14 ± 0.24 in group B, p=0.163).
The studied cardiac parameters have been significantly improved in group A following exercise compared to its response to medication in group B. There was an increase in EF (%) of group A patients following exercise by 0.08±1.35 compared to a decrease of 2.12 ± 2.11 in control group B (p-value 0.001). Comparison of the change in METS between the two studied groups was statistically significant (1.64 ± 0.64 and -0.36 ± 0.70 in group A and group B respectively, p-value=0.001).
Discussion
In this study, we found that comprehensive exercise-based cardiac rehabilitation along with drug therapy improved all assessed parameters including systolic and diastolic arterial blood pressure, heart rate, lipid profile (in the form of LDL-C, HDL-C and TG), left ventricular ejection fraction (LVEF), and functional capacity of the patient except glycosylated hemoglobin (HbA1c). The non-significant change in HbA1c levels in this study may due to short term of follow up of patients.
The significant reduction in blood pressure is mostly due to frequent visits in which there is more accurate follow up of blood pressure & tailoring of antihypertensive medications and also due to the combined effect of exercise, healthy diet and patient education.
The effect of exercise on the autonomic nervous system can explain the significant difference in heart rate between the 2 groups. Stimulation of the sympathetic nervous system and suppression of the parasympathetic tone cause the increase in heart rate during exercise, while after the termination of exercise, the autonomic changes that happens during exercise are reversed and this helps decrease the heart rate [11].
The intervention group also showed a significant LDL and TG reduction and a significant HDL rise. On the contrary, the control group showed nonsignificant results regarding LDL, HDL and TG. It is well established that HDL-C levels are `important indicators for the development of atherosclerosis in CHD patients [12]. Therefore, it is considered an important parameter in the evaluation of cardiac rehabilitation impact on the risk factors of coronary artery disease. It is well known that regular exercise is the most practical approach for improving HDL-C levels [13].
The exercise group showed maintenance of left ventricular fraction, which proves the efficacy of exercise-based cardiac rehabilitation in prevention of deterioration of LVEF. Long term prognosis and mortality post myocardial infarction are strongly correlated to LVEF [14-16]. However, little information is available regarding the effect of exercise training on LVEF [16]. It is possible that an 8-week duration exercise program was too short to induce changes in myocardial function and hence the non-significant improvement.
As regards METS, there was a significant increase in the intervention group patients’ functional capacity compared to the control group, which demonstrates the benefits of exercise in maintaining and improving the functional capacity and the quality of life of patients after acute coronary syndromes.
Exercise training can positively affect maximal VO2, central hemodynamic function, autonomic nervous system function, peripheral vascular and muscle function, as well as exercise capacity. These adaptations result in a training effect, allowing an individual to exercise to higher peak workloads at a lower HR with each submaximal level of effort [17]. There are many researches supporting that morbidity and mortality in patients with coronary artery disease are correlated with improved exercise capacity [18,19].
Conclusion
Comprehensive cardiac rehabilitation and secondary prevention programs were able to causes significant improvement of cardiovascular risk factors and functional capacity through optimization of medical treatment, risk factor control, prescribed exercise training and increasing physical activity.
Author Contributions
Noran Ibrahim: Data collection, data analysis, and writing the manuscript.
Ikram Sadek: Study design and reviewing the manuscript.
Hanan Kassem: Study design and reviewing the manuscript.
Timoor Hassan: Study design, data analysis, and reviewing the manuscript.
Declarations
All authors listed meet the authorship criteria according to the latest guidelines of the international committee of medical journal editors. All authors are in agreement with the manuscript.
Ethics Approval and Consent to Participate
An informed written consent was obtained from all participants in the study after explaining the benefits and possible risks of the study as well as the ways to overcome these risks. The patient’s files including their information and investigations were given code numbers in order to guarantee privacy and confidentiality. All the procedures in the study were approved by the institutional board of ethical committee. (Ethical committee of Tanta Faculty of Medicine; Head of Committee Prof. Dr. Enas Arafa, Prof. of Toxicology).
Conflict of Interest
The authors declare that they have no conflict of interest.
Acknowledgement
We like to thank all colleges and nurses in the cardiology department, Tanta university hospital for helping in data collection and completion of the study.
REFERENCES
- Deckers JW. Classification of myocardial infarction and unstable angina: A re-assessment. Int J Cardiol. 2013;167:2387–90.
- Lloyd-Jones D, Adams RJ, Brown TM, et al. Executive summary: heart disease and stroke statistics-2010 update: a report from the American Heart Association. Circulation. 2010;121(7):948.
- Grech ED, Ramsdale DR. Acute coronary syndrome: unstable angina and non-ST segment elevation myocardial infarction. BMJ 2003;326:1259–1261.
- Shaheen S, Magdi A, Esmat I, et al. National Heart Institute Acute Coronary Syndrome Registry. Med. J. Cairo Univ. 2012; 80 (2): 141-149.
- Kushner FG, Hand M, Smith SC, et al. 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (Updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/ SCAI Guidelines on Percutaneous Coronary Intervention (Updating the 2005 Guideline and 2007 Focused Update): A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205–41.
- Watanasawad K, Watanasawad P, Chamsaard P, et al. Effects of a Cardiac Rehabilitation and Secondary Prevention Program on Modifiable Risk Factors in Coronary Heart Disease Patients. Thai Heart J 2010;23: 22-33.
- Grace SL, Abbey SE, Shnek ZM, et al. Cardiac rehabilitation II: Referral and participation. Gen Hosp Psychiatry 2002;24:127-34.
- Frederix I, Van Driessche N, Hansen D, et al. Increasing the medium-term clinical benefits of hospital-based cardiac rehabilitation by physical activity telemonitoring in coronary artery disease patients. Eur J Prev Cardiol 2015;22:150-8.
- American College of Sports Medicine. ACSM Guidelines for Exercise Testing and Prescription. 9th ed. Philadelphia: Lippincott Williams & Wilkins, 2014.
- Josef N. Cardiac rehabilitation manual, 2010
- Mahdavi Anari L, Ghanbari-Firoozabadi M, Ansari Z, et al. Effect of Cardiac Rehabilitation Program on Heart Rate Recovery in Coronary Heart Disease. J Tehran Heart Cent. 2015;10(4):176-81.
- Lavie CJ, Milani RV. Effects of non-pharmacologic therapy with cardiac rehabilitation and exercise training in patients with low levels of HDL-C. Am J Cardiol.1996;78:1286–1289.
- Miller TD, Balady GJ, Fletcher GF. Exercise and its role in the prevention and rehabilitation of cardiovascular disease. Ann Behav Med.1997;19:220–29
- Ratchford AM, Hamman RF, Regensteiner JG, et al. Attendance and graduation patterns in a group model health maintenance organization. Alternative cardiac rehabilitation program. J Cardiopulm Rehabil. 2004;24:150–6.
- Johnson N, Fisher J, Nagle A, et al. Factors associated with referral to outpatient cardiac rehabilitation services. J Cardiopulm Rehabil. 2004;24:165–70.
- Dutcher JR, Kahn J, Grines C, et al. Comparison of left ventricular ejection fraction and exercise capacity as predictors of two and five-year mortality following acute myocardial infarction. Am J Cardiol. 2007;99:436–41.
- Fletcher G, Balady GJ, Amsterdam E, et al. Exercise standards for testing and training. A statement from the American Heart Association. Circulation 2001;104:1694–740.
- Thomas RJ, Denna T. The role of cardiac rehabilitation following acute coronary syndromes. Curr Cardiol Rep. 2014;16(10):534.
- Stephens MB. Cardiac rehabilitation. Am Fam Physician.2009;80(9):955-59.