Exercise-induced lower extremity ischemia
Received: 07-Nov-2017 Accepted Date: Nov 17, 2017; Published: 23-Nov-2017
Citation: Malarkey S, Chess B, Mikkineni K. Exercise-induced lower extremity ischemia. J Vas Dis Treat. 2017;1(1): 07-09.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
This case demonstrates a 59 year old, active Asian male patient, who presented with subacute left lower extremity ischemia in the absence of other findings or associated history. A vigorous exercise session resulted in new-onset, unilateral claudication symptoms. After two weeks, the progression to numbness on the dorsum of his foot raised concern for the patient, thus prompting his decision to receive treatment. The patient was found to have thrombus in his left popliteal artery with minimal evidence of atherosclerosis and the only potential culprit was a right ventricular mass. The treatment was a popliteal embolectomy with near-complete symptom resolution. This case elucidates an otherwise obscure etiology for limb ischemia in that a right ventricular lesion manifested with embolization to the leg related to a possible valsalva-induced reflux across the tricuspid valve.
Keywords
Case report; Embolus; Exercise-induced; Limb ischemia; Right ventricular thrombus; Valsalva
Introduction
The purpose of this case presentation is that it highlights a common pathology that presented itself in an unusual fashion. A variety of different causative reasons exist for limb ischemia and this case does not serve to offer a different etiology for the presentation (i.e. tumor or thrombus) [1]. Rather, it does suggest that certain pathologies may be more indolent in nature and the pathophysiology is not always exact. An examination of published literature did not distinctly identify a case series where patients have a known (or unknown as in this case) right ventricular or pulmonary artery mass that undergoes systemic embolization. The patient’s care is also purposefully demonstrated showing how a conservative surgical approach can lead to not only symptom resolution but improved morbidity, at least in the short term and does not conflict with the standard of care which is removal of the embolus, attempted identification of the source and systemic anticoagulation [2]. This patient was treated at a single academic institution. This work was a retrospective case review and has been reported in line with the SCARE and PROCESS guidelines [3-6].
Case Report
A 59 year old Asian male with a limited past medical history, and no surgical history, presents to the emergency room with reported two week history of left lower extremity discomfort. He states that his symptoms began following a vigorous exercise session. His symptoms mimicked claudication without a prior history of similar symptomatology or antecedent risk factors for atherosclerotic disease (smoking, hypertension, diabetes). His symptoms also appeared to be inconsistent with limb-threatening ischemia; therefore he was not immediately taken to the operating room. The patient consented to the presentation of this case.
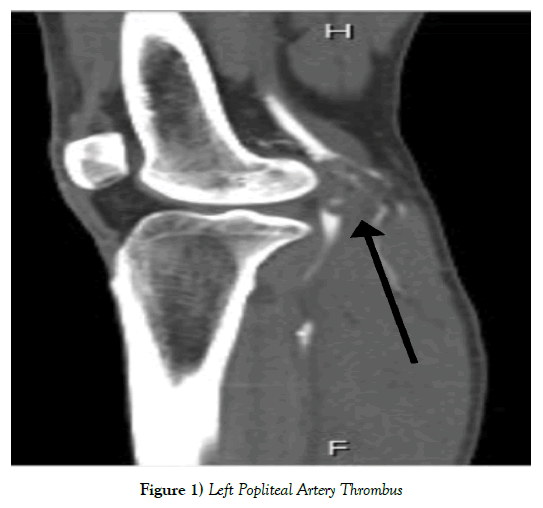
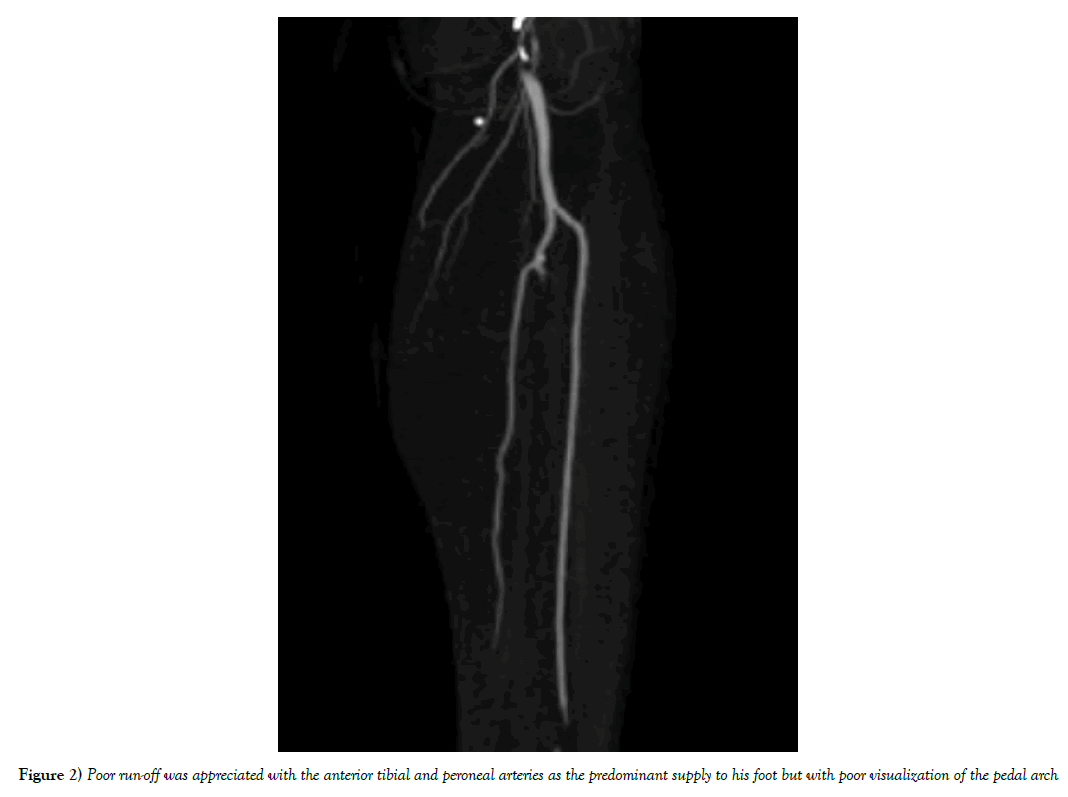
The initial evaluation demonstrated relative leukopenia, no arrhythmia on his electrocardiogram, and no abnormal laboratory markers to suggest ischemia. His pulse examination demonstrated palpable femoral and popliteal pulses bilaterally; the right dorsalis pedis and posterior tibial pulses were palpable but were absent on the left to both palpation and doppler evaluation. He underwent a CT-angiogram of his left lower extremity which demonstrated an occlusive thrombus in the above-knee popliteal artery with associated filling defect (Figure 1). Poor run-off was appreciated with the anterior tibial and peroneal arteries as the predominant supply to his foot but with poor visualization of the pedal arch (Figure 2). The patient underwent systemic heparinization and admission to the hospital.
An extensive evaluation for the etiology of the thrombus began with an echocardiogram which demonstrated an ejection fraction within normal limits. However, a large intra-cavitary mobile mass measuring 2.5 x 3.7 centimeters was present in the right ventricle. The patient subsequently underwent a cardiac MRI which demonstrated new and enlightening information about the character of the cardiac mass. The right ventricular mass measured at 3.4 centimeters in greatest diameter. There was also a left pulmonary artery mass, measuring 4.1 centimeters in length. These masses were isotense on T1 imaging with an increased signal intensity on T2 imaging which aided in the suggestion of a possible tumor; although thrombus could not be excluded as the time interval of thrombus formation varies the degree of MR signal [7-10]. No masses were identified in the left atrium, right atrium or left ventricle. A repeat echocardiogram with a bubble study did demonstrate a patent foramen ovale and no evidence of right ventricular strain despite the large pulmonary artery lesion. The patient also underwent a lower extremity venous duplex which was negative for deep venous thrombosis or sequelae to suggest chronic clot.
Given the radiographic findings, in association with the absence of a hypercoagulable state, underlying arrhythmia, trauma or other direct source of arterial embolization, the cardiac and pulmonary lesions were suggestive of possible tumor. The inability to rule in or out tumor prompted a multidisciplinary evaluation and discussion about obtaining tissue for diagnosis. It was eventually determined that the most efficacious way to obtain tissue was to remove the popliteal thrombus with the presumption that it embolized from the right ventricle. At this point, the patient had subjectively improved with heparin, with reduced dorsal foot numbness, but still had residual claudication symptoms. His subjective improvement allowed for delayed operative intervention especially when there was concern about worsening his overall clinical condition with surgical manipulation.
One week following his initial presentation, the patient was taken to the operating room. The operation consisted of an incision below the knee with identification of the below knee popliteal artery. There was no pulse in the vessel. The anterior tibial artery and tibio-peroneal trunk were also appropriately identified. A transverse arteriotomy was created in the below knee popliteal artery. Using a number three Fogarty catheter in a retrograde fashion, a thrombectomy was performed with resolution of vessel thrombosis and the presence of brisk pulsatile flow was appreciated. A number two Fogarty catheter was then able to be passed into the anterior tibial artery with extraction of a small amount of thrombus. The extracted thrombus was sent to pathology.
The patient did well following the operation. The pathology report suggested “organizing blood clot, consistent with thrombus.” He was discharged on post-operative day three with a therapeutic INR with plans to continue with Coumadin therapy. The Cardiac Surgery service in conjunction with Cardiology and Hematology agreed that the patient would be best served with anticoagulation and interval follow-up with repeat imaging. Follow-up out to six months, with repeat Cardiac MRI, demonstrated reduction in size of the right ventricular and pulmonary artery lesions (from 3.4 to 2.9 centimeters and 4.1 to 1.9 centimeters respectively) in addition to progressive improvement in left lower extremity symptoms. This substantiated the supposition that the patient’s right ventricular mass is consistent with thrombus given the ambiguity based on imaging, and the interval resolution in size on imaging, ultimately avoiding the need for intra-myocardial biopsy that would otherwise add further morbidity.
Discussion
When determining thrombosis versus embolism as possible etiologies for arterial occlusion, there are subcategories for each. The sources for arterial obstruction are classically determined to be cardiac, paradoxical emboli, thrombosis, prothrombogenic states, or any precipitant of endothelial injury [1]. Based on our literature review, there do not appear to be evidence of case reports where the presumed nidus for arterial embolization is a right ventricular mass. However, sources of paradoxical emboli causing acute limb ischemia and other embolic phenomenon have been described [7,8]. Cardiac sources would expect to be atrial thrombus from atrial fibrillation, left ventricular thrombus from previous myocardial infarction, debris from infected prosthetic or cardiac valves1, or a migratory thrombus from the right atrium to left atrium via a patent foramen ovale [11,12]. However, the ability of a right ventricular thrombus to reflux across the tricuspid valve and traverse a patent foramen ovale is a pathophysiologic phenomenon that has seemingly not been described. The physiologic effect of valsava-induced increase in right atrial pressure with its associated increased propensity for right-to-left shunt via a patent foramen ovale does allow for this possibility [13].
We present this patient as an interesting case because it highlights the obscure nature by which acute arterial ischemia may occur. The patient here presents with obvious radiographic signs of an arterial occlusion with a potential source being a cardiac lesion. However, the pathophysiology does not lend itself to a particularly common presentation. It is still the prevailing theory that the physical activity of the patient, with potential valsava maneuvers, caused a reflux of the intra-ventricular material across the tricuspid valve and distributed it via the patent foramen ovale into the systemic circulation. The absence of any previous venous thrombotic disease or concomitant deep vein thrombosis on presentation suggests that the patient does not appear to have a hypercoagulable state that could possibly exclude the right ventricular thrombus as the source. The obvious limitation is the absence of obtaining a direct myocardial biopsy of the suspected lesion. However, the findings of a thrombus as the pathological presentation of the clot coincides with the resolving nature of the intra-cardiac mass on follow cardiac MRI, as well as the interval improvement in patient symptoms after being systemically anticoagulated. There was strong consideration given to intra-myocardial biopsy but given the follow up improvement in size of the intra-cardiac mass with anticoagulation, it was presumed to be thrombus. However, we have not completely ruled out a structural lesion. The working plan is to manage the patient with indefinite anticoagulation and interval follow-up, the results of which have been satisfactory to date.
Conclusion
This case report demonstrates the presumed capability of a right ventricular mass to undergo intra-arterial embolization via a valsalva-induced reflux. It also demonstrates that a conservative surgical approach can lead to satisfactory results. This appears to be an isolated case but further study could be directed towards the physiologic assessment of intra-cardiac reflux, particularly as it pertains to right heart lesions.
REFERENCES
- Mitchell ME, Carpenter JP. Overview of Acute Arterial Occlusion of the Extremities. 2016.
- Norgren L, Hiatt WR, Dormandy JA, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007;45(1):S5-67.
- Agha RA, Fowler AJ, Saetta A, et al. The SCARE Statement: Consensus-based surgical case report guidelines. Int J Surg. 2016;34:180-6.
- Agha RA, Fowler AJ, Rajmohan S, et al. Preferred reporting of case series in surgery; the PROCESS guidelines. Int J Surg. 2016;36:319-23.
- Baguet JP, B Faurie, C Saunier. Bulky thrombus associated with patent foramen ovale. Heart. 2005;91.
- Gunduz Y, Ucar A, Vatan MB, et al. Tricuspid valve thrombus causing acute pulmonary embolism. BMJ Case Rep. 2013;2013.
- Kouskov OS, Nichols DJ, O'Hearn DJ. Paradoxical arterial embolism involving both upper extremities in a patient with pulmonary embolism and a patent foramen ovale. Clin Appl Thromb Hemost. 2011;17(6): e98-101.
- Liu M, Menzoian JO. A Patient with Multiple Paradoxical Emboli. J Vasc Surg. 2016:63(4):1085-7.
- Varun M, Awan MU, Faraj K, et al. Traversing Boundaries: Thrombus in Transit with Paradoxical Embolism. J Community Hosp Intern Med Perspect. 2016; 6(4):31438.
- Motwani M, Kidambi A, Herzog BA, et al. MR Imaging of Cardiac Tumors and Masses: A Review of Methods and Clinical Applications. Radiology. 2013;268(1):26-43.
- Ozdogru I, Kaya MG, Dogan A, et al. Thrombus Crossing through a Patent Foramen Ovale. Int J Cardiol. 2009;133(2):e55-6.
- Robert BR, Cronenwett JL, Johnston KW. Rutherford's Vascular Surgery. Elsevier Saunders. 2014.
- Zhao E, Zhang Y, Kang C, et al. Influence of the Valsalva maneuver on the cardiac hemodynamics and right to left shunt in patients with patent foramen ovale. Sci Rep. 2017;7:442-80.