Foam sclerotherapy and eccentric compression
2 Department of Vascular Surgery, 19 rue St Pierre 43100 Brioude, France
Received: 18-Dec-2020 Accepted Date: Jan 01, 2021; Published: 08-Jan-2021, DOI: 10.37532/1983-8905.2021.14(1).6-9
Citation: Crebassa V, Mollard G. Foam sclerotherapy and eccentric compression. J Phlebol Lymphol.14(1):6-9.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Digressive compression of 20 mm Hg does not modify the diameter of saphenous varicose veins in a standing position. This explains the results of Dr Hamel-Desnos’ study, which demonstrated that there was no significant benefit to the use of this compression after treatment with foam sclerotherapy of the Great Saphenous Vein. Dr. Zarca will confirm, few years later, these same results with a compression of 30 mm Hg.
So how can we explain the recommendations of many authors who suggest that we must use an eccentric compression?
This can be explained by the Laplace’s Law which explains that the more the surface is plane, the lower the transmitted pressure is. This is also explained by the physical law of pressure transmission according to the density of the compressed tissues: the suppler the surface is, the lower the transmitted pressure is.
This is obviously the case for the medial part of the thigh where we would like to compress the GSV and for the posterior part of the calf for the SSV compression. These surfaces are flat and the tissue is supple and depressible. Digressive compression loses in these cases all its efficiency. On the other hand, eccentric compression allows us to concentrate the pressure, with denser material, on a specific area, to promote healing, fibrosis and control inflammation. Under no circumstances, it plays a role in venous return. It favours varicose vein treatments during the short healing period, possibly in addition to digressive compression.
Eccentric compression is often put in place by the doctor and cannot be replaced by the patient. Moreover, this compression is artisanal and the applied pressure is not measurable.
We have thus studied a new device that corresponds to a standardisation of the eccentric compression that the patient can put over his clothes and reposition whenever he wants, according to his sensations. Our study shows that this eccentric compression allows the reduction of varicose vein diameter and therefore the volume of the saphenous veins and superficial varicose veins decrease up to 70%. Blood is the public enemy of all our treatments, thus, as the volume of blood is reduced in the treated varicose veins we reduce haematomas after surgery, we limit blood carbonisation around the thermal probe and we decrease the volume of foam injected.
Maintaining this compression 48 hours after these treatments would enable us to have a more harmonious fibrosis, in addition to reduced side effects related to excessive inflammation (redness, intravenous blood traps, hematomas, localized pain, pigmentation). We could also consider treating larger varicose veins with this eccentric compression, without increasing the volume of foam injected.
Keywords
Varicose vein; Diameter; Volume; Eccentric compression; Foam sclerotherapy; Compression and foam sclerotherapy
Introduction
The first public ennemi of endovenous treatment is the blood. The major risk of inefficiency and complications during sclerotherapy is the presence of blood in the treated varicose vein. If it be during thermic endovenous treatment [1-3] reducing the diameter of the varicose vein during and after the treatment is a major therapeutic objective, or more specifically, reducing the volume of blood in the varicose vein during but also after the treatment is a major therapeutic objective. The reduction of the varicose vein will not only improve results by obtaining uniform fibrosis but also reduce possible side effects and potential complications [4].
Why are we divided on the Utility of Compression after Endo Venous Treatments?
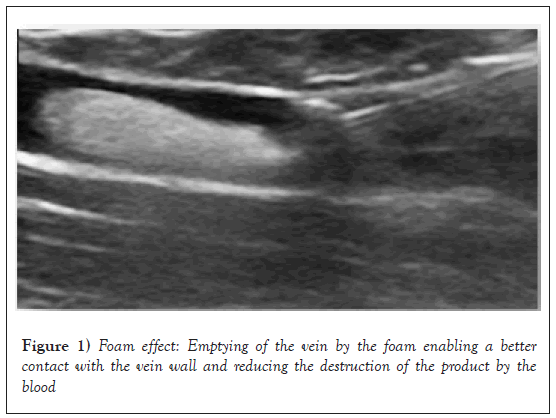
Chemical endo venous techniques are also limited by the presence of blood. The sclerosing product is destroyed by the blood not only in vivo [5] but also in vitro [6]. The “foam” effect allows us to delay the destruction of the product by the blood by totally emptying the varicose vein. The contact time between the product and the vein wall is therefore increased (Figure 1).
The volume effect of the foam explains these results. However, this technique reaches its limits when treating voluminous varicose veins. Only a limited quantity of foam can be injected into the vein [7].
Therefore, it is highly useful to reduce the diameter of the varicose vein in order to reduce the quantity of foam to be injected. This also increases the contact time between the product and the vein wall and allows us to treat bigger varicose veins.
Whatever the treatment, the reduction of the diameter of the treated varicose vein after treatment and “antalgic compression“, preventing movement, is a therapeutic objective. This favors uniform fibrosis and limits side effects and possible complications such as: pigmentation, swelling, venous traps requiring thrombectomy, localized pain, regularity defects in the fibrosis but also hematoma, bleeding and cicatrization, complications for surgery.
Which Compression, Digressive or Eccentric Compression?
Certain experts defend the idea that standardized graduated compression is not useful. C. Hamel-Desnos demonstrated this for the treatment of the GVS. She demonstrated that the use of compression stockings of less than 20 mm Hg after sclerosis was not an real advantage [8]. The use of higher pressure does not provide significant better results [9].
Three reasons can explain these results
This can be explained by the imposed and obligatory graduation causing low pressure on the thigh [10,11] questioning the real utility of this graduated compression to obtain an efficient compression and that especially to the thigh. French class II Compression stockings (15 to 20 mm Hg) will only deliver a pressure of around 8 mm Hg on the thigh [12].
On the other hand, the Laplace law explains that the pressure transmitted decreases on flat surfaces such as the back side of the calf muscle where the SSV is located or on the medial side of the thigh where the GSV is situated.
Finally, the transmission of pressure decreases on a “soft” cutaneous muscular surfaces (thigh and back side of the calf muscle) in comparison to “hard” surfaces (tendon and bone) [13].
P=nT/r
P: the delivered pressure is depending of the curvature (r). A flat surface is not compressed (posterior face of the calf), an angular surface is too compressed (Tibia ridge); nT is a constant for a same device).
Some authors have demonstrated that French class II graduated compression (15 to 20 mm Hg) did not modify the diameter of saphenous veins raising the question that compression, in fact, did not reduce the diameters of saphenous and superficial veins [14,15]. In the same way, material delivering a pressure of 20 to 30 mm Hg at the ankle does not compress the superficial veins in a standing position.
This explains that many experts recommend using eccentric compression.
Luggli uses eccentric compression on the thigh. This use significantly reduced postoperative pain in comparison to the non-use of eccentric compression [16].
Mosti demonstrated the more efficient and better results of the use of eccentric compression on the thigh after surgery than the use of class III graduated compression stockings [17,18].
Graduated compression is used to facilitate the venous return. This is done by the rebalancing of hydrostatic and oncotic pressure of the Starling law [19].
Eccentric compression is used during treatment to reduce the diameter of the varicose vein and to reduce the blood volume of the varicose vein. It is used after treatment to control the inflammatory reaction, immobilize the treated zone and to bring a local antalgic effect, to favor uniform fibrosis, reduce bruising and facilitate proper cicatrization.
Graduated and eccentric compression should not be opposed but should be considered complimentary and synergic. One facilitates the venous return and the other facilitates cicatrization by immobilizing the treated zone.
Standardised eccentric compression applies a localized, external compression, reducing the diameter like a tumescence but without any injection, without pain, without needles and consecutives risks. In addition, the diameter reduction and immobilization effect continues as long as the patient carries this compression where a tumescence whose effects disappear in a few minutes or even hours.
What is the Ideal Eccentric Compression System?
The limits of existing eccentric compression
Some authors, such as M. Schadek, recommend compressing the varicose vein during injection with the probe, others with a weight (sandbag) but even if this technique allows the diameter of the varicose vein to be reduced, it does not maintain analgesic, anti-inflammatory and immobilizing pressure after sclerosis. Its action is ephemeral and don’t limit the secondary effects [20].
The problems that we encounter today with eccentric compression are associated with the “awkward” application after sclerosis and due to the fact, that after the treatment, this compression must be maintained in place several days [21]. This compression is either difficult to remove or not removable at all (bandages, adhesive strips). Moreover, these compression systems are not standardized, the reproducibility is poor; the reliability of the application by the patient is practically impossible (Figure 2).
To improve reproducibility we therefore try to use a standardised compression stocking or under an overlap of two compression stocking by interposing a localized overpressure system (silicone foam compress). The use of standardised compression stockings allows for possible self-installation by the patient [22].
However they are difficult to put into place by the patient because the patient must also pull on the two compression stockings to position the large foam around the painful and that after the treatment potentially painful.
It is the same for other techniques that have proved their efficiency [23]. The patient cannot install it alone for most systems.
The new device: Thanks to the experience and knowledge of our Masters we have studied a standardized eccentric compression device reserved for compression during and after varicose vein treatment in order to reduce the volume of blood in the varicose vein during treatment but also after treatment to improve fibrosis and to limit the adverse or exacerbated effects of sclerotherapy [24].
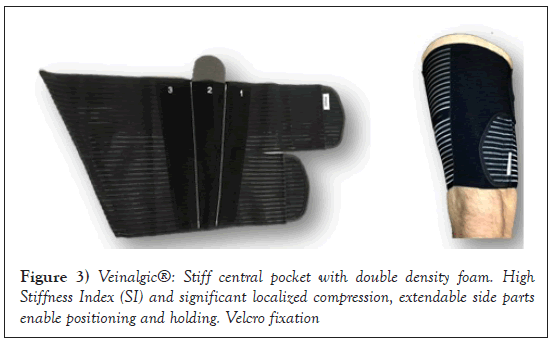
The standardized eccentric contention-compression orthosis (Veinalgic®) is a device which is easy to use and fit alone if the patients can reach their thigh or calf muscle themselves (Figure 3).
It is composed of an inextensible tissue pocket containing a dense foam to be applied on the treated varicose vein. Thanks to the reduction of the curvature by the dense foam, the inter face pressure obtained, when the device is placed by patients, is high (40 to 70 mm Hg) and the Stiffness Index (SI) is significant and there is no tourniquet effect. The device is maintained on the skin or on the compression stocking by a vertical silicon strap. The pressure is adjusted by the patient using the numerical markers. This rigid part is maintained by two long-stretch elastic straps. This contention-compression device is neither tubular nor knitted, it is adjustable, washable, sterilizable and reusable. It is composed of a contention part which is inextensible and a maintaining compressive part which is extensible. Patients reported no inconvenience related to pain or specific discomfort using the compression system. No patient reported difficulties positioning the system.
The cost is low, it is washable, sterilizable and reusable. It can be used and conserved by the patient all along the evolution of the chronic venous disease.
The reduction of the diameter is significant with this standardized eccentric compression with a relatively moderate pressure because the system is evaluated at 50% extension (marker 2 for an interface pressure of 50 mm Hg). This pressure can be increased (marker 3) giving us hope that the diameter can be further reduced (Table 1).
| Stretching | Elastic part | Stiff part | ||||
|---|---|---|---|---|---|---|
| P | P-standing | SI | P | P-standing | SI | |
| lying | lying | |||||
| 30% marker 1 | 24.6 | 24.6 | 0 | 33 | 63.4 | 30.4 |
| 50% marker 2 | 32 | 36.2 | 4.2 | 40.6 | 73.4 | 32.8 |
| 100% marker 3 | 46.4 | 54 | 7.6 | 50.8 | 87.6 | 36.8 |
Table 1: Pressure and stiffness index delivered by Veinalgic®, on the thigh, according to the stretching under the elastic part and under the stiff part.
Some effects of this device in a recent study: 76.9% of the varicose veins concerned the Greater Saphenous Vein (GSV) and 23.1% concerned the Small Saphenous Vein (SSV). The varicose veins were located in the saphenous compartment in 76.6% of the cases; they were superficial therefore above the superficial fascia in 24.4% of the cases. 95.4% of the varicose veins were primary and 4.6% were recurrences [25].
The reduction of the diameter is more than one third (36%) on incontinent saphenous veins and is reduced even more on superficial varicose veins (43% reduction) (Table 2).
| Group | Without veinalgic | With veinalgic | Delta | Student-test (paired) |
|---|---|---|---|---|
| Below fascia (n=97) |
4.4 ± 1.3 IC95%:[4.1; 4.6] |
2.8 ± 0.9 IC95% [2.6; 2.9] |
1.6 ± 1 IC95%:[1.4; 1.9] |
Value T:15.4199 p-value:<0.0001 |
| Above fascia (n=33) |
5.1 ± 1.9 IC95%[4.4; 5.8] |
2.9 ± 1 IC95%:[2.5; 3.2] |
2.2 ± 1.6 IC95%:[1.6; 2.8] |
Value T: 7.8793 p-value:<0.0001 |
| Global (n=130) |
4.6 ± 1.5 IC95%:[4.3; 4.8] |
2.8 ± 0.9 IC95%:[2.6; 2.9] |
1.8 ± 1.2 IC95%:[1.6; 2] |
Value T: 16.5077 p-value:<0.0001 |
| ANOVA | Value F:5.6706 p-value:0.0187 |
Value F:0.5197 p-value:0.4723 |
Value F:5.2943 p-value:0.023 |
Table 2: Evolution of the diameter of varicose veins in a lying position with and without eccentric compression.
A reduction of 43% of the diameter of a superficial varicose vein will reduce the volume of this varicose vein by 68% for a 50% extension of the device (demonstration 1). In the same manner, a reduction of 36% of the diameter of a saphenous vein will reduce the volume of this saphenous vein by 59%. We therefore immediately see the implications of this external eccentric compression before and after therapy. This goes for both thermic and chemical endo-venous treatments and after surgery by the exerted hemostatic pressure. This device allows us to apply high localized pressure exactly where we want. It allows us to reduce the diameter of the varicose vein by nearly 40%, to reduce the volume of the varicose vein by at least 59% and finally to obtain a localized stiffness and Stiffness Index which is very significant. This study have proved that the effect on the diameter is the same in standing and lying position whatever is the diameter and the superficial or sub facial position of the varicose vein.
Thanks to the immobilization of the treated zone, which is therapeutically traumatized, and thanks to the reduction of the volume of blood in the varicose vein, we can realistically hope to reduce the strength of our treatments (especially during a sclerosis with foam) and therefore reduce the harmful side effects of our treatments.
This external eccentric compression can also allow us to imagine an extension of the indications of each technique. As the diameter of the varicose vein to be treated changes, so does the prolongation of the “tumescence effect” especially after an ephemeral tumescence anesthesia.
Our patients can easily adjust this compression without the inconveniences of having to pull on and off the familiar stocking with graduated compression systems. Patients can easily take it off, even temporarily, to take a shower for example. It is possible to adjust the system over stockings or socks. Patients have not expressed either irritation or slipping of the system in daily use.
Conclusion
The graduated compression is inoperative to reduce the size of the varicose vein. Any eccentric compression is useful for reducing the diameter of superficial varicose veins and saphenous veins. Some are efficient during the treatment, others during the treatment and during the days following the treatment reducing local pain and stimulate parietal fibrosis [26].
The evolution of the eccentric compression is its standardization. It permits an easier using by the patient themselves, every day, with efficiency and can be easily readjusted identically to the initial setting. The standardization promotes the compliance and certify the delivered pressure.
The walk decreases the risk of thrombosis. The walk increases the delivered pressure by an rigid part in front of the varicose vein and increase the effect of the compression because of its stiffness index. The eccentric compression will allow us to reduce the volumes of concentrations injected in case of foam sclerosis.
Eccentric compression allows us to imagine changes our sclerotherapy indications, changes in injection volumes and an increase in contact time allowing a reduction in the concentrations used. It makes it possible to limit the harmful effects even if they are not serious in sclerotherapy.
After more than 1700 Patients treated with this eccentric compression I advise to conserve the compression 3 days and more according to the inflammatory or the sensations. The eccentric compression is indicated specially for larger saphenous veins or for superficial varicose vein but further studies are however required to evaluate the consequences of eccentric compression on our therapeutic attitudes and their results.
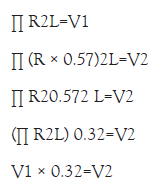
Demostration 1: Initial varicose volume × 0.32=Volume using Veinalgic®
R=radius of the varicose vein, R × 0.57=43% reduction=new radius, L=length of the varicose vein V1=volume of the varicose vein, V2=volume after compression.
REFERENCES
- Desnos P. Mode d’action des différents Lasers endo-veineux et impact des differentes longueurs d’onde. Phlebologie. 2013; 66(2):28-33.
- Anastasie B, Mordon S, Cazaubon M, et al. Lasers endo-veineux. Angiologie. 2012; 64(2):50-62.
- Luggli M, Logo A, Guerzoni S, et al. Effects of eccentric compression by a crossed-tape technique after endovenous laser ablation of the great saphenous vein: a randomized study. Phlebology. 2009; 24(4):151-6.
- Mosti G. Post-treatment compression: Duration and techniques. Phlebology. 2013; 28(1):21-4.
- Lurie F, Lal BK, Antignani PL, et al. Compression therapy after invasive treatment of superficial veins of the lower extremities: Clinical practice guidelines of the American Venous Forum, Society for Vascular Surgery, American College of Phlebology, Society for Vascular Medicine, and International Union of Phlebology. J Vasc Surg Venous Lymphat Disord. 2019; 7(1):17-28.
- Parsi K, Exner T, Low J, et al. In vitro Effects of Detergent Sclerosants on Clot Formation and Fibrinolysis. Eur J Vasc Endovasc Surg. 2011; 41(2):266-77.
- Watkins MR. Deactivation of Sodium Tetradecyl Sulphate Injection by Blood Proteins. Eur J Vasc Endovasc Surg. 2011; 41(4):521-5.
- Rabe E, Breu FX, Cavezzi A, et al. European guidelines for sclerotherapy in chronic venous disorders. Phlebology. 2014; 29(6):338-54.
- Hamel-Desnos CM, Guias BJ, Desnos PR, et al. Foam sclerotherapy of the saphenous veins: randomised controlled trial with or without compression. Eur J Vasc Endovasc Surg. 2010; 39(4):500-7.
- Zarca Ch, Bailly C, Gachet G, et al. classMousse 1: bas medicaux et injection de mousse. Phlebologie. 2012; 65(1):11-20.
- Benigni JP, Cornu Thénard A, Uhl JF. la sclérothérapie. Editions ESKA. 2007; 205-7.
- Benigni JP, Uhl JF, Cornu Thenard A. La thérapeutique compressive a la cuisse. Phlebologie. 2009; 62(1):77-80.
- Ricci S. La sclerotherapie. Editions ESKA. 2007:235-8.
- Gardon-Mollard C. Compression médicale. Edition Masson. 219.
- Partsch H, Menzinger G, Borst-Krafek B, et al. Does thigh compression improve venous hemodynamics in chronic venous insufficiency? J Vasc Surg. 2002; 36(5):948-52.
- Rastel D. No reduction of diameter under the fascia with 20 mm Hg. Phlebologie. 2014; 67(1):40-5.
- Lord RSA, Hamilton D. Graduated compression stockings (20-30 mmHg) do not compress leg veins in the standing position. ANZ J Surg. 2004; 74(7):581-5.
- G Mosti. Post-treatment compression: Duration and techniques. Phlebology. 2013;28 Suppl 1:21-4.
- Mosti G, Mattaliano V, Arleo S, et al. Thigh compression after great saphenous surgery is more effective with high pressure. Int Angiol. 2009; 28(4):274-80.
- Crebassa V. Oedème veineux chronique et compression médicale. Phlebologie. 2014; 67(3):34-42.
- Gachet G, Galem K. L'écho-sclérose mousse des varices sous compression ou tumescence externe : L'étude MOUSSECOMP. Phlebologie. 2014; 67(3):23-28.
- Benigni JP, Allaert FA, Desoutter P, et al. The efficiency of pain control using a thigh pad under the elastic stocking in patients following venous stripping: Results of a case-control study. Perspect Vasc Surg Endovasc Ther. 2011; 23(4):238-43.
- Milleret R. The sclerosis of the large saphenous veins by means of foam emitted through an ultrasound-guided catheter: Alpha Technique. The conclusions of the first 1000 treatments. Phlebology. 2006;59:53-8.
- Gardon-Mollard C, Crebassa V. Évaluation de la pression interface délivrée et de l'Indice deRigidité (IR) d'un nouveau dispositif combine de contention-compression excentrée pour les suites des traitements de volumineuses varices saphènes ou superficielles. Phlebologie. 2014; 67(4):32-64.
- Crébassa V, Galleze B, Gardon-Mollard C, et al. Réduire de 70% le volume des varices pendant et après traitements. Tumescence externe par compression excentrée standardisée. Phlebologie. 2017; 70(3):20-8.
- Fegan WG, Fitzgerald DE. A histologic assessment of continuous compression sclerotherapy. Angiology. 1965:433-42.