Gastric pulmonary resection cancer
Received: 03-Jun-2022, Manuscript No. PULCMR-22-4352; Editor assigned: 06-Jun-2022, Pre QC No. PULCMR-22-4352(PQ); Accepted Date: Jun 29, 2022; Reviewed: 18-Jun-2022 QC No. PULCMR-22-4352(Q); Revised: 24-Jun-2022, Manuscript No. PULCMR-22-4352(R); Published: 30-Jun-2022, DOI: 10.37532/pulcmr-.2022.4(3).59-60
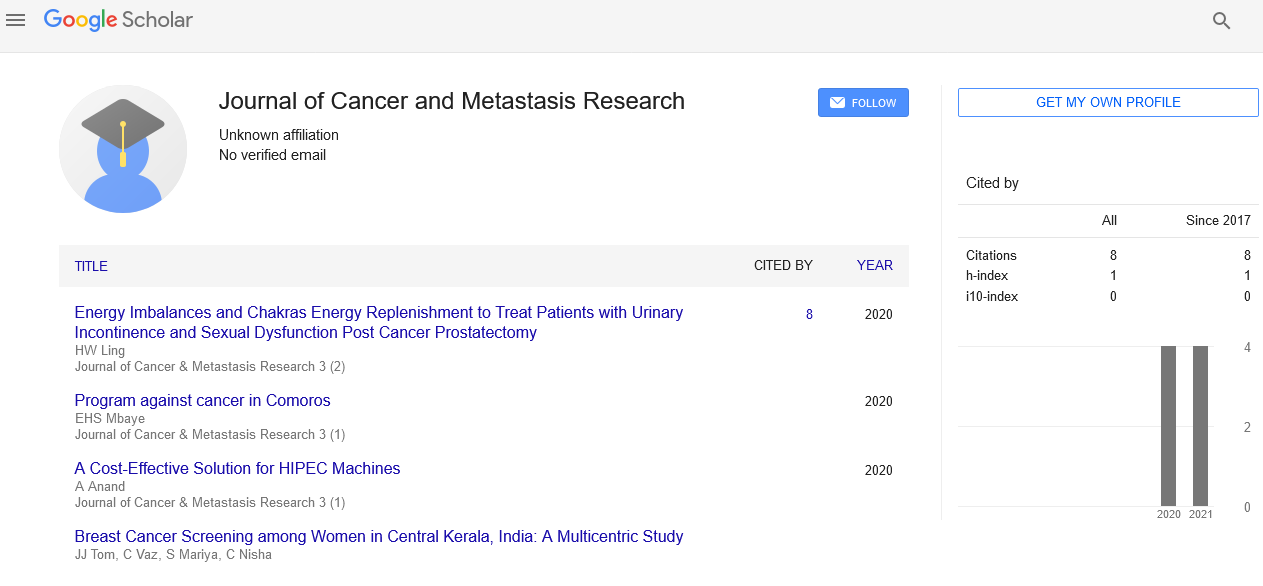
Citation: Sophia. Gastric pulmonary resection cancer. J Cancer metastasis res. 2022; 4(3):59-60.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Cancer is the subsequent driving reason for death in the United States. Although the frequency and mortality of gastric disease has diminished essentially since the 1930s, this harm is as yet the fourth most normal malignant growth around the world also the fourteenth most normal in the United States. The lifetime hazard for development of gastric disease is around 1 of every 113 with an age-changed rate of 8 in 100,000 and yearly passing pace of 4.1 per 100,000.3 and large 5-year endurance is 24.7%, going from 78% for restricted infection to 2% for far off disease. Unfortunately, at determination, just 25% of patients present with limited sickness bound to the actual stomach; 30% present with local nodal illness, and another 35% have far off metastases.
Keywords
Gastric; Pulmonary; Metastasectomy; Chemotherapy
Introduction
Future from the hour of pneumonic repeat is poor with a middle endurance of a half year, which isn't essentially impacted by fundamental chemotherapy. 70% of patients are dead inside 1 year, and 89% are dead inside 2 years of recurrence. A meta-examination of patients with Metastatic Gastric Disease (MGD) showed a 5 year endurance of 0% to 7% with a general 5 year endurance of 2% with chemotherapy alone. 11 no of patients with pneumonic metastases treated with chemotherapy alone made due to the 5 year follow-up in any of these preliminaries. An audit of in excess of 5000 patients who went through aspiratory resections for malignancies of different histologies showed that after complete metastasectomy, a middle endurance of 35 months with long haul endurance of 36% at 5 years, 26% at 10 years, and 22% at 15 years is conceivable in chosen patients and histologies. Pulmonary Metastasectomy for metastatic colorectal malignant growth has become norm of care in view of review information alone and has never been exposed to a randomized controlled preliminary. Up to this point, there have been no far reaching investigations of the distributed information depicting pneumonic metastasectomies for MGC. Besides, no examinations looking at careful resection to best elective consideration of foundational chemotherapy have tended to this theme in a forthcoming randomized design. It was our objective to audit all distributed information for aspiratory resection of MGC and to endeavor to recognize potential patients who may profit from this treatment methodology. A far reaching search of the midline and scopes data sets was performed to recognize all distributed reports of pulmonary resections for gastric malignant growth in three dialects (English, German, and Japanese) utilizing the accompanying watchwords: lung, pneumonic, metastasis, gastric, stomach, malignant growth, resection and metastasectomy. All non-english distributions were interpreted by a creator familiar with the essential language of the distribution. Information gathered incorporated the extended period of distribution, name and nation of foundation, size of the series, patient socioeconomics, pathologic subtleties of essential gastric growths remembering American joint committee for cancer growth, hub, metastasis arranging, site of first repeat, timing of aspiratory metastasis and resection, sort of activity, pathologic subtleties of metastatic growth, time to repeat from metastasectomy, adjuvant and neo adjuvant chemotherapy and radiation treatment, follow-up and in general endurance (operating system). 15% (5/34) of patients had T1 growths, 47% (16/34) had T2 growths, 23% (8/34) had T3 cancers and 15% (5/34) had T4 growths. 35% (12/34) of the patients had No illness, 38% (13/34) had N1 infection, 15% (5/34) had N2 illness, and 12% (4/34) had N3 infection. 6 growths had proof of lymphatic or potentially vascular intrusion on definite pathology. For those with histologic portrayals, 53% (8/15) of cancers were all around separated, 33% (5/15) were tolerably separated, and 13% (2/15) were accounted for as ineffectively separated. Degree of lymph hub analyzation was not announced in any review. All patients were resected to no proof of sickness after gastrectomy. Information on neo adjuvant treatment before gastrectomy were accessible for half (22/44) of patients, none of whom got neo adjuvant chemotherapy or radiation before essential gastrectomy. Information on adjuvant treatment after gastrectomy were accessible for 65% (28/43) of the patients, 36% (10/28) of whom got adjuvant chemotherapy and one of whom moreover gotten adjuvant radiation treatment. Segment and clinic pathologic factors were analyzed to decide any prognostic elements related with DFS after gastrectomy. On additional examination, those patients who went through all out gastrectomy were found to have higher generally speaking stage cancers than the individuals who went through distal gastrectomy [6]. Patients in the complete gastrectomy bunch had 24% and 76% stage I and stages IIIV growths, separately, contrasted and 62% and 38% among those going through distal gastrectomy. The relationship of adjuvant chemotherapy after gastrectomy on DFS was too inspected, and there was no measurably critical contrast in DFS between the individuals who got adjuvant chemotherapy and the people who didn't (22 months versus 39 months (p 0.139).
Resected Pulmonary Metastases
Pulmonary resections were performed at a middle of 35 months (range: 0 months to 120 months) after essential gastrectomy in the 19 examinations for which data was accessible. Of the 88% (42/48) of the pneumonic resections for which definite information were accessible, most of patients 81% (34/42) had one sore, 17% (7/42) had two sores, and 2% (1/42) had three injuries resected in a similar activity. Sore size was accounted for in 44% (22/48) of resections. All the patients who had more than one sore resected had sickness that was restricted to one hemi thorax. For the seven patients with two sores resected, five patients had unilobar ipsilateral sickness, and two patients had illness in two projections. The one patient with three injuries had illness in two projections lobectomies, segmentectomies, wedge resections, consolidated lobectomy and wedge resection, and sternal resection with coalition wedge resection, individually. 10% (5/48) were pneumonic resections that were not in any case determined. The degree of thoracic lymphadenectomy was not detailed in any study; be that as it may, 10 investigations detailed lymph hub status on last pathology, and two of these patients had proof of lymphatic association. Employable intricacies were accounted for in 10 investigations; in nine, there were no morbidities revealed, and in one there was a chylothorax. There were no perioperative mortalities. There was no measurably critical prognostic element for DFS after aspiratory metastasectomy. There were no genuinely huge prognostic elements for OS; be that as it may, there was a pattern toward expanded OS among patients who had longer than the authentic DFI of two years (middle OS: 65 months versus 19 months (p 0.119) and who had less broad resections contrasted and lobectomy (middle OS: not came to versus 45 Months (p 0.081). The patient was alive without proof of sickness and 67 Months after his first pneumonic metastasectomy at 79 month post gastrectomy. The second patient in this series was a 58 year elderly person who went through a distal gastrectomy for stage IV (T4N3M0) adenocarcinoma. She had an underlying repeat in the liver 14 months. After gastrectomy and went through liver resection, trailed by right upper and lower lung segmentectomies 3 years later gastrectomy and afterward a recurrent right lower segmentectomy 44 Months after gastrectomy for aspiratory metastases. This patient was alive without proof of infection 180 Months after gastrectomy and 84 months after starting aspiratory metastasectomy. For patients with pneumonic repeats after beginning resection, rehash metastasectomy was related with huge expansion in OS contrasted and the individuals who didn't go through recurrent resection of their pneumonic repeat (middle OS: not yet reached versus year and a half, (p 0.008).
While looking at these five patients who went through rehashes. Resection with the other patients who just went through a Single resection, there was a pattern toward expanded OS. Among the individuals who went through recurrent resection, however this was not genuinely critical middle OS not yet reached versus 22 months, (p 0.053). 9% (4/43) of the patients had disengaged. Extra pulmonary metastases that were resected furthermore. To aspiratory metastasectomy. 3 patients had hepatic Metastases that were resected at 14 months, 38 months. An undefined time after gastrectomy and in this way went through aspiratory resections at 3 years, 71 months, What's more 16 months after gastrectomy, individually. One patient had an aspiratory metastasectomy at two years after gastrectomy, trailed by resection of a right adrenal metastasis at 30 months, resection of a retroperitoneal repeat at 42 months, and a second aspiratory metastasectomy at 50. Months after gastrostomy, one was in a similar projection, two were in the ipsilateral. Hemi thorax in an alternate projection, three were in the contralateral. Hemi thorax, and seven were undefined. 38% (5/13) of these patients went through recurrent aspiratory resection, and each of the five had no further pneumonic or different repeats, one of these patients a fostered cerebral metastasis 17% (4/24) of the patients had intracranial. Metastases, 13% (3/24) of the patients had bone metastases, what’s more 8% (2/24) had liver metastases after aspiratory metastasectomy. Middle opportunity to repeat after aspiratory resection was a year (6 years to 4 years). In excess of 60,000 patients with a background marked by gastric. Malignant growth is right now alive in the United States. Given the truth that dependent upon one out of 7 patients will create an aspiratory repeat and up to 1 of every 16 patients will have disconnected aspiratory metastases, our review is possibly material to a critical number of patients who have illness that is manageable to careful therapy. 7 patients to 9 patients with aspiratory metastases from gastric malignant growth are thought of as nonsurgical competitors; however those treated with chemotherapy alone have helpless endurance that is estimated on the request for a few months. In the United States, more than 60,000 patients with a history of stomach cancer are surviving today. Given that one out of every seven patients would acquire a pulmonary recurrence, and one out of every 16 patients will develop isolated pulmonary metastases, our research could benefit a large number of patients with disease that is amenable to surgical treatment. 7 patients to 9 patients with pulmonary metastases from stomach cancer are considered nonsurgical candidates, but those who are treated just with chemotherapy have a poor prognosis of many months. The majority of published reports were case reports and a few small case series from larger tertiary centers, which is understandable given the rarity of MGC resection at any site. Furthermore, almost all of the reports came from Japan, which is not surprising given that this disease is more prevalent in the East than in the West. The small number and nature of these publications suggest that a publication bias may exist. It is irrational to expect "bad outcomes" from this contentious procedure to be published. From non-anatomic wedge resections to formal lobectomies, a wide range of operations were carried out. Because the primary goal of metastasectomy is complete tumor removal with grossly and microscopically negative margins, there are numerous options for pulmonary resection of MGC. Few of these studies reported morbidity, but as pulmonary metastasectomies for other histologies have become more common, it is expected that rates of complications after MGC pulmonary resections will be comparable and acceptable.