Gram-negative bacteria are more inclined to cause thrombocytopenia than Gram-positive ones in the bloodstream infections
2 Wenzhou Medical University, Wenzhou, Zhejiang Province, China, Email: liu00794@umn.edu
#Equally contribution
Received: 25-Oct-2017 Accepted Date: Jan 10, 2018; Published: 19-Jan-2018
Citation: Lin C, Zhou X, Ying F, et al. Gram-negative bacteria are more inclined to cause thrombocytopenia than Gram-postive ones in the bloodstream infections. J Microbiol Biotechnol Rep. 2018;2(1):14-16.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Purpose: Existing studies show that some bacteria or fungi can cause thrombocytopenia by infecting the human blood. However, it remains unclear which kind of bacteria is more inclined to give rise to thrombocytopenia after infection in human blood. Through a retrospective cohort controlled trial, based on a large sample, this study analyzed the results of the patient’s blood culture and routine blood tests, so as to determine which kind of microbial infection in human blood is more likely to cause thrombocytopenia.
Study design: A retrospective cohort control trial was carried out to analyze the platelet (PLT) level and infectious bacteria strains, in 2,308 blood culture-positive and 3,786 blood culture-negative patients from 2014 to 2016.
Results: The thrombocytopenia (PLT<100) incidences of blood culture-positive patients and blood culture-negative ones were 26.0% and 14.4%, respectively (p<0.001); the thrombocytopenia incidences of patients infected with Gram-negative and Gram-positive bacteria were 29.9% and 20.4%, respectively (p<0.001).
Conclusions: Bloodstream infection can cause thrombocytopenia, and Gram-negative bacteria are more oriented to cause thrombocytopenia than Gram-positive ones.
Platelets play an important role in the processes of hemostasis, wound healing, inflammatory response, and thrombosis [1,2].The value of normal platelet count ranges from 150,000 to 440,000 platelets per cubic millimeter of human blood.3 Thrombocytopenia is a disorder characterized by an abnormally low platelet count [3,4]. Since thrombocytopenia can cause capillary and mucosal bleeding, [5] infusion of platelets should be considered when patients show symptoms of capillary or mucosal bleeding with a platelet count of less than 50 ˟ 109 per liter or when the platelet count is less than 20 ˟ 109 per liter [3]. The main cause of thrombocytopenia is that the balance between formation and destruction of platelets is broken [4]. Various factors including blood diseases, immunity, tumors, drugs, and infections can cause thrombocytopenia [6-8]. Existing studies have shown that some severe sepsis and viral infections can also cause thrombocytopenia [9-12]. However, it is still unclear that whether the bloodstream infection (BSI) and thrombocytopenia are correlated and which kind of microbial infection is more likely to cause thrombocytopenia. To resolve these two questions, a retrospective cohort controlled trial was performed on the blood culture results and platelet count of 6,094 patients who had been treated in the First Affiliated Hospital of Wenzhou Medical University from 2014 to 2016.
Methods
Study site and patients
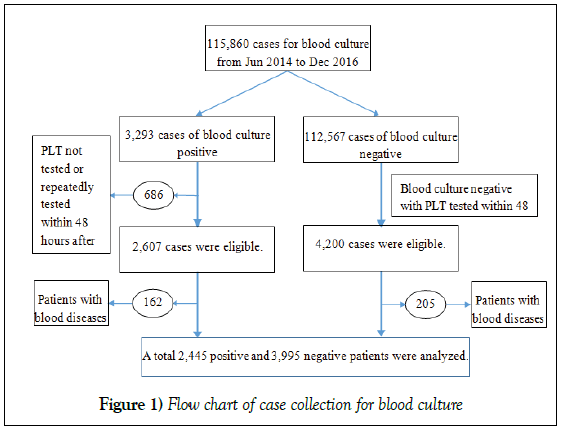
A total of 2,607 patients, which had shown positive results of blood culture and measured platelet count within 48 hours after blood collection at the First Affiliated Hospital of Wenzhou Medical University from June 2014 to December 2016, were included in this study. Two hundred and twenty-seven patients with blood diseases and senventy-two patients with hepatocirrhosis were excluded, and the remaining 2,308 were eligible. At the same time, 4,200 patients with negative blood culture were randomly collected. Three hundred and thirty-eight patients with blood diseases and seventy-six patients with hepatocirrhosis were excluded, and the remaining 3,786 were eligible (Figure 1). The differences of incidence of thrombocytopenia within hepatocirrhosis and solid tumor and the other patients were analysed.
Strain identification
The bacteria transferred from the blood culture bottle were purely cultured on a blood agar plate. Gram staining and oxidase experiments were conducted according to the instructions of the automatic microbiological analyzer. Based on these experimental results, the appropriate identification strips were selected, and the strains were identified with Vitek 2 Identification System (bioMérieux). All operations shall be conducted strictly in accordance with the instructions.
Platelet count analysis
Through sterile blood collection, 1.5 mL of venous blood was collected from a patient into the vacuum blood collection tube (Becton, Dickinson and Company) and then evenly mixed through oscillation. After that, Sysmex XE-2100 system (Sysmex Corporation) was used to count and analyze the platelets.
Statistical analysis
Pearson’s chi-squared test was performed on the comparison of thrombocytopenia percentages, and p<0.05 was considered as a statistically significant difference. Chi-square segmentation was used for comparison between multiple experimental groups.
Results
In this study, a retrospective cohort controlled trial was conducted to analyze the platelet count of 2,308 blood culture-positive and 3,786 blood culture-negative patients who had undergone treatment from June 2014 to December 2016. Among them, the blood culture-positive patients averaged 61.29 ± 16.08 (95% CI 60.64 to 61.95) years old, while the blood culturenegative patients averaged 57.00 ± 19.03 (95% CI 56.39 to 57.61) years old. The ratio of male to female was 1465:843 among the positive patients, and 2284:1502 among the negative patients. Through analysis on the patients’ blood culture result and platelets count, it was found that the thrombocytopenia incidences of the blood culture-positive and negative ones were 3.0% and 0.8% at PLT less than 20; 9.9% and 4.3% at PLT less than 50; and 26.0% and 14.4% at PLT less than 100. Then Person’s chi-squared test was performed on thrombocytopenia incidences at three PLT levels, showing significant differences between each two of them (P<0.001) (Table 1).
Table 1: Comparison of thrombocytopenia incidences in blood culture-positive and negative cases
| Positive (n=2308) | Negative (n=3786) | p value | |
|---|---|---|---|
| PLT<20 | 69 (3.0%) | 29 (0.8%) | < 0.001 |
| PLT<50 | 228 (9.9%) | 141 (4.3%) | < 0.001 |
| PLT<100 | 599 (26.0%) | 547 (14.4%) | < 0.001 |
Colonies isolated from the blood culture were classified after Gram staining, into three groups: Gram-negative bacteria, Gram-positive bacteria, and fungi. Then the three groups were analyzed at three platelet levels. Results showed that at PLT less than 20, the incidences of thrombocytopenia in the Gram-negative bacteria, Gram-positive bacteria, fungi, and blood culture-negative groups were 4.2%, 1.3%, 5.7%, and 0.8% (P<0.001); at PLT less than 50, the incidences were 11.7%, 6.7%, 20.0%, and 4.3% (P<0.001); at PLT less than 100, the incidences were29.9%, 20.9%, 30.5%, and 14.4% (P<0.001), as shown in Table 2. Then Pearson’s chi-squared test was performed on the above incidences at various platelet levels. Results showed differences in incidences between the three groups at all three levels (P<0.001). Pairwise analysis found that Gram-negative bacteria were more likely than Grampositive to cause thrombocytopenia at all three levels (P<0.001) (Table 2).
Table 2: Comparison of thrombocytopenia incidences by Gram-negative bacteria, Gram-positive bacteria and fungi
| Gram-negative bacteria (n=1177) | Gram-positive bacteria (n=999) | Fungi (N=105) | negative (n=3786) | p value | |
|---|---|---|---|---|---|
| PLT <20 | 50 (4.2%) | 13 (1.3%) | 6 (5.7) | 29 (0.8%) | <0.001 |
| PLT <50 | 138 (11.7%) | 67 (6.7%) | 21 (20.0%) | 161 (4.3%) | <0.001 |
| PLT <100 | 352 (29.9%) | 209 (20.9%) | 32 (30.5%) | 547 (14.4%) | <0.001 |
Note: By using Pearson Chi-squared test, it was found that all the p values between the Gram-negative bacteria, Gram-positive bacteria, fungi, and blood culture-negative groups were less than 0.001, suggesting that the first three groups were more likely than the negative control group to cause thrombocytopenia. Then pairwise comparison showed that the p value between the Gram-negative and Gram-positive bacteria was less than 0.001, suggesting that Gram-negative bacteria was more likely than Gram-positive bacteria to cause thrombocytopenia.
The blood culture-positive samples were identified by standard procedures, and the relationship between the strains and thrombocytopenia was analyzed (Table 3). The infectious bacteria with a percentage less than 1% among blood culture-positive bacteria (i.e., fewer than 23 cases) were not analyzed in this paper. The incidence of thrombocytopenia was compared with the negative control group, and the results were shown in Table 3.
Table 3: Comparison of thrombocytopenia incidences by different strains
| Infectious bacteria | Infected cases | Cases with PLT<100 | incidence | p value | |
|---|---|---|---|---|---|
| Pseudomonas aeruginosa | 39 | 18 | 46.2% | <0.001 | |
| Klebsiella pneumoniae | 251 | 89 | 35.5% | <0.001 | |
| Acinetobacter baumannii | 75 | 25 | 33.3% | <0.001 | |
| Candida albicans | 41 | 13 | 31.7% | 0.006 | |
| Staphylococcus aureus | 131 | 36 | 27.5% | <0.001 | |
| Escherichia coli | 419 | 109 | 26.0% | <0.001 | |
| Staphylococcus warneri | 24 | 6 | 25.0% | 0.146 | |
| Staphylococcus capitis | 63 | 15 | 23.8% | 0.046 | |
| Enterococcus faecium | 41 | 9 | 22.0% | 0.180 | |
| Staphylococcus hominis | 159 | 28 | 17.6% | 0.253 | |
| Staphylococcus haemolyticus | 71 | 12 | 16.9% | 0.501 | |
| Staphylococcus epidermidis | 167 | 28 | 16.8% | 0.432 | |
| Enterobacter cloacae | 33 | 5 | 15.2% | 0.806 | |
| Enterococcus faecalis | 24 | 3 | 12.5% | 1.00 | |
| Negative control | 3786 | 547 | 14.4% | ||
Note: The bacteria with a percentage accounting for less than 1% among the positive cases were excluded
Discussion
Existing studies have shown that hematopathy is associated with thrombocytopenia [3]. The incidence of thrombocytopenia was significantly greater in patients with cirrhosis than in the control group. The P value of the solid tumor group and the control group was greater than 0.05, so the difference was not considered. Therefore, we excluded the cases of blood diseases and cirrhosis in this experiment, and incorporated the entity tumor group into the experiment.
Through a retrospective cohort controlled trial, this paper found that the blood culture-positive (i.e., BSI) patients were more likely than the negative ones to cause thrombocytopenia, as showed in Table 1. However, the study by Stephan et al. indicated that at the surgical intensive care unit, the mortality of patients with thrombocytopenia was 18% higher than that ones with normal platelet count (mortality rate: 38% vs 20%) [13,14]. Therefore, if BSIs were timely managed, the mortality might be reduced.
Through Gram staining analysis on the infectious bacteria, it was found that Gram-negative bacteria were more likely than the positive ones to cause thrombocytopenia, as showed in Table 2. This may be due to more endotoxin produced by the Gram-negative bacteria. The study by Francois et al. found that endotoxin could induce thrombocytopenia [15]. Bacterial endotoxin inhibits platelet production by inhibiting the bone marrow megakaryocytes in patients. Through the identification of infectious strains, Pseudomonas aeruginosa, Acinetobacter baumannii and Klebsiella pneumonia were more likely to cause thrombocytopenia. In light of this, in the future management of BSI, we should be particularly cautious about the thrombocytopenia possibly caused by the infections of these bacteria.
Main messages
• Bloodstream infection can cause thrombocytopenia.
• Gram-negative bacteria are more inclined to cause thrombocytopenia than Gram-positive ones.
• Pseudomonas aeruginosa, Acinetobacter baumannii and Klebsiella pneumonia were more inclined to cause thrombocytopenia.
Current research questions
• The relationship between bloodstream infection and thrombocytopenia.
• The difference in the ability of gram-negative bacteria and positive ones to cause thrombocytopenia.
• Which strains of microbial infections in human blood is more likely to cause thrombocytopenia
Acknowledgement
We thank the patients for their participation and cooperation; the staff members from the clinical laboratory of the first affiliated hospital of Wenzhou medical university for their work in the detect of blood culture and routine blood test of the samples; Mr X.Zhong for technical support.
Contribution
X. Xue and D. Hu designed this study and wrote the paper; C.Lin, X.Zhou and F.Ying and B. Lu performed all of the studies with the assistance of Q. Wu.
Conflict-of-Interest Disclosure
The authors declare no competing financial interests.
REFERENCES
- Van Kruchten R, Cosemans JM, Heemskerk JW. Measurement of whole blood thrombus formation using parallel-plate flow chambers - a practical guide. Platelets. 2012;23:229-42.
- Swieringa F, Baaten CC, Verdoold R, et al. Platelet Control of Fibrin Distribution and Microelasticity in Thrombus Formation Under Flow. Arteriosclerosis, Thrombosis, and Vascular Biology. 2016;36:692-99.
- Organization WH. The Clinical Use of Blood Handbook. Geneva: WHO. 2001.
- Eto K, Kunishima S. Linkage between the mechanisms of thrombocytopenia and thrombopoiesis. Blood. 2016;127:1234-41.
- Greenberg EM. Thrombocytopenia: A Destruction of Platelets. Journal of infusion nursing : The Official Publication of the Infusion Nurses Society. 2017;40:41-50.
- Yamamoto T, Watarai Y, Futamura K, et al. Efficacy of eculizumab therapy for atypical hemolytic uremic syndrome recurrence and antibody-mediated rejection progress after renal transplantation with preformed donor-specific antibodies: case report. Transplantation Proceedings. 2017;49:159-162.
- Zhang W, Li M, Xiong S, et al. Decreased myeloid dendritic cells indicate a poor prognosis in patients with severe fever with thrombocytopenia syndrome. International journal of infectious diseases : official publication of the International Society for Infectious Diseases. 2017;54:113-20.
- Alhamdi Y, Abrams ST, Lane S, et al. Histone-associated thrombocytopenia in patients who are critically Ill. JAMA. 2016;315:817-19.
- Thiery-Antier N, Binquet C, Vinault S, et al. Is Thrombocytopenia an early prognostic marker in septic shock? Critical Care Medicine. 2016;44:764-72.
- Landi PJ, Fernandez Torrejon GA, Rausch S, et al. Subarachnoid hemorrhage and thrombocytopenia associated to staphylococcal bacteremia. Medicina. 2014;74:497-501.
- Pongas G, Dasgupta SK, Thiagarajan P. Antiplatelet factor 4/heparin antibodies in patients with gram negative bacteremia. Thrombosis Research. 2013;132:217-20.
- Musso D, Nhan TX, Deparis X et al. Uncommon presentation of Zika fever or co-infection? Lancet. 2016;387:1812-13.
- Stephan F, Hollande J, Richard O, et al. Thrombocytopenia in a surgical ICU. Chest. 1999;115:1363-70.
- Gafter-Gvili A, Mansur N, Bivas A, et al. Thrombocytopenia in Staphylococcus aureus bacteremia: risk factors and prognostic importance. Mayo Clinic Proceedings. 2011;86:389-96.
- Francois B, Trimoreau F, Vignon P, et al. Thrombocytopenia in the sepsis syndrome: role of hemophagocytosis and macrophage colony-stimulating factor. The American Journal of Medicine. 1997;103:114-20.