High prevalence of cervical perineural cysts on cervical spine MRI-Case series
Received: 17-Jan-2018 Accepted Date: Jan 29, 2018; Published: 13-Feb-2018, DOI: 10.37532/1308-4038.18.11.18
Citation: Gossner J. High prevalence of cervical perineural cysts on cervical spine MRI. Int J Anat Var. 2018;11(1):018-019.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The Cervical perineural (Tarlov) cysts have been reported to be a rare occurance. The frequency, distribution and possible clinical relevance of such perineural cyst in the cervical spine were studied. In a retrospective review of 41 patients undergoing cervical spine MRI 6 patients showed perineural cysts (14%). Size ranged from 4 to 12 mm and the lower cervical was predominantly affected. The reported clinical symptoms could not be correlated to the found perineural cysts. Cervical perineural cysts seem to be a common asymtomatic incidental finding. The rare diagnosis of a symptomatic perineural cyst should be made with caution and is a diagnosis of exclusion.
Keywords
MRI; Cervical spine, Perineural cysts
Introduction
In the year 1938 the American neurosurgeon Isadore Tarlov described the finding of perineural cysts of the sacral nerve roots in a cadaveric study on 30 individuals [1]. These perineural cysts or Tarlov cysts are meningeal dilatation of the posterior nerve root sheat filled with liquor. With the increased use of magnetic resonance imaging (MRI) of the lumbar spine theses perineural cysts are frequently detected. Perineural cysts have also been reported in the cervical spine. There are a few case reports describing perineural cysts of the cervical spine [2-7]. In a more systematic study Burdan et al. reported about a prevalence of 1.2% of perineural cysts in their patients undergoing MRI of the spine [8]. With the use MR-myelography perineural cystic lesions of the cervical spine seem to be a more common occurrence. To the best of our knowledge there are no reports describing the incidence, detailed morphology and possible clinical relevance in patients undergoing cervical spine MRI. Therefore in a small retrospective case series MRI scans of the cervical spine were analysed for the presence of perineural cysts. In cases of cervical perineural cysts, a morphological analysis and a chart review for possible association with clinical symptoms was performed.
Methods
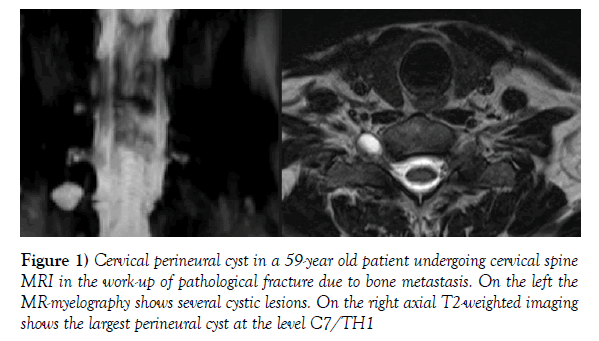
This retrospective study was performed in accordance to the statute of the ethics committee of the affiliated University of Gottingen. From the departmental radiology information system 41 consecutive cervical MRI scans performed between September 2016 and November 2017 were identified. The sample consisted of 19 male and 22 female patients with a mean age of 57.8 years (range 11-86 years). All patients were examined using the same 1.5 Tesla Scanner (Siemens Magentom Avanto, Siemens Healthcare, and Erlangen, Germany). Basis sagittal T1- and T2- weighted as well as axial T2-weighted sequences were performed. Additional heavy T2- weighted coronal volume sequences with MIP- reconstructions (MR-myelography) were performed. All examinations were examined on a standard medical workstation using the departmental PACS (Synedra view personal, Synedra information technologies, Innsbruck, Austria). Initially the MR-myelography was reviewed for the presence of small cystic lesions at the exit of the cervical nerve roots. The findings were correlated with the other sequences, especially the axial T2- weighted images. The diagnosis of a cervical perineiral cyst was made if a small rounded cystic lesion along the exit of the nerve root could also be found on axial T2- weighted images (Figure 1). Very small cystic lesions (<2 mm) of the proximal nerve roots or lesions not detectable as distinct small cystic lesion on axial T2-weighted images were not recorded. In patients with cervical perineural cysts a detailed anatomical analysis as well as a chart review was performed. A descriptive statistics was performed.
Figure 1) Cervical perineural cyst in a 59-year old patient undergoing cervical spine MRI in the work-up of pathological fracture due to bone metastasis. On the left the MR-myelography shows several cystic lesions. On the right axial T2-weighted imaging shows the largest perineural cyst at the level C7/TH1
Results
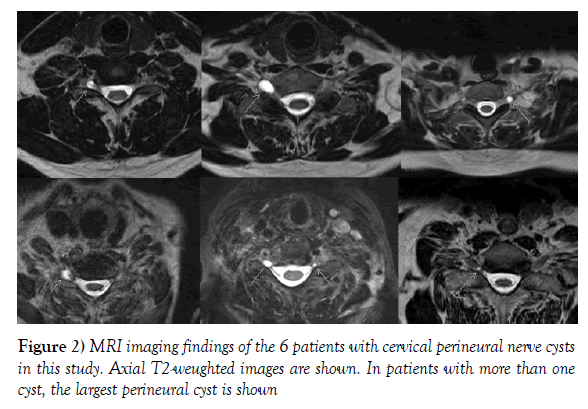
In this series 6 patients showed cervical perineural cysts, i.e. incidence in this sample was 14%. Single cervical perineural cysts were found in 3 patients; in 3 patients two or more cysts were observed. Cervical perineural nerve cysts occurred in men and women equally. The most common affected levels were C6/7 and C7/Th1 (Figure 2). Size ranged from 3 to 12 mm. Using the patients clinical data none of the perineural cysts could be correlated to the clinical symptoms. A detailed description is given in Table 1.
| Patient | Age | Gender | Number of Cervical perineural cysts |
Level | Size | Affected side | Indication for imaging |
|---|---|---|---|---|---|---|---|
| 1 | 28 | male | 1 | C6/C7 | 6.5 mm | Right | Adhesive capsulitis of the shoulder, MRI to rule out Disc prolapse |
| 2 | 82 | female | 1 | C6/C7 | 10 mm | Right | Pseudarthrosis of C1 fracture |
| 3 | 59 | male | 4 | C5/6 C6/7 C7/TH1 |
4- 12 mm | Bilateral | Bone metastasis |
| 4 | 49 | female | 4 | C7/TH1 TH1/TH2 |
4-7.5 mm | Bilateral | C7 syndrom on the left |
| 5 | 72 | female | 2 | C6/C7 | 3 and 7.5 mm | Bilateral | Rheumatoid arthritis |
| 6 | 70 | male | 1 | C7/TH1 | 4 mm | Right | Vitamin B defiency, MRI to rule out myelopathy |
Table 1: Morphological and clinical data of patients with cervical perineural cysts
Discussion
Perineural cysts or Tarlov cysts are pathological fluid collections located between the peri- and endoneurium, i.e. meningeal dilatations of the nerve sheat at the dorsal root ganglion [2,6,9]. They are filled with liquor, therefore the signal is isointense to liquor on all MRI sequences. Especially at sacral level perineural cysts can get relatively large and may lead to bone remodelling with enlargement of the neural exit and/or the sacral foramina [6]. It has been shown that perineural cysts have microconnections to the subarachnoid space and the hydostatic pressure of the cerebrospinal fluids leads to the dilatation of the meningeal layers and cyst formation. It has been discussed, that in some perineural cysts a valve-like mechanism may exist, i.e. cerebrospinal fluid can move inside the cyst, but cannot leave. This leads to progressive enlargement. It may be speculated that these cysts with a valve like mechanism are prone to become symptomatic [9]. The etiology of this cyst formations has been discussed [2-7,9]. Some authors favour an inflammatory pathogenesis with inflammation leading to increased fluid influx into the cyst or a posttraumatic pathogenesis with old micro hemorrhages and hemosiderin deposition leading to the above mentioned valve-like mechanism. Other authors discuss a developmental or congenital origin [2-7,9]. In the original report Tarlov reported about sacral perineural cysts, but perineural cysts can be found at every spine level [1-9]. Cervical perineural cysts have been demonstrated in myelography, but with use of MRI they are increasingly found [8,10]. In a systematic study Burdan et al. reported about a prevalence of 1.2% of perineural cysts, they found 6 cervical perineural cysts in 514 MRI scans [8]. In our case series 6 out of 41 patients undergoing cervical spine MRI showed perineural cysts, i.e. an incidence of 14%. This high frequency needs to be explained. First our case series is quite small with 41 consecutive cervical MRI scans and selection bias may play a role. Another explanation is the used imaging technique. With the use of MIP-reconstructions in MR-myelography even very small cystic lesions at the nerve roots can be seen and correlated on other conventional T2- weighted sequences. The image appearance itself of small perineural cysts has a benign appearance and the reporting radiologists may assess it as a small incidental finding not to be worth mentioned in the report. And, as there are only a few reports in the literature radiologists may be not aware of the existence of cervical perineural cysts and may therefore make another differential diagnosis like facet ganglion cysts or a nerve sheat tumor. Despite the differences of reported incidences between the study of Burdan et al. and our case series cervical perineural cysts are not a rare occurrence. In our case series there was no sex predeliction, in contrast Burdan et al. reported cervical perineural cysts in women only [8]. It has been stated that in sacral perineural cysts less than 1% are symptomatic [1,9]. This seems to be true also for cervical perineural cysts. In the literature there are only 5 case reports about symptomatic cervical perineural cysts [2-5,7]. In none of our patients the presence of perineural cysts could be correlated to the symptomatology (given the obvious limitations of a retrospective chart review). I.e. cervical perineurals cysts per se are not rare, but symptomatic perineural cysts are rare. Bayrakli et al. describe the case of a cervical perineural cyst presenting with symptoms of a cubital tunnel syndrome. A cervical perineural cyst at the C8 nerve root was found. After the initiation of steroid medication and physical therapy symptoms improved and the initially diminished muscle strength has returned to a normal level [2]. Kim et al. described the case of a patient with long standing cervicobrachialgias and a perineural cyst at the C8 root. The patient received 3 transformainal epidural steroid injections, which provided a long-term relief. On follow up imaging shrinkage of the perineural cyst could be detected [3]. Joshi et al. reported about a central perineural cyst masquerading a tumor, the cyst was located intra spinally and caused compression of the cervical myelon. An operation was performed and the symptoms disappeared [4]. Zibis et al. described the case of a patient with a C6-syndrome and a cervical perineural cyst at the C6 nerve root. A conservative approach with a soft cervical collar and non-steroidal antiinflammatory medication for 2 weeks was choosen. At the 24 months follow up a symptom reaction of 90% was reported [5]. Dugan et al. reported about a patient with several cervical and thoracic perineural cysts causing a thoracic outlet syndrome. The patient improved with a multimodality pain treatment (including physical and occupational therapy as well as teaching of coping skills) [7]. In the case reports only one patient was operated because of spinal cord compression, in the remaining cases different conservative or minimal invasive approaches showed therapeutic efficacy. The small number of case reports suggests a very low incidence of symptomatic cervical perineural cysts. I.e. the diagnosis of a symptomatic perineural cyst should be made with caution and is in our opinion a diagnosis of exclusion.
Conclusion
Cervical perineural cysts are a quite common finding and can be frequently found in patients undergoing MRI of the cervical spine. In most cases they seem to be incidental findings lacking clinical relevance. The rare diagnosis of a symptomatic perineural cyst should be made with caution and is a diagnosis of exclusion.
REFERENCES
- Konar SK, Bir SC, Maiti TK, et al. Isadore Max Tarlov (1905-1977) and the controversial Tarlov cyst: historical perspective. J Neurosurg Spine. 2016;24:510-3.
- Bayrakli F, Kurtuncu M, Karaarslan E, et al. Perineural cyst presenting like cubital tunnel syndrome. Eur Spine J. 2012;21:S387-9.
- Kim K, Chun SW, Chung SG. A case of symptomatic cervical perineural (Tarlov) cyst: clinical manifestation and management. Skelet Radiol. 2012;41:97-101.
- Poshi VP, Zanwar A, Karande A, et al. Cervical perineural cyst masquerading as a cervical spinal tumor. Asian Spine J. 2014;8:202-5.
- Zibis AH, Fyllos AH, Arvanitis DL. Symptomatic cervical perineural (Tarlov) cyst: a case report. Hippokratia. 2015; 19:76-7.
- Cheong WK, Wong BSV. Clinics in diagnostic imaging (181). Cervical spine perineural cyst. Singapore Med J 2017;58:636-641.
- Dugan SE, Oken JE. Poster 485 A rare case of multiple cervical and thoracic tarlov cysts presenting at thoracic outlet syndrome. PM&R. 2014;6:S355-6.
- Burdan F, Mocarska A, Janczarek M, et al. Incidence of spinal perineural (Tarlov) cysts among east European patients. PLoS ONE. 2013;8:e71514.
- Lucantoni C, Than KD, Wang AC, et al. Tarlov cysts: a controversial lesion of the sacral spine. Neurosurg Focus. 2011;31:E14.
- Smith DT. Multiple meningeal diverticula (perineural cysts) of the cervical region disclosed by pantopaque myelography. Report of a case. J Neurosurg. 1962;19:599-601.