How evolution of quorum sensing must fit into the understanding of the origin, prevention and treatment of cancer
Received: 16-Oct-2018 Accepted Date: Nov 20, 2018; Published: 30-Nov-2018
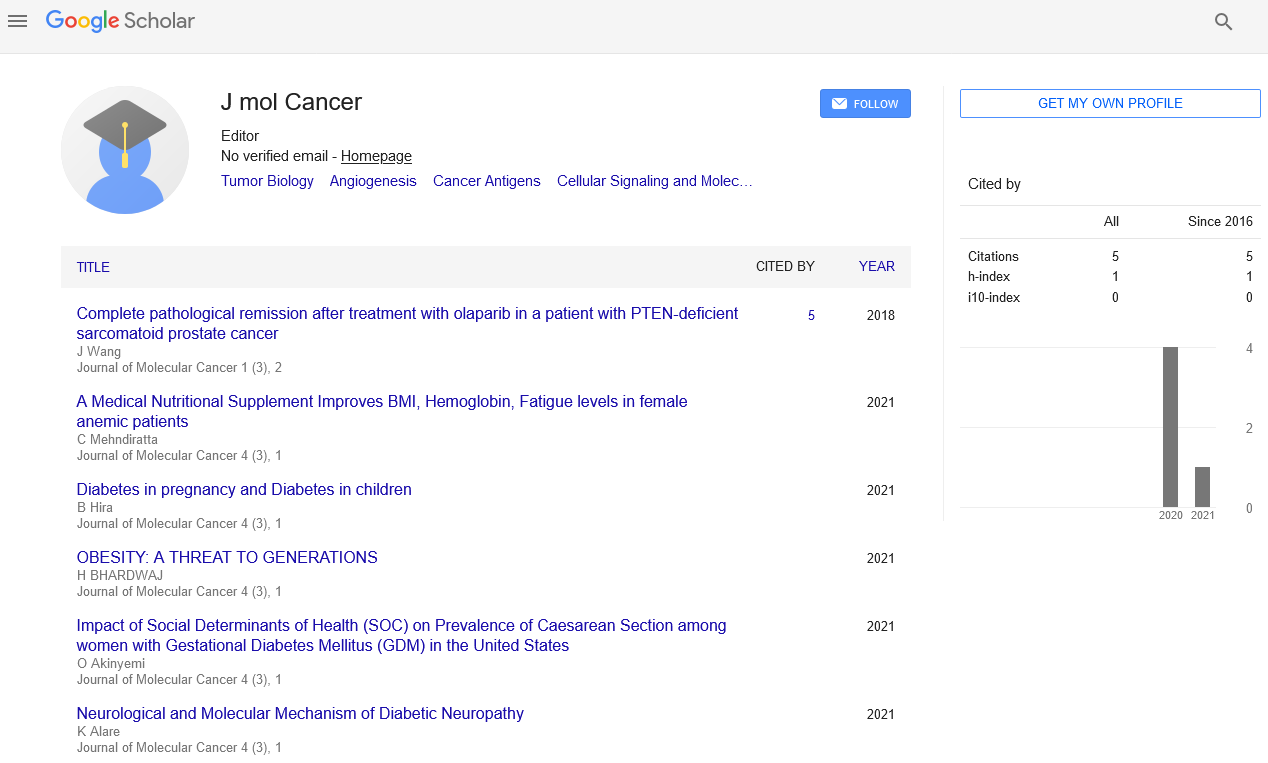
Citation: James E. Trosko. How evolution of quorum sensing must fit into the understanding of the origin, prevention and treatment of cancer. J Mol Cancer. 2018;1(3):22-24.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Keywords
Gap junctional intercellular communication; Adult stem cells; Epigenesis; evolution of cancer; OCT4A; Mutagenesis; Multi-step process of carcinogenesis.
This review applies the mechanism of “cell-cell signaling in sustaining and perpetuating homeostasis, starting with the reduction in intracellular entropy as the organizing principle for metazoan evolution”[1].
How Evolutionary Mechanisms of Mutagenesis and Epigenesis at the Organ-Specific Adult Stem Cell Level in the Multi-Cellular Metazoans Contribute to the Resistant “Cancer Stem Cells”
Currently, cancer is still a major global health problem, whether the disease is strongly correlated to smoking, alcohol, diet, viruses, exposure to sun light, lack of exercise, inherited cancer-predisposing genes, exposure to mutagenic or epigenetic chemicals, etc.; whether the types of cancers varies from nation to nation, ethnic group to ethnic group; or whether it seems to be somewhat resistant to prevention or therapy. In the paper to which I would like to add a “Commentary”, I wanted to point out that in the basic cancer research field and translational- therapeutic field, the success or failure of the new fields of “bioinformatics”, “precision medicine”, “cancer stem cells”, together with extremely sophisticated technologies of CRISPR, or single cell molecular analyses, will depend on a much broader view of human carcinogenesis than what traditional approaches can provide. This was seen by Hanahan and Weinberg [2]: “Some would argue that the search for the origin and treatment of this disease will continue over the next quarter century in much the same manner as it has in the recent past, by adding further layers of complexity to a scientific literature that is already complex beyond measure. But we anticipate otherwise: those researching the cancer [or any other disease] problem will be practicing a dramatically different type of science than we have experienced over the last 25 years. Surely much of this change will be apparent on the technical level. But ultimately, the more fundamental change will be conceptual.”
In general, so many concepts need to integrate the various scientific disciplinary fields (evolution; genetics; epigenetics; stem cell biology, microbiology (viruses, microbiome), immunology; nutrition, etc.) with psychological, social, economic, political, and cultural factors. First, cancer is clearly not a new disease [3], simply because human DNA, which plays several roles in the carcinogenic process, either by specific genes being mutated or epigenetically altered, is not immune to these potentially disrupting molecular processes [4]. Second, the cell, in a multi-cellular organism, is the unit by which the evolutionary forces act to maintain homeostasis for health. Third, the human carcinogenic process is a multi-step, multimechanism process [5-7], consisting of the “initiation” of a single normal cell to an “immortalized” cell; the “promotion” or clonal amplification of this initiated cell by the stimulation of proliferation and the blockage of apoptosis [8], and the “progression” state, where an initiated cell in this promoted clone acquires the ability to invade tissues and to metastasize. Fourth, while each cancer starts from a single cell, by the time an invasive metastatic cancer appears, the population of the tumor is both genotypically and phenotypically heterogeneous, consisting of “cancer stem cells” and “cancer non-stem cells”, interacting with each other and the other normal stromal and immune cells, as well as the extra-cellular matrices [9,10]. This complexity of cell interactions, as seen by Potter [11], creates that major challenge to the erroneous idea that a single preventive and therapeutic approach to cancer management can be performed. “The cancer problem is not merely a cell problem, it is a problem of cell interaction, not only within tissues, but also with distal cells in other tissues. But in stressing the whole organism, we must also remember that the integration of normal cells with the welfare of the whole organisms is brought about entirely by molecular messages acting on molecular receptors” [11].
The major objective of my original paper on “Quorum Sensing” [12] tried to point out that during the evolution of single cell organisms, primitive communication signals between the population of these single cells was selected to protect both the individual cell and the species by forcing them to go into a dormant phase when nutrients or other conditions, needed for life, would jeopardize their survival if ignored. Obviously, the so-called “drugresistant” bacteria appeared when that survival mechanism was disrupted and when the quorum signal was ignored. Today, this same phenomenon of cancer drug resistance has been a typical phenomenon found in cancer therapy. Until recently, the common explanation has been that the drug resistance of cancer cells was the result of radiation/chemotherapy and immunotherapy ability to induce mutations in the cancer population by the therapy itself. More recently, with the concept of stem cells, based on some stem cell biology [13-16], the appearance of therapy-resistant cancer cells is probably due to a selection of therapy resistant “cancer stem cells”, either because of better DNA repair [17], or of expressed drug transporter genes [18,19]. In both cases of drug resistant bacteria or therapy- resistant cancer cells, there is a biologically- based evolutionary basis for this phenomenon.
The Fundamental Assumption of the Origin of Cancer-Resistant Cells
In the original paper on “Quorum Sensing” in multi-cellular organisms, it was assumed that, of the two opposing hypotheses of the single cell origin of the “cancer stem cell”, namely the normal cell, that was “initiated”, was an organ-specific adult stem cell (the Stem Cell hypothesis) [20-24] or that it was a somatic differentiated cell that was “de-differentiated” or “re-programmed” [25]. Further, because the “initiation” event in that cell was an “irreversible” event, it was assumed that a mutagenic event had occurred [26]. Now, here is the critical fact that seems to be missed. Mutations can occur as a result of an “error of DNA repair”, best exemplified by the skin cancer prone, “Xeroderma Pigmentosum Syndrome” [27-30] after the skin is exposed to ultraviolet light. Yet, normally, one rarely sees any discussion of another means by which a mutation can occur, namely by the process of an “error of DNA replication”, as seen in the cancer prone, Blooms syndrome [31,32]. In other words, every time an adult stem cell is stimulated to proliferate, there is always a finite chance that a mutation could occur, without any pre-existing DNA damage. This implies that, while stem cells are, under normal conditions usually quiescent, under rapid tissue growth or under several tissue injury or cell death or removal, stem cells are recruited into compensatory hyperplasia. One of the major epidemiological questions raised in the case of human cigarette -induced lung cancer, “How does one explain lung cancers in nonsmokers?” While exposure to “downstream” smoke is one explanation, the fact that initiated cells exist in all of us, some due to “errors of DNA repair”, others are due to errors in DNA replication”. It might be that non-smokers have lung cancers because they have been exposed to epigenetic, tumor promoting conditions/chemicals that stimulated the clonal expansion of the pre-existing, spontaneously- generated initiated lung adult stem cells, which were generated by “errors of DNA replication”.
Are All Cancer Stem Cells Alike?
Of course, while we still are not sure of the biological nature of any or all cancer stem cells, there is some strong evidence that cancer stem cells did originate from normal adult organ-specific stem cells [33,34]. Moreover, Loewenstein and Kanno [35] first speculated that there seemed to be a universal phenotype of cancer cells, namely they did not “contact inhibit”; did not have growth control; did not terminally differentiate and were seemingly “immortal”. One major characteristic, they argued, was a lack of Gap Junctional Intercellular Communication (GJIC). At that time, Loewenstein and Kanno did not know about one characteristic of normal stem cells, namely they did not express connexin or gap junction genes [36]. Nor did Loewenstein and Kanno [35] know that tumor promoting, epigenetic chemicals, such as phorbol esters or DDT, could reversibly inhibit GJIC [37]. Further, Loewenstein and Kanno did not know that various viruses (SV-40; HPV) or oncogenes (H-Ras; Src, Neu, etc) could stably inhibit gap junction function) [38-40]. Since the Oct-4A gene has been associated with both normal adult stem cells and many cancer stem cells [33,41], the question is , “If all cancer cells lack growth control, lack terminal differentiation and lack GJIC function, could there be two kinds of cancer stem cells that lack GJIC?” [42]. The answer would seem to be, “Yes”. There are those that originated in the adult undifferentiated organ-specific stem cell, expressing the OCT4A gene but not the connexin genes. These would be very “embryonic-like”, such as the “flat-type” human colon cancer cells [43]. The other cancer stem cells might have originated in an early-differentiated adult stem cell, whose Oct4A gene has been repressed and its gap junction gene, needed for differentiation, has been expressed, but that the gap junction function has been rendered non-functional by some oncogene or virus [44,45]. The “polyp-type” human colon tumor might represent this type. The implication of this interpretation explains why two tumors might not respond to the same therapy, since a stem cell-derived Oct4A expressing, non-connexin expressing, and a drug transporter gene- cancer stem cell would require a cancer drug to repress the Oct4A gene and the drug-transporter gene but to express the transcription of the connexin gene to establish functional gap junctional intercellular communication [46]. On the other hand, the cancer stem cells, which expresses the connexin genes, but also has expressed oncogenes or oncogenic viruses, post-translation- inhibitors to the SV40, HPV or other viral proteins would be needed to re-establish GJIC.
Conclusion
The essence of the original “Quorum Sensing” paper was that through the evolutionary process, both single cell and multi-cellular organisms developed adaptive communication mechanisms that allowed these cells to survive during moments of stress. However, in both cases of the single cell organism and of the multi-cellular organism, the “Quorum Sensing” mechanisms could be disrupted, causing the homeostatic regulation of proliferation (and differentiation in the case of multi-cellular organisms). Drug-resistance bacteria and therapeutic resistant cancer cells are the ultimate end result of this disruption of quorum sensing. Based on the original “Quorum Sensing” paper, this “Commentary” has tried to re-emphasize the fact that the initiation of a normal organ-specific adult stem cell is the inevitable consequence of the evolutionary process of mutagenesis, that can occur by either an “error of DNA repair” of damage caused by some environmental agent or by an “error of DNA replication” in adult stem cells when they are forced to expand their population for tissue growth or by “compensatory hyperplasia”, after there has been significant cell death or cell removal. In other words, mutagenesis is a double-edge sword both the creation of new adaptive genes that leads to evolutionary survival of the species, and for the disruption of genes, needed to maintain homeostatic control of cells for health of somatic cells, but could lead to diseases.
The evolution of multi-cellularity also gave rise to stem cell niches, organspecific stem cells, and the dual process of symmetrical and asymmetrical stem cell division; new mechanisms (“Epigenesist”) to regulate the expression of specific sets of genes in the total genome, required for tissue differentiation, and senescence of cells.
Lastly, all cancer stem cells seem to lack GJIC, however, there are two types, those that never express their connexin genes but express OCT4A, and those that do express the connexin genes, but not OCT4A gene, yet the connexin proteins are unable to form functional gap junctions, because they have been inactivated by some viral proteins or activated oncogenes. This implies, anticancer therapy has to be designed to attack these two very different “cancer stem cells”, such that the phenotypes of these two cancer stem cells would be very different. Lastly, health or pathologies are the result of evolution, via mechanisms of mutagenesis and epigenetic alteration of genes, acting on the cell level via the integrated cell-cell communication mechanisms in multicellular metazoans.
Acknowledgement
To all my former undergraduate, graduate and medical students, postdoctoral fellows, Visiting Scholars and Collaborating Colleagues, I wish to thank you for providing the experimental results and stimulating discussions over my 50 years of laboratory research.
REFERENCES
- Torday JS. Evolutionary biology redux. Perspect Biol Med. 2014;56:455-84.
- Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100:57-70.
- Carruba G, Trosko JE. The long evolutionary journey of cancer from ancestor to modern humans. Crit Rev Oncog. 2017;22: 323-52.
- Trosko JE. Reflections on the use of 10 IARC carcinogenic characteristics for an objective approach to identifying and organizing certain mechanistic studies. Tox Res Appl. 2017;1:1-10.
- Weinstein IB, Gattoni CS, Kirschmeier P, et al. Multistage carcinogenesis involves multiple genes and multiple mechanisms. J Cell Physiol. 1984;121:127-37.
- Pitot HC, Dragan YP. Facts and theories concerning the mechanisms of carcinogenesis. FASEB J. 1991;5:2280-86.
- Pitot HC. Progression: The terminal stage of carcinogenesis. Jpn J Cancer Res. 1989;80:599-607.
- Trosko JE. Modulation of cell-cell communication and epigenetic mechanisms as a shared cellular mechanism in diverse childhood brain diseases, such as cancer and autism. EC Neurology. 2018;10:134-56.
- Al Hajj M, Wicha MS, Benito-Hernandez A, et al. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA. 2003;100:3983-88.
- Atena M, Reza AM, Meehran G. A review on the biology of cancer stem cells. Stem Cell Discovery. 2014;4:83-9.
- Potter VR. Phenotypic diversity in experimental hepatomas: The concept of partially blocked ontogeny. Br J Cancer. 1978;38:1-23.
- Trosko JE. Evolution of microbial quorum sensing to human global quorum sensing: An insight to how gap junctional intercellular communication might be linked to global metabolic disease crisis. Biology. 2016;5:E29.
- Armstrong L, Tilgner K, Saretzki G, et al. Human induced pluripotent stem cell lines show stress defense mechanisms and mitochondrial regulation similar to those of human embryonic stem cells. Stem Cells. 2010;28:661–73.
- Nesti C, Pasquali L, Vaglini F, et al. The role of mitochondria in stem cell biology. Biosci Rep. 2007;27:165–71.
- Trosko JE, Chang CC, Wilson MR, et al. Gap junctions and the regulation of cellular functions of stem cells during development and differentiation. Methods. 2000; 20:245-64.
- Trosko JE, Kang KS. Evolution of energy metabolism, stem cells and cancer stem cells: how the Warburg and Barker hypotheses might be linked. Int J Stem Cells. 2012;5:39-56.
- Kim Y, Joo KM, Jin J, et al. Cancer stem cells and their mechanism of chemo-radiation resistance. Int J Stem Cells. 2009;2:109-14.
- Kim M, Turnquist H, Jackson J, et al. The multidrug resistance transporter ABCG2 (Breast cancer resistance protein 1 effluxes Hoechst 33342 and is overexpressed in hematopoietic stem cells. Clinical Cancer Res. 2002;8,22-8.
- Micelli V, Cocciadiferro L, Maurizio Z, et al. Molecular profiling of potential human prostate cancer stem cells. J Stem Cell Res Ther. 2011;S7:1-9.
- Markert CL. Neoplasia: A disease of differentiation. Cancer Res. 1968;28:1908-14.
- Pierce B. Neoplasms, differentiation and mutations. Am J Pathol. 1974;77:103-18.
- Trosko JE. Cancer stem cells and cancer non-stem cells: From adult stem cells or from re-programming of differentiated somatic cells. Vet Pathol. 2009;46:176-93.
- Till JE. Stem cells in differentiation and neoplasia. J Cell Physiol. 1982;113:3-11.
- Greaves MF. Differentiation-linked leukemogenesis in lymphocytes. Science. 1986;234:697-704.
- Sell S. Cellular origin of cancer: Differentiation or stem cell maturation arrest? Environ Health Perspect. 1993;101:15-26.
- Trosko JE, Carruba G. Bad Luck mutation: DNA mutations are not the whole answer to understanding cancer risks. Dose-Response. 2017;15:1-7.
- Cleaver JE, Trosko JE. Absence of excision of ultraviolet-induced cyclobutane dimers in Xeroderma pigmentosum. Photochem Photobiol. 1970;11:547-50.
- Maher VM, McCormick JJ. Effect of DNA repair on the cytotoxicity and mutagenicity of UV irradiation and of chemical carcinogens in normal and xeroderma pigmentosum cells. Raven Press. 1976;8:129-45.
- Glover TW, Chang CC, Trosko JE, et al. Ultraviolet light induction of diphtheria toxin resistant mutations in normal and xeroderma pigmentosum human fibroblasts. Proc Natl Acad Sci USA. 1979;76:3982-86.
- Brash DE, Rudolph JE, Simon JA, et al. A role for sunlight in skin cancer: UVinduced p53 mutations in squamous cell carcinomas. Proc Natl Acad Sci USA. 1991;88:10124-28.
- German J. Bloom syndrome: A Mendelian prototype: somatic mutations and disease. Medicine. 1993;72:393-406.
- Warren ST, Schultz RA, Chang CC, et al. Elevated spontaneous mutation rate in Bloom syndrome fibroblasts. Proc Natl Acad Sci USA. 1981;78:3133-37.
- Tai MH, Chang CC, Kiupel M, et al. Oct-4 expression in adult human stem cells: evidence in support of the stem cell theory of carcinogenesis. Carcinogenesis. 2005;26:495-502.
- Vries RG, Huch M, Clevers H. Stem cells and cancer of the stomach and intestine. Mol Oncol. 2010;4:373-84.
- Loewenstein WR, Kanno Y. Intercellular communication and the control of tissue growth: Lack of communication between cancer cells. Nature. 1966;209:1248-9.
- Trosko JE. A conceptual integration of extra-, intra-, and gap junctional inter- cellular communication in the evolution of multi-cellularity and stem cells: How disrupted cell-cell communication during development can affect diseases later in life Int J Stem Cell Res Ther. 2016;3:1-6.
- Yotti LP, Chang CC, Trosko JE. Elimination of metabolic cooperation in Chinese hamster cells by a tumor promoter. Science. 1979;206:1089-91.
- Kao CY, Nomata K, Oakley CS, et al. Two types of normal human breast epithelial cells derived from reduction mammoplasty. Phenotypic characterization and response to SV40 transfection. Carcinogenesis. 1995;16:531-8.
- Trosko JE, Ruch RJ. Cell-cell communication in carcinogenesis. Front Biosci. 1998;3:208-36.
- De Feijter AW, Ray JS, Weghorst CM, et al. Infection of rat liver epithelial cells with V-Ha-ras: Correlation between oncogene expression, gap junctional communication, and tumorigenicity. Mol Carcinog. 1990;3:54-67.
- Zhou Y, Chen X, Kang B, et al. Endogenous authentic OCT4A proteins directly regulate FOS/AP-1 transcription in somatic cancer cells. Cell Death Dis. 2018;9:585.
- Trosko JE. The role of stem cells and gap junctional intercellular communication in carcinogenesis. J Biochem Mol Biol. 2003;36:43-8.
- Trosko JE, Lenz HJ. Review: What roles do colon stem cells and gap junctions play in the left and right location of the origin of colorectal cancers. J Cell Commun Signal. 2017;11:79- 87.
- Ahuja D, Sáenz-Robles MT, Pipas JM. SV40 large T antigen targets multiple cellular pathways to elicit cellular trans formation. Oncogene. 2005;24:7729-45.
- Trosko JE. The gap junction as a ‘Biological Rosetta Stone’: Implications of evolution, stem cells to homeostatic regulation of health and disease in the Barker Hypothesis. J Cell Commun Signal. 2011;5:53-66.
- Ogawa T, Hayashi T, Tokunou M, et al. Suberoylanilide hydroxamic acid enhances gap junctional intercellular communication via acetylation of histone containing connexin43 gene locus. Cancer Res. 2005;65:9771-8.