Iatrogenic peroneal arteriovenous fistula successfully treated lower limb ischemia
2 Department of Radiology, Pauls Stradins Clinical University Hospital, Latvia, Email: janis@anatomystandard.com
Received: 11-Nov-2020 Accepted Date: Nov 26, 2020; Published: 03-Dec-2020, DOI: 10.37532/1983-8905.2021.14(1).4-5
Citation: Lacis A, Savlovskis J, Kupcs K, Strods V, Andris V. Iatrogenic peroneal arteriovenous fistula successfully treated lower limb ischemia. J Phlebol Lymphol.14(1):4-5.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Critical Limb Ischaemia (CLI) is the clinical end stage of Peripheral Artery Disease (PAD) associated with a high risk of major amputation, cardiovascular events, poor quality of life and death. Bypass surgery and/or endovascular interventions are the first-line treatment of choice in these cases to prevent amputation and resolve rest pain. Other treatment methods are either in the study phase (gene and stem cell therapy) or have little or no effect (vasoactive therapy or spinal cord stimulation). Unfortunately, about 15%-20% of CLI patients are not candidates for distal revascularization because of a lack of target outflow vessels. Surgical Deep Venous Arterialization (DVA) provides reverse flow to the capillary beds and increases collaterals. DVA may be considered as a viable alternative before major amputation in patients with CLI due to an unreconstructable lower extremity arterial disease.Keywords
Critical limb ischaemia; Deep venous; arterialisation
Introduction
A 73-year-old male was admitted to Pauls Stradins Clinical University Hospital with complaints about severe claudication and rest pain since a non-healing ulcer of the medial surface of the distal right calf appeared three months before hospitalization. The symptoms developed gradually during the preceding year.
Case Report
Clinically, he had Rutherford category 5 ischemia at high risk of amputation based on the Society for Vascular Surgery’s WIfI (grade 1 wound, grade 3 ischemia, and grade 2 foot infection) classification.
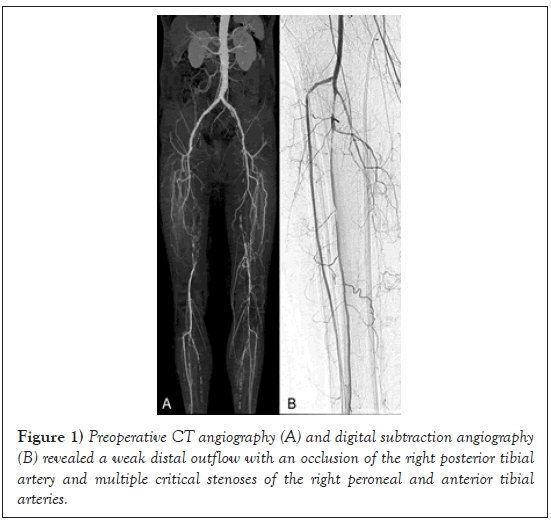
A Computed Tomography Angiography (CTA) examination revealed a long occlusion of the superficial femoral artery with advanced atherosclerosis of the crural arteries and poor plantar artery runoff (Figure 1).
Figure 1: Preoperative CT angiography (A) and digital subtraction angiography (B) revealed a weak distal outflow with an occlusion of the right posterior tibial artery and multiple critical stenoses of the right peroneal and anterior tibial arteries.
Despite the ulcer and severely calcified peripheral arteries the patient underwent distal femoro-popliteal bypass with an 8 mm synthetic prosthesis, because the great saphenous vein was not suitable for reconstruction.
Revision of the femoropopliteal bypass distal anastomosis shortly before its closing revealed the absence of retrograde blood flow. Four thrombectomy attempts with 4F Fogarty balloon catheter resituated the weak retrograde bloodstream and anastomosis was closed.
A dual antiplatelet therapy with 100 mg/d of acetylsalicylic acid and 75 mg/d of clopidogrel was started postoperatively.
On the first day after the revascularization, the patient had less severe ischemic pain but experienced a significant swelling of the right calf.
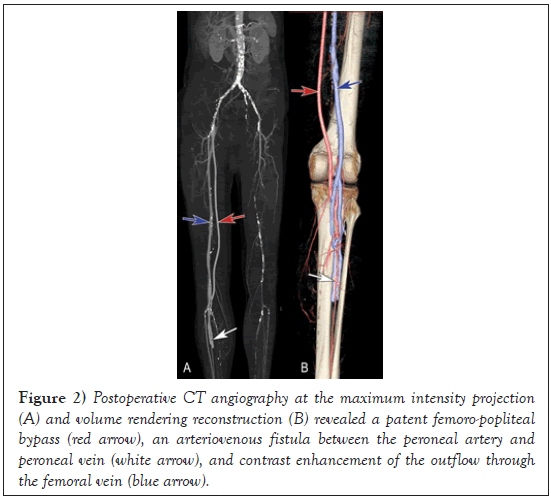
Postoperative CTA revealed good functioning of the distal anastomosis of the femoropoliteal bypass but at the same time an interosseous arteriovenous fistula (Figure 2).
Figure 2: Postoperative CT angiography at the maximum intensity projection (A) and volume rendering reconstruction (B) revealed a patent femoro-popliteal bypass (red arrow), an arteriovenous fistula between the peroneal artery and peroneal vein (white arrow), and contrast enhancement of the outflow through the femoral vein (blue arrow).
According to actual clinical and angiographic findings, 5000 IU heparin was administered in addition four times a day subcutaneously in combination with the right shin compression with elastic bandage and with of the foot of the bed raised.
The administration of heparin was cancelled on the third postoperative day because calf swelling significantly decreased. The patient was discharged on the 10th postoperative day on dual antiplatelet therapy.
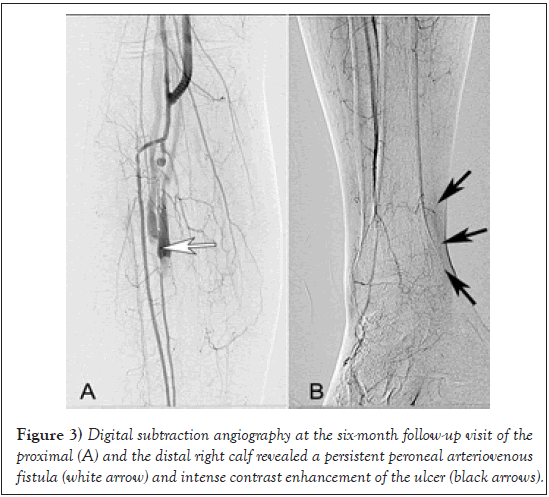
At the six-month follow-up visit, the patient noted that ischemic rest pain had ended. A slight swelling of the right calf and active granulation of the ulcer were observed during the dressing of the wound. Postoperative CTA revealed good retrograde filling of the small distal venous channels in the ulcer area and the initial arterialization of the peripheral venous set (Figure 3).
Figure 3: Digital subtraction angiography at the six-month follow-up visit of the proximal (A) and the distal right calf revealed a persistent peroneal arteriovenous fistula (white arrow) and intense contrast enhancement of the ulcer (black arrows).
Results and Discussion
Critical Limb Ischaemia (CLI) is the clinical end stage of Peripheral Artery Disease (PAD) associated with a high risk of major amputation, cardiovascular events, poor quality of life and death. Studies have shown the development of peripheral complications (ulcer, gangrene, infection, high risk of limb amputation) in 10%-40% of cases and mortality in 20% of patients within the first six months of primary CLI diagnosis, as well as up to 50% possible mortality rate over the first five years from coronary artery disease and cerebrovascular artery disease [1].
Bypass surgery and/or endovascular interventions are the first-line treatment in these cases. Other treatment methods are either in the study phase (gene and stem cell therapy) or have a little or no effect (vasoactive therapy or spinal cord stimulation). Unfortunately, about 15%-20% of CLI patients are not candidates for distal revascularization because of lack of target outflow vessels [2,3].
Surgical Deep Venous Arterialization (DVA) uses a venous bed as an alternative conduit for the perfusion of peripheral tissues, thus providing reverse flow to the capillary beds and increasing collaterals [4]. The effect of DVA can be explained by at least two mechanisms: angiogenic growth factors that triggered neovascularization and reversed perfusion of arterioles through the capillary network that results in increased oxygenation to the ischemic tissues [5].
DVA includes not only a connection between an arterial inflow and a venous outflow but also the disruption of the vein valves and ligating or coiling of any venous branches, which finally guarantee maximal arterialisation of the distal aspects of the foot [6,7].
Typical indications for DVA are Rutherford classes 5 and 6 disease at high risk of amputation based on the Society for Vascular Surgery’s WIfI classification, unavailablility of surgical or endovascular treatment options and ineffective conservative treatment of CLI.
Although open surgical DVA has been performed for decades, there were recently published very good amputation-free survival midterm results from studies of percutaneous DSA using the LimFlow device for the “desert foot” [8,9].
The use of the DVA technique for no-option foot salvage in patients with CLI would allow for at least temporary to avoid a possible limb amputation and to improve quality of life.
Conclusion
Femorodistal revascularisation in combination with deep venous arterialization may be used as a therapeutic option to enhance the healing of ischemic ulcers and limb salvageability in patients with critical limb ischemia due to unreconstructable distal arteries and occluded pedal arches.
REFERENCES
- Uccioli L, Meloni M, Izzo V, et al. Critical limb ischemia: current challenges and future prospects. Vasc Health Risk Manag. 2018; 14:63–74.
- Migliara B. Treatment of No-Option CLI Patients. J Vasc Endovasc Ther rapy.2018;3(15).
- Schreve MA, Vos CG, Vahl AC, et al. Venous Arterialisation for Salvage of Critically Ischaemic Limbs: A Systematic Review and Meta-Analysis. Eur J Vasc Endovasc Surg. 2017; 53(3):387-402.
- Del Giudice C, Van Den Heuvel D, Wille J, et al. Percutaneous deep venous arterialization for severe critical limb ischemia in patients with no option of revascularization: early experience from two European centers. Cardiovasc Intervent Radiol. 2018; 41100:1474-80.
- Gandini R, Merolla S, Scaggiante J, et al. Endovascular Distal Plantar Vein Arterialization in Dialysis Patients with No-Option Critical Limb Ischemia and Posterior Tibial Artery Occlusion: A Technique for Limb Salvage in a Challenging Patient Subset. J Endovasc Ther. 2018; 25(1):127–32.
- Ho VT, Gologorsky R, Kibrik P, et al. Open, percutaneous, and hybrid deep venous arterialization technique for no-option foot salvage. J Vasc Surg. 2020; 71(6):2152-60.
- Ferraresi R., Casini A., Losurdo F, et al. Hybrid foot vein arterialization in no-option patients with critical limb ischemia: a preliminary report. J Endovasc Ther. 2018; 26: 7-17.
- Kum S, Huizing E, Schreve MA, et al. Percutaneous deep venous arterialization in patients with critical limb ischemia. J Cardiovasc Surg (Torino). 2018; 59(5): 665-9.
- Schmidt A, Schreve MA, Huizing E, et al. Midterm outcomes of percutaneous deep venous arterialization with a dedicated system for patients with no-option chronic limb-threatening ischemia: the ALPS multicenter study. J Endovasc Ther. 2020; 27(4):658–65.