Idiopathic granulomatous mastitis: a disease mimics breast cancer appearing in pregnancy
2 Department of General Surgery, Gulhane Education and Research Hospital, Ankara, Turkey, Email: %20drsdestek@yahoo.com
Received: 22-Jan-2018 Accepted Date: Jan 24, 2018; Published: 11-Feb-2018
Citation: Destek S, Gul OV. Idiopathic granulomatous mastitis: a disease mimics breast cancer appearing in pregnancy. Gen Surg: Open Access. 2018;1(1):7-10.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Idiopathic granulomatous mastitis: A Disease Mimics Breast Cancer Appearing In Pregnancy. Purpose: Idiopathic granulomatous mastitis (IGM) is a rare and chronic inflammatory disease. It is more common with autoimmune diseases, pregnancy and lactation periods, oral contraceptive (OKS) users and hyperprolactinemia cases. IGM mimics breast cancer regarding its clinical and radiological features. In this study, we present IGM cases which were diagnosed in pregnancy and mimics breast cancer. Cases: First case was 37 years old, suffering from hyperaemia, pain and swelling in the right breast applied our clinic on 18th week of pregnancy. Second patient was 24 years old, complaining with hyperaemia, pain, discharge and swelling in the left breast applied our clinic on 28th week of pregnancy. Heterogeneous, hypoechoic mass lesions with irregular margins that are similar findings observed in breast cancer were determined in both cases by breast ultrasonography. IGM was diagnosed by tru-cut biopsy for aiming differential diagnosis with breast cancer. Breast abscesses were drained and patients were treated with antibiotics and steroids. Conclusion: Pregnancy leads to some alterations on several systems in the body including immune system and hormonal system as well. Therefore, it is suggested that incidence of IGM is increased in pregnancy and lactation periods due to these systemical changes. As a result; IGM disease that clinically and radiologically is to mimic breast cancer should be diagnosed by breast biopsy and an appropriate treatment should be applied.
Introduction
IGM is a chronic inflammatory disease of the breast characterized by non-caseating granuloma, lobulitis and abscess formation. The etiology has not been fully elucidated. It mimics breast cancer with its clinical and radiological features [1]. It is more common with autoimmune diseases, pregnancy and lactation periods, oral contraceptive (OKS) users and hyperprolactinemia cases [2]. In this study, we present IGM cases which were diagnosed in pregnancy and had similar features with breast cancer.
Case Report
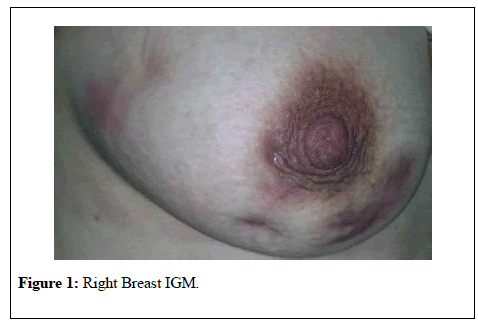
Case 1: Patient was 37 years old. When questioning family history, her aunt had a breast CA diagnosis. Gravidity was 6 and parity was 3. Due to Hashimoto's thyroiditis he had been using levothyroxine. She applied to our clinic with complaints of increased redness, pain and swelling in her right side at the 18th week of her pregnancy (Figure 1).
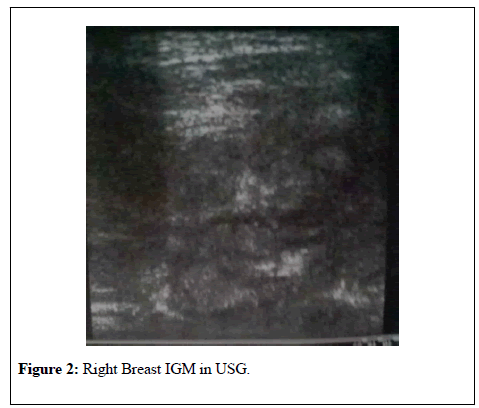
The right breast in breast ultrasound node revealed irregular heterogeneous hypoechoic mass lesions limited to solid ground which the biggest in 6 cm in diameter which are suspicious for malignancy and 18.4×9 hypoechoic lymph nodes at right axilla (Figure 2).
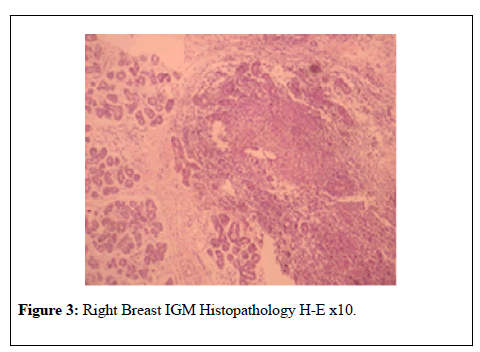
Serum leukocyte levels , C Reactive Protein (CRP) and Prolactin levels were high (12300 K/ul, 76.2 mg/l, Prolactin 95.5 ng/ml respectively). Rheumatoid Factor (RF), CA 125, Anti Nuclear Antibody (ANA), CA 15-3, Anti-Ds DNA Antibody (Anti ds DNA), Anti-Microsomal Antibody values were normal. True-cut breast biopsy was performed for differential diagnosis with breast cancer. IGM was diagnosed with histopathologic examination (Figure 3). Gram (+) cokes were detected with gram stain microscobic examination of apse taken from breast tissue. Cultures were positive for E. coli.
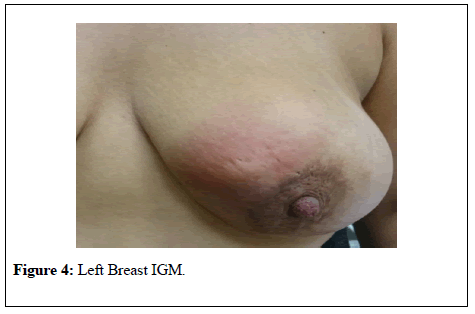
Case 2: Patient was 24 years old. There was no breast tumor history in her family. Gravidity and parity was 2. She applied to our clinic on the 28th week of gestation due to complains such as redness, pain, swelling on the breast of the left breast (Figure 4).
Breast ultrasound revealed a heterogeneous, hypoechoic irregularly limited mass lesions which the largest is diameter of 4.5 cm and a hypoechoic lymph node with a diameter of 20x8 mm in the left axilla (Figure 5).
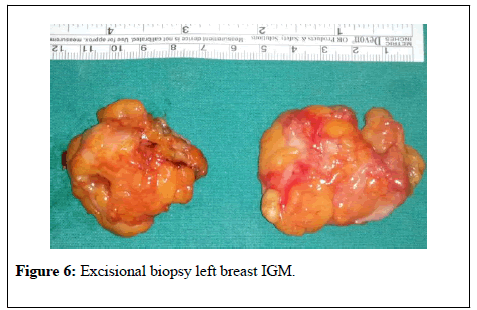
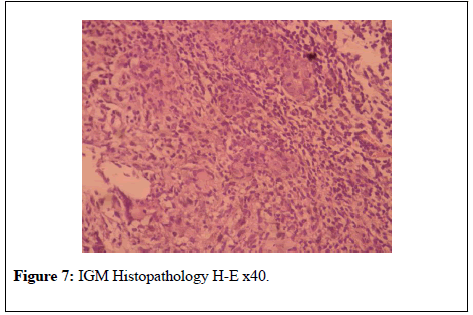
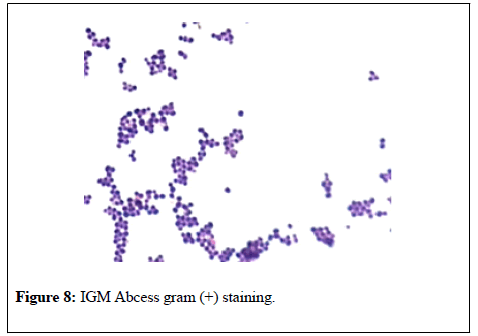
Serum leukocyte levels, C Reactive Protein (CRP) and Prolactin levels were high (13100 K/ul, 24.7 mg/l, Prolactin 114 ng/ml respectively).Serum RF, CA 125, CA 15-3, ANA, Anti ds DNA values were normal. For the purpose of differential diagnosis with breast cancer, excisional breast biopsy was performed on massive lesions (Figure 6). IGM was diagnosed with histopathologic examination (Figure 7). Gram (+) cokes were detected in gram spread of apse taken from breast tissue (Figure 8). There was no reproduction in the abscess culture.
Figure 6: Excisional biopsy left breast IGM.
The breast abscess was drained. Steroids were given for two months (Prednol 4 mg/day/oral and 0.1% betamethasone pomade topically) and wide spectrum antibiotics (cefuroxime axetil 500 mg tablets 2×1) were given during treatment for fifteen days. Short-term antibiotic intake was inadequate. As redness, pain and abscess increase in IGM area; given antibiotics.
After two months of treatment, there was no improvement. In the tests performed, serum prolactin levels were higher in both patients. Literature studies have reported that prolactin elevation is effective in the etiology of ICM. For this reason, prolactin inhibitor treatment was planned in consultation with the gynecology clinic. Prolactin inhibitor Cabergoline tablets were added to steroid treatments of patients. Patients were given Cabergoline tablet 2 mg / week / oral for 2 months on average. When the prolactin values of the patients were normalized, the IGM clinic improved. Hemogram and CRP levels were normal after treatment. A total of four months of treatment was discontinued. However, after the birth of the patients, there was a short lactation period of 3 months. No recurrence occured in four year's follow-up.
Discussion
The term Granulomatous Mastitis (GM) was first used by Kessler and Wolloch in 1972; and also made the definition of IGM for the first time [1,2]. GMs are classified as idiopathic (primary) and specific (secondary) [2,3].Specific GMs occur with various infectious agents such as sarcoidosis, foreign body reaction, cornea bacterium, tuberculosis, actinomycosis, blastomycosis, flaryazis [2,3]. GMs are different from IGMs, regarding as containing histopathologically caseation necrosis and common granulomas [2,3].
Less than 1 % of all women underwent biopsy for breast diseases are diagnosed with IGM [1]. It is also called idiopathic granulomatous lobular mastitis or idiopathic granulomatous lobulitis. It is more frequent between 2-4 decades in reproductive ages and in the first 6 years after childbirth [3,4]. It can also rarely be seen in men [3].
The etiology of the IGM is not fully understood. Hormonal disorders, autoimmunity, race, smoking, infectious factors, α1-antitripsin deficiency, diabetes mellitus, breast trauma, obesity are blamed factors on its etiology [3,4]. In the meantime, it has been reported that some pathologic gene polymorphisms may be effective in the etiology of lCM [4]. The IGM is most prevalent in the Mediterranean Region and developing countries in Asia [3].
Especially in non-gestational and non-lactational cases, the etiology is explained by autoimmunity [1-4]. The effectiveness of steroids in the treatment of IGM supports autoimmunity role in the disease pathology [3,4].
IGM may be seen alone or in combination with autoimmune diseases such as Weber-Christian disease Sjogren's syndrome, erythema nodosum, arthritis and thyroiditis [2,3]. It has been reported that breast secretions, centrilobular granulomatous formation, T-lymphocyte-cell-mediated autoantibodies to lobular epithelial cells play role in pathogenesis of IGM [3,4]. Since vasculitis and significant plasma cell infiltration are not present and autoimmune serologic tests such as RF and ANA results are negative, autoimmunity is still controversary [3,4]. In the first case of our study, there was Hashimoto Thyroiditis with IGM.
In various studies, the relationship between IGM and pregnancy or lactation is 90-100% [2,5]. A close association has also been reported between IGM and OKS use or hyperprolactinemia [3,5]. It has been also reported that Prolactin levels are important in recurrent cases [6]. Hyperprolactinemia is seen mostly due to drugs that increase prolactin levels and microprolactinomas [6]. These conditions have signed that hormonal irregularity is effective in etiology [2-4]. It has been reported that IGM may develop with hormonal effects such as estrogen and prolactin increase leading to intraductal protein secretion, ductal ectasia, intraductal inflammation [4-6].
İncreasing in the incidence of IGM in pregnancy and puerperium are caused by hormonal imbalance and immunological changes in the mother's body [5]. The most effective hormones in the pathogenesis of IGM in pregnancy are estrogen and prolactin [7]. In addition, we assume that hormones such as human chorionic gonadotropin which increases estrogen release, human chorionic growth hormone acting on ducts in mother's womb and human placental lactogen are effective in the formation of IGM by hormonal and immunologically ways [5-7]. Prolactin levels were high in our patients as well. The use of prolactin inhibitors in these patients has been reported to increase success in the treatment of IGM.
IGM usually seen with painful, fast growing breast mass, redness and fistula [1,2]. Abscesses may develop with findings of infection [2]. Sometimes it mimics cancer with breast withdrawal and peau d'orange appearance [2]. 50% of cases are confused with cancer. It has been reported that 13% of patients have axillary palpable lymphadenomegaly [3]. The incidence of both breasts is equal. Involvement is often unilateral [4]. Bilateral incidence rate is 25% [1].
Breast ultrasound reveals hypoechoic tubular structures and nodules while mammography reveals focal asymmetry and nodular opacity [1]. Imaging features may mimic inflammatory breast cancer [1,3]. Magnetic resonance findings are nonspecific [1]. Ultrasonography, mammography and magnetic resonance imaging have no pathognomonic sign [1,3].
The diagnosis of IGM is based on the exclusion of other specific granulomatous lesions such as tuberculosis, sarcoidosis, wegener granulomatosis and fungal infections. Besides, it should come to mind nonpuerperal mastitis, cancers and breast abscess in differential diagnosis [2,3]. The diagnosis is made by histopathological examination [1,6]. Cytologic fine needle examination is generally inadequate. Usually, core biopsy or excisional biopsy with ultrasonography is used for definite diagnosis [1,8]. Non-caseified granulomas in lobular regions, giant cells, chronic inflammation, microabcesses and fatty necrosis may seen in hystopathologically [3]. We performed breast-true-cut biopsy in a case and excisional breast biopsy in another.
If there is no secondary infection in the abscess culture, usually there is no reproduction [2,3]. In the presence of secondary infection, the most common pathogens are coagulase-negative streptococuses, propiniobacteriums and corynebacterium bacterias. Ziehl-Neelsen for tuberculosis and PAS staining for fungus should performed as well as Gram staining and cultures [2,3]. E. coli was positive in cultures in one of our patients. Before treatment, malignancy and specific causes of GM should be excluded primarily [2]. There is no common form of treatment has been generally accepted in the IGM treatment [3]. So that, general approach is conservative treatment [2]. In case there is an abscess, it must be drained primarily. Immunosuppressives such as steroids, antiinflamatuaries such as colchicine, methotrexate and azothiopurine are used for conservative treatment [9]. If hyperprolactinemia is present, prolactin antagonists are used and appropriate antibiotics are used if culture results are positive. [4,6]. Steroid therapy is recommended especially for complicated and recurrent cases with abscess or fistulas [9]. Before steroid treatment, it should be ruled out that there is no infection elsewhere in the body, especially tuberculosis should be excluded [9]. Complete response rates with steroids are 42-93%, partial response 6-58% and unresponsiveness is 6.5% [9,10].
Surgical treatment is carried out in the presence of clinical signs such as non-response to medical therapy and recurrent abscesses or fistulas. As a surgical treatment; drainage, limited or extensive surgical excision and mastectomy may be applied. The most common surgical treatment is extensive surgical excision. Negative limits should be deducted. Excisional structures may have 5-50% recurrence, 30% fistula or abscess development [9,11]. It should aim to limit negative interference. Excision applied of 5-50% patients may develop recurrences and 30% cases may seen with an abscess or fistula complications [8,9].
Surgery and steroid treatment may also be used together. Primarily; low dose steroid treatment for reducing lesion size and after that surgical excision may be used for chosen cases. In some reports; steroid treatment after surgical excision applications are suggested for attaining much lower recurrence rates [9,10].
Abscess drainage was applied in one case and local excision in the other. Subsequently for medical treatment systemic steroid treatment (Prednol 4 mg/day) for four weeks and topical (0.1% betamethasone pomate topically) and Cefuroxime Axetil 500 mg tablet 2x1 were given. Since the steroid was not able to get a complete response and the levels of prolactin were high, the treated Cabergoline tablets were added. It was stated that the use of prolactin inhibitor was effective in the treatment of IGM in various studies. Patients were treated with steroids for two months and steroids and prolactin inhibitors for two months. Therapeutic responses were obtained and the patients' clinic improved. We did not have a gestational problem related to the use of a prolactin inhibitor. However, our patients had a short postpartum period.
Regular follow-up is recommended with 3-6 months periods [10]. Recurrence rate is reported as 16-50% in two years [11]. Our cases did not develop recurrence in 4 year follow-up period.
Conclusion
It is thought that IGM is a disease due to autoimmunity, hormonal disorders. It may mimic breast carcinoma with its clinical and radiological features. Diagnosis must be confirmed by biopsy. During pregnancy, both the immunity and the hormonal system change in the body. During this period, the prolactin hormone rises. Therefore, IGM is more prevalent in pregnancy and lactation period. Consequently, prolactin inhibitors may be an effective option for medical therapy in the treatment of IGM during the pregnancy period when steroids can not be used for long periods and high doses. On the other hand, more comprehensive research is required.
REFERENCES
- Hovanessian LJ, Peyvandi B, Klipfel N, et al. Granulomatous lobular mastitis: imaging, diagnosis, and treatment. AJR Am J Roentgenol. 2009;193:574-81.
- Diesing D, Axt-Fliedner R, Hornung D, et al. Granulomatous mastitis. Arch Gynecol Obstet. 2004;269:233–6.
- Mathew M, Siwawa P, Misra S. Idiopathic granulomatous mastitis: an inflammatory breast condition with review of the literature. BMJ Case Rep. 2015.
- Destek S, Gul VO, Ahioglu S. A variety of gene polymorphisms associated with idiopathic granulomatous mastitis. J Surg Case Rep. 2016.
- Laas E, Touboul C, Kerdraon O, et al. Inflammatory and infectious breast mastitis outside of pregnancy and lactation: Guidelines. J Gynecol Obstet Biol Reprod. 2015;44:996-1016.
- Destek S, Gul VO, Ahioglu S, et al. Pituitary Adenoma and Hyperprolactinemia Accompanied by Idiopathic Granulomatous Mastitis. Case Rep Endocrinol.
- Garcia-Rodiguez JA, Pattullo A. Idiopathic granulomatous mastitis: a mimicking disease in a pregnant woman: a case report. BMC Res Notes. 2013;6:95.
- Yabanoglu H, Colakoglu T, Belli S, et al. A Comparative Study of Conservative versus Surgical Treatment Protocols for 77 Patients with Idiopathic Granulomatous Mastitis. Breast J. 2015;21:363-9.
- Sakurai K, Fujisaki S, Enomoto K, et al. Evaluation of follow-up strategies for corticosteroid therapy of idiopathic granulomatous mastitis. Surg Today 2011;41:333-7.
- Baslaim MM, Khayat HA, Al-Amoudi SA. Idiopathic granulomatous mastitis: a heterogeneous disease with variable clinical presentation. World J Surg. 2007;31:1677-81.
- Skandarajah A, Marley L. Idiopathic granulomatous mastitis: a medical or surgical disease of the breast? ANZ J Surg. 2015;85:979-82.