Idiopathic purulent pericarditis without underlying causes present with tamponade: A Rare case report.
2 The Bachelor of Science in Nursing, Congenital and Pediatric Cardiology Division, Pediatric Departme, Iran
3 Asistance Professor, Pediatric Interventional Cardiologist, Pediatric and Congenital Cardiology divi, Iran
4 Pediatric Cardiologist, Pediatric and Congenital Cardiology division, Pediatric Department, Faculty, Mashhad University of Medical Sciences, Mashhad – Iran Hospital, Iran, Email: Feisalrahimpoor@gmail.com
Received: 28-Sep-2022, Manuscript No. puljhr-22-5548; Editor assigned: 30-Sep-2022, Pre QC No. puljhr-22-5548 (PQ); Accepted Date: Oct 23, 2022; Reviewed: 13-Oct-2022 QC No. puljhr-22-5548 (Q); Revised: 20-Oct-2022, Manuscript No. puljhr-22-5548 (R); Published: 26-Oct-2022, DOI: 10.37532/ puljhr.2022.5(5).01-03
Citation: Maleki MH, Ghaznavi NSM, Birjandi H, et al. Idiopathic purulent pericarditis without underlying causes present with tamponade: A Rare case report. Int J. Heart Res. 2022; 5(5):1-3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Pericardial effusion is not a common finding in clinical practice. Sometimes, the pericardial effusion is a comorbidity of known underlying disease, such as end-stage renal disease, acute myocardial infarction, cardiac surgery or widespread metastatic neoplasm. When no reason is apparent, some clinical findings can be useful to establish a diagnosis. The presence of acute inflammatory signs is predictive for acute idiopathic pericarditis. Severe pericardial effusion with absence of inflammatory signs without evidence of tamponade is predictive for chronic idiopathic pericardial effusion, and tamponade without inflammatory signs for neoplastic pericardial effusion. We present a 4 years-old boy who developed tamponade and was successfully treated with surgical pericardial drainage and intravenous drugs.
Keywords
Pericarditis; Chest X-ray; ECG; Echocardiography; CT/MRI
INTRODUCTION
Purulent pericarditis is a rare disease that is most often caused by organisms such as Staphylococcus aureus, viridians streptococci, Streptococcus pneumonia, Hemophilic influenza, and anaerobic bacteria [1]. Pericarditis often presents with chest pain and dyspnea and symptoms that improve while sitting upright and worsen while lying flat. Other important point of history includes questions regarding recent illnesses, malignancy, history of tuberculosis and vaccination status, auto-immune disorders, history of chronic kidney disease or renal failure, or history of congestive heart failure, liver disease, and hypothyroidism. Occasionally, the pericardial effusion can be related to a known disorder, such as acute myocardial infarction, cardiac surgery, end-stage renal disease or widespread metastatic neoplasm. The presence of acute inflammatory signs is predictive of acute idiopathic pericarditis irrespective of the size of the effusion or the presence or absence of tamponade [2]. Severe pericardial effusion with an absence of inflammatory signs without evidence of tamponade is predictive for chronic idiopathic pericardial effusion, and tamponade without inflammatory signs for neoplastic pericardial effusion
Case Report
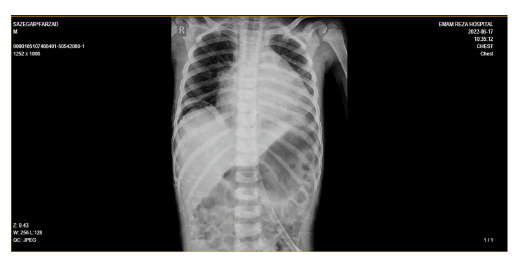
A 4 year-old child patient with fever, toothache, and edema in a right submandibular area referred to the clinic and treated with Amoxicillin, he had a temporary recovery and the symptoms was disappeared. After a few days the symptoms returned and cough and sore throat was added also. He was referred to the clinic again, the dose of Amoxicillin was raised and penicillin and a single dose of Betamethasone were added. The next day he had arthralgia and couldn’t walk. The patient refers to the Emergency Department of Sheikh Hospital of Mashhad University of Medical Sciences and hospitalized and meropenem and vancomycin was started.in the first lab tests these results were obtained (wbc=17000/mcl, Neut=84%, lymph=16%),(plt=129000/ mcl),(Na=127 mEq/L),(Ca=8.5 mg/dl),(C RP=120 mg/l). During hospitalization Edema in the lower limbs was appeared and coughing continues. For further investigation, CX-Ray was performed and cardiomegaly was observed (Figure 1).
Electrocardiogram (ECG) data suggested Generalized St-t changes (Figure 2). The patient was transferred to the Pediatric Cardiology Department of Imam Reza Hospital of Mashhad University of Medical Sciences to continue treatment with a possible diagnosis of pericarditis. In the initial examination, lymphadenopathy was disappeared but erythema in the pharynx was seen. Lung auscultation was clear and breath movement was normal. The abdomen was soft and without distention and there was no organomegaly. Pitting Edema in the lower limbs was also revealed. Passive movement of the right hip was decreased and he still couldn’t walk well. Abdomen, pelvic and hip sonography was normal and there was no effusion in the hip. Infectious consultation was done and meropenem changes to ceftriaxone (75 mg/kg/day). The patient was isolated with a possible defect in the immune system. The lab tests were disturbed (WBC=15000/mcl, Neut=68%, lymph=20%), (Hb=9.5 g/ dl), (Plt=258000/ml), (ESR=24mm/h), (CRP=65mg/l), (Total protein=5.4 g/dl), (Alb=3.1 g/dl). With doubt of diffuse staphylococcus infection, the bone scan was performed and hip, knee and right tibia osteomyelitis was observed. The patient suffered LOC due to hyponatremia, the electrolyte disorder was corrected and brain MRI was Normal. echocardiography was also done and showed severe pericardial effusion(24 mm) with fibrin appearance and RA collapse was revealed, but in cardiac monitoring evidence of tamponade was not seen (Figure 3)
Figure 3: Echocardiography in Standard 4 Chamber and Para sternal short axis showed massive purulent pericarditis
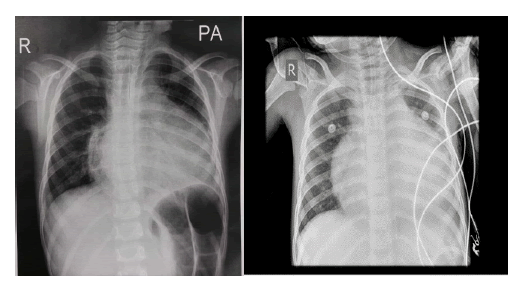
Cardiac surgery consultation was done and patient was a candidate for Pericardiocentesis and was transferred to the PICU (Figure 4).
After pericardiocentesis, a sample of pericardial and plural fluid and pleural biopsy was send to laboratory and the following findings were obtained, acute purulent pleuritic and no neoplastic lesion-Pericardial fluid cell count: (WBC=80000/mm, RBC=3100/mm, Polynuclear=8 0%, Mononuclear=20%), (sugar=16 mg/dl), (Protein=3800 mg/dl), (LDH=12197 U/L), (Albumin=2600 mg/dl)-Pleural fluid cell count: (WBC=1170/mm, RBC=920/mm, Polynuclear=30%, Mononuclear= 70%), (sugar=98 mg/dl), (Protein=2000 mg/dl),(LDH=301 U/L),(Alb umin=1400 mg/dl), Pleural and pericardial fluids cultures was also negative. The lab tests were done again. (WBC=26000/mcl, neut=82%, lymph=8.5%), (Hb=10 g/dl), (plt=365000/ml), (ESR=66 mm/h), (CRP=39.7mg/l), (Alb=2.6g/dl), (AST=22U/L), (ALT=60 U / L), (LDH=536 U/L), (RF-), (ASO titr-), (2ME-), (WRIGHT-), (ANA=0.1) Treatment continued with ceftriaxone and vancomycin for about 28 days and after 4 weeks from the onset of disease lab tests decreased(CRP=14.2), (ESR=17). Echocardiography showed no significant pericardial effusion, the patient was discharged with stable hemodynamic and vital signs.
Discussion
About 37% to68% of children that was admitted for pericardial effusions or acute pericarditis has Idiopathic pericarditis [1]. The idiopathic form of pericarditis is the most in developed country, and the search for an infectious etiology isalmost negative. Patients with acute inflammatory signs should receive aspirin or non-steroid antiinflammatory drugs. In the setting of acute inflammatory pericarditis, steroids should not be used as they raise the possibility of relapses. Colchicine is an established indication in patients with recurrent pericarditis, and has also been suggested to be useful in the first episode of acute pericarditis to avoid the appearance of relapses. The patients with acute viral or idiopathic pericarditis should be managed on the hospital if they have clinical predictors of poor prognosis (cardiac tamponade, severe pericardial effusion, immunosuppression, oral anticoagulant therapy or fever gt; 38°C [2]. Pericardial drainage and antibiotic therapy are essential in management of children with purulent effusions. Several surgical drainage approach have been reported, including subxiphoid tube drainage, placement of a pericardial window with pleural drainage, partial pericardiectomy with pericardial drainage, total pericardiectomy, and infusion of streptokinase into the pericardial space[1,3]. Selection of the surgical approach depends on many factors, including the etiology of the pericarditis, the consistency of the pericardial fluid, the patient's progress after initial management, and the experience of the medical center itself. After pericardiocentesis is performed, the fluid should be sent for test [3]. Aspiration of Pericardial effusion can help relieve symptoms and hemodynamic compromise in most patients, those occurring after a malignancy may require a pericardial window that can be done. The prognosis of pericardial effusion depends on the etiology, being especially poor in patients with neoplastic pericardial effusion secondary to lung cancer. Prognosis is very good in idiopathic/viral pericarditis; Patients with structurally normal hearts have excellent outcomes after operation [4]. In patients with tuberculous or purulent pericarditis the prognosis depends on the precocity of the diagnosis and adequate treatment, but purulent pericarditis frequently occurs in patients with underlying disease (diabetes mellitus, liver cirrhosis, widespread infections) [5-7].
Conclusion
Purulent pericarditis frequently occurs in patients with underlying disease but it may happen in the patient without underlying factors in these cases the prognosis depends on the precocity of the diagnosis and adequate treatment.
References
- Ö. Çakir, F. Gurkan, A. E. Balci, et al. “Purulent pericarditis in childhood: Ten years of experience,” Journal of Pediatric Surgery. 2002; 37(10): 1404–8.
- Colombo A, Olson HG, Egan J, et al. Etiology and prognostic implications of a large pericardial effusion in men. Clin Cardiol. 1988; 11:389–94.
- Kuhn B, Peters J, Marx GR, et al. Etiology, management, and outcome of pediatric pericardial effusions. Pediatr Cardiol. 2008; 29:90–4.
- Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004; 43:1042–46.
- Troughton RW, Asher CR, Klein AL, et al. Pericarditis. The Lancet. 2004; 363(9410):717-27.
- Roodpeyma S, Sadeghian N. Acute pericarditis in childhood: a 10-year experience. Pediatr Cardiol 2000; 21:363–7
[Google scholar] [Cross Ref].
- Bhaduri-McIntosh, S., Prasad, M., Moltedo, J. et al. Purulent pericarditis caused by group A streptococcus. Texas Heart Institute Journal, 33,519-22.(2006)




-g002.png)