Immunotherapy: Revolutionizing cancer treatment through immune modulation
Received: 15-Dec-2023, Manuscript No. puljmc-24-7150; Editor assigned: 17-Dec-2023, Pre QC No. puljmc-24-7150; Accepted Date: Jan 20, 2024; Reviewed: 05-Jan-2024 QC No. puljmc-24-7150; Revised: 12-Jan-2024, Manuscript No. puljmc-24-7150; Published: 22-Jan-2024
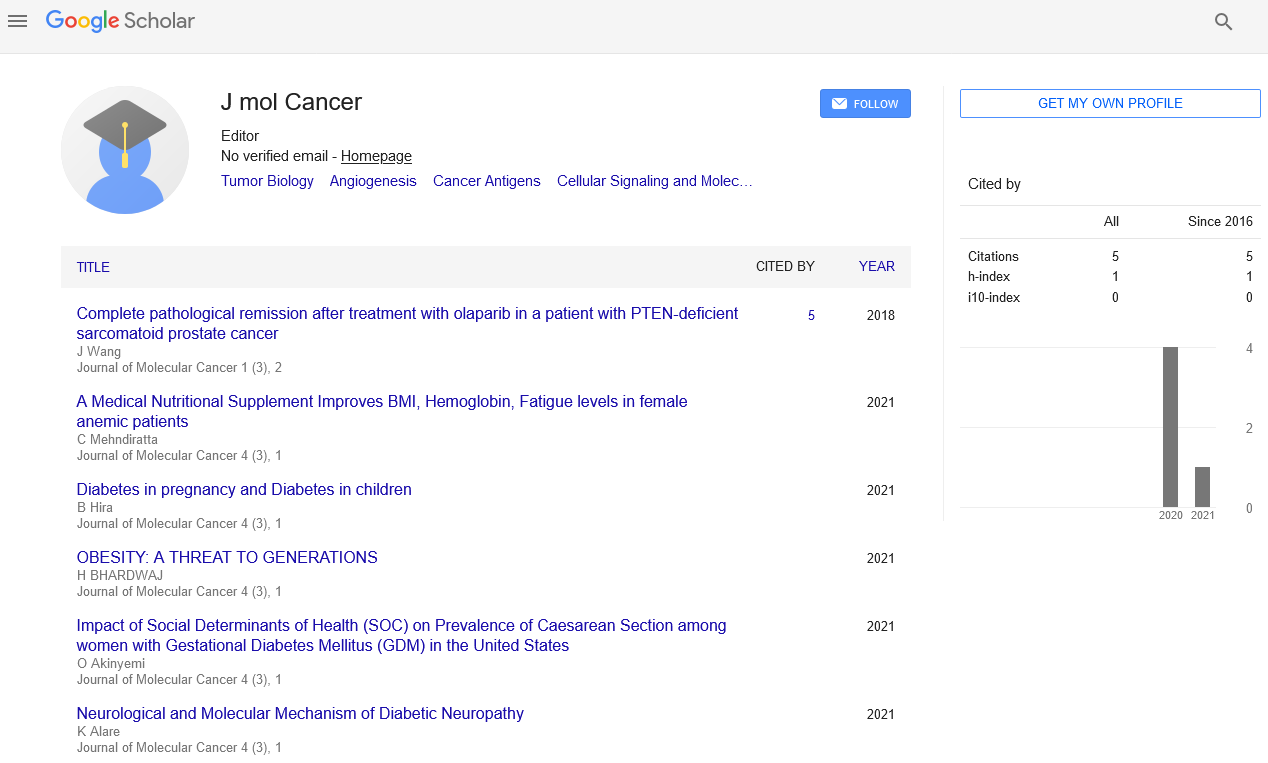
Citation: Wang W. Immunotherapy: Revolutionizing cancer treatment through immune modulation. J Mol Cancer. 2024; 6(1):1-2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Immunotherapy has emerged as a transformative approach in cancer treatment, harnessing the body's immune system to target and eliminate cancer cells. This article provides a comprehensive overview of immunotherapy, including its mechanisms, types, and impact on cancer treatment. We explore key innovations such as checkpoint inhibitors, CAR-T cell therapy, and cancer vaccines, highlighting their successes and ongoing challenges. The article also examines the current landscape of immunotherapy research, recent advancements, and future directions. By understanding the principles and progress in immunotherapy, we can appreciate its potential to reshape cancer treatment and improve patient outcomes.
Key Words
Immunotherapy; Cancer treatment; Checkpoint inhibitors; CAR T Cell therapy; Cancer vaccines; Immune modulation; Tumor microenvironment
Introduction
Cancer remains one of the leading causes of death worldwide, driven by complex interactions between genetic mutations, cellular processes, and the immune system. Traditional treatments, including surgery, radiation, and chemotherapy, have achieved significant advancements in cancer management but are often limited by issues such as resistance, toxicity, and limited efficacy in certain cancers. In recent years, immunotherapy has emerged as a revolutionary approach, offering new hope by harnessing the power of the immune system to fight cancer.
Immunotherapy leverages the body’s natural defense mechanisms to specifically target and destroy cancer cells while sparing normal cells. This approach has shown remarkable success in treating various cancers and has significantly expanded the therapeutic options available to patients. This article aims to provide an in-depth understanding of immunotherapy, exploring its mechanisms, different types, and the current state of research and clinical application.
Mechanisms of immunotherapy
Immunotherapy works by enhancing or manipulating the immune system to recognize and attack cancer cells. The primary mechanisms through which immunotherapy exerts its effects include:
Checkpoint inhibitors are a class of immunotherapy drugs designed to block immune checkpoints—molecules that normally inhibit immune responses to prevent autoimmunity. Cancer cells often exploit these checkpoints to evade immune detection. By inhibiting checkpoint molecules, these therapies restore the immune system's ability to recognize and attack cancer cells.
Chimeric Antigen Receptor T-cell (CAR-T) therapy involves engineering a patient’s T cells to express a receptor specific to cancer antigens. This process enables the T cells to recognize and kill cancer cells more effectively.
CAR-T cells are created by extracting T cells from a patient’s blood, modifying them in the laboratory to express a CAR specific to a tumor-associated antigen (e.g., CD19 in B-cell lymphomas), and then infusing the engineered cells back into the patient. This approach has shown dramatic success in treating hematologic malignancies such as Acute Lymphoblastic Leukemia (ALL) and large B-cell lymphoma.
Despite its success, CAR-T cell therapy faces challenges such as Cytokine Release Syndrome (CRS), neurotoxicity, and limited efficacy in solid tumors. Ongoing research aims to address these issues and enhance the therapy's effectiveness. Cancer vaccines aim to stimulate the immune system to recognize and attack cancer cells by introducing specific tumor-associated antigens. There are two main types of cancer vaccines:
These vaccines are designed to treat existing cancer by boosting the immune response against tumor-specific antigens. Examples include the prostate cancer vaccine Sipuleucel-T and the melanoma vaccine Ipilimumab. Therapeutic vaccines can enhance the immune system’s ability to target and destroy cancer cells. Preventive vaccines are designed to prevent cancer development by inducing immunity against cancer-causing pathogens. The most notable example is the Human Papillomavirus (HPV) vaccine, which reduces the risk of cervical and other HPV-related cancers. Monoclonal Antibodies (mAbs) are laboratory-made molecules designed to bind specifically to cancer cell antigens. They can work through various mechanisms, including:
Monoclonal antibodies can directly bind to tumor antigens and inhibit cancer cell growth. For example, trastuzumab targets HER2 in breast cancer. Some monoclonal antibodies can recruit immune cells to attack cancer cells. For instance, antibodies such as rituximab can engage immune effector cells to destroy B-cell lymphomas. Oncolytic virus therapy involves using genetically modified viruses that selectively infect and kill cancer cells. These viruses can also stimulate an immune response against the tumor.
Impact of immunotherapy on cancer treatment
Immunotherapy has significantly impacted cancer treatment by providing new options for patients who may not have responded to traditional therapies:
Immunotherapy has shown remarkable efficacy in cancers previously considered difficult to treat. For example, checkpoint inhibitors have provided durable responses in melanoma and non-small cell lung cancer, while CAR-T cell therapy has transformed the treatment landscape for certain hematologic malignancies. Immunotherapy offers the potential for personalized treatment based on the specific genetic and molecular characteristics of a patient’s tumor. This approach allows for more precise targeting and tailored therapies, improving treatment outcomes and minimizing side effects.
Current challenges and future directions
Despite its successes, immunotherapy faces several challenges that require ongoing research and development:
Not all patients or cancers respond to immunotherapy. Understanding the factors that influence response, such as tumor microenvironment and genetic mutations, is critical for improving efficacy and expanding the range of treatable cancers. Immunotherapy can lead to immune-related adverse events, including autoimmune reactions and inflammation. Managing these side effects and developing strategies to mitigate toxicity are important for optimizing patient safety and treatment outcomes.
Conclusion
Immunotherapy represents a ground breaking advancement in cancer treatment, leveraging the body’s immune system to target and destroy cancer cells. Through mechanisms such as checkpoint inhibition, CAR-T cell therapy, cancer vaccines, and monoclonal antibodies, immunotherapy has demonstrated remarkable efficacy in treating various cancers and has transformed the therapeutic landscape.
As research continues to advance, addressing the challenges associated with immunotherapy and exploring new approaches will be crucial for maximizing its potential and improving patient outcomes. By harnessing the power of the immune system, immunotherapy has the potential to revolutionize cancer treatment and provide new hope for patients worldwide. The ongoing exploration of immunotherapy and its integration with other treatment modalities will shape the future of oncology and offer promising prospects for the fight against cancer.