Implementation of a shared plan of care: A pilot approach to care coordination with children with neurodevelopmental disabilities
2 Riley Hospital for Children at Indiana University Health, Riley Child Development Center, Indiana University School of Medicine, Indianapolis, Indiana, USA, Email: mcnallyr@iu.edu
3 Developmental Pediatrics, Riley Hospital for Children, Indiana University School of Medicine, Indianapolis, Indiana, USA, Email: tlock@verizon.net
Received: 07-Feb-2018 Accepted Date: Apr 20, 2018; Published: 27-Feb-2018
Citation: McAllister JW, Keehn RM, Rodgers R, et al. Implementation of a shared plan of care: A pilot approach to care coordination with children with neurodevelopmental disabilities. J Nurs Res Pract. 2018;2(2):01-05.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Care Coordination is highlighted as a beneficial cross-cutting healthcare improvement, and plans of care a promising strategy. However, little empirical work addresses these theoretical ideals, particularly in pediatrics. This paper describes a care coordination innovation using a family-centered, goal-directed approach.
Keywords
Children and youth with special health care needs; Neurodevelopmental disabilities; Family-centered care; Care coordination; Shared plan of care; Planned-care; Care neighborhood; Co-production
Introduction
Children and youth with special health care needs (CYSHCN) are defined as those who have one or more chronic physical, developmental, behavioral, or emotional condition requiring health and related services beyond that required by children generally [1]. Families caring for CYSHCN report many unmet, challenging medical and non-medical needs [2,3], unmet needs are often further complicated by social determinants of health factors [4].
Children with neurodevelopmental disabilities, a subpopulation of CYSHCN, have complex, lifelong disorders affecting their physical, cognitive, social, and behavioral development [5,6]. Pediatric clinicians are challenged to care for this population as care requires significant knowledge, time, and resources [7,8]. Additionally, children and their families often live in communities ill-equipped to help them navigate complex healthcare, education and financing systems [5,6].
Families increasingly report that they need, but do not have, adequate care coordination [2]. Care coordination, implemented as a patient and family centered, assessment driven, continuous, team-based activity designed to meet bio-psychosocial needs while enhancing family and professional care giving skills [9], can lead to better pediatric care, family and professional experience of care, and population health [10,11]. The literature highlights the plan of care as important to the care coordination process, but suggests that variations in practice makes evaluation challenging [12,13]. Current care coordination initiatives often lack consistent adherence to recommended standards [14,15]. Families are frequently uncertain about what care coordination means and whether they have authentic care coordination. To address these concerns, an expert panel, funded by the Lucile Packard Foundation for Children’s Health, published guidelines for an approach to care coordination using a Shared Plan of Care (SPoC) [16]. These guidelines include underlying principles and action steps [17]. However, little empirical work has been reported on “real-life” implementation of these theoretical ideals, particularly with a population having complex medical and psychosocial needs.
The Riley Hospital for Children at Indiana University Health is a 280- bed, specialty children’s hospital located in downtown Indianapolis, Indiana. It serves as the tertiary and quaternary care resource for both the metropolitan region and the state at large, evaluating and treating high numbers of children with complex medical conditions. The Riley Care Coordination Program (RCCP) was developed to work proactively with families to address unmet needs and eliminate barriers to understanding and accessing needed interventions and services for a population of children with neurodevelopmental disabilities. RCCP piloted the application of a SPoC-based care coordination model with this population. This paper will: 1) describe implementation of this approach to care coordination within the context of a children’s specialty hospital ambulatory care setting, and 2) outline successes, challenges and lessons learned.
Methods
Care coordination model and implementation team
RCCP’s first task was adapting the “Achieving a Shared Plan of Care” model17 to the local context. An interdisciplinary team was formed that included a family leader, care coordination expert, three subspecialty clinicians (developmental pediatrician, Med/Peds physician, and clinical psychologist), three care coordinators (family advocate, registered nurse, and clinical social worker), and administrative support. Establishing a prepared, proactive team required skill development, effective care processes, and supportive tools [18], Principles of relational coordination were applied to foster team cohesion including shared goals, frequent communication, and generation of new knowledge [19].
The population selected to test the care coordination model were children ages 2-10 with a diagnosis of autism, developmental delay, and/or intellectual disability cared for by neurodevelopmental subspecialists at Riley Hospital for Children. Divisions eligible to refer included child development, developmental pediatrics, child psychiatry, neurology, and genetics. RCCP leaders presented to each division to facilitate recruitment; explained the program and eligibility criteria, distributed referral forms and brochures, and requested collaboration. Subspecialists in these sections identified families for referral based upon clinical assessment of need and family interest.
During an 18-month pilot period team roles were detailed, care processes/ functions tested, tools enhanced, and outcome measures applied. Participants engaged in a Table 1.
| Participants (N=263) | |
|---|---|
| Age [years; M (SD)] | 4.5 (1.9) |
| Sex | |
| Male Female |
205 (78%) 58 (22%) |
| Race | |
| Caucasian Black/African American Asian/Pacific Islander Multi-racial Not reported |
207 (79%) 40 (15%) 10 (4%) 3 (1%) 3 (1%) |
| Ethnicity | |
| Non-Hispanic Hispanic |
241 (92%) 22 (8%) |
| Primary Language | |
| English Spanish Burmese |
242 (92%) 16 (6%) 5 (2%) |
| Diagnosis | |
| ASD DD/ID |
154 (59%) 105 (40%) |
| Referral Source | |
| Child Development Developmental Pediatrics Other Child Psychiatry Neurology Genetics |
125 (48%) 83 (32%) 29 (10%) 20 (8%) 5 (2%) 1 (<1%) |
| Subspecialty Providers* | |
| 1-3 4-5 > 5 |
119 (45%) 59 (22%) 47 (18%) |
| Insurance | |
| Public Private |
187 (71%) 72 (27%) |
Table 1: Demographic characteristics of enrolled participants
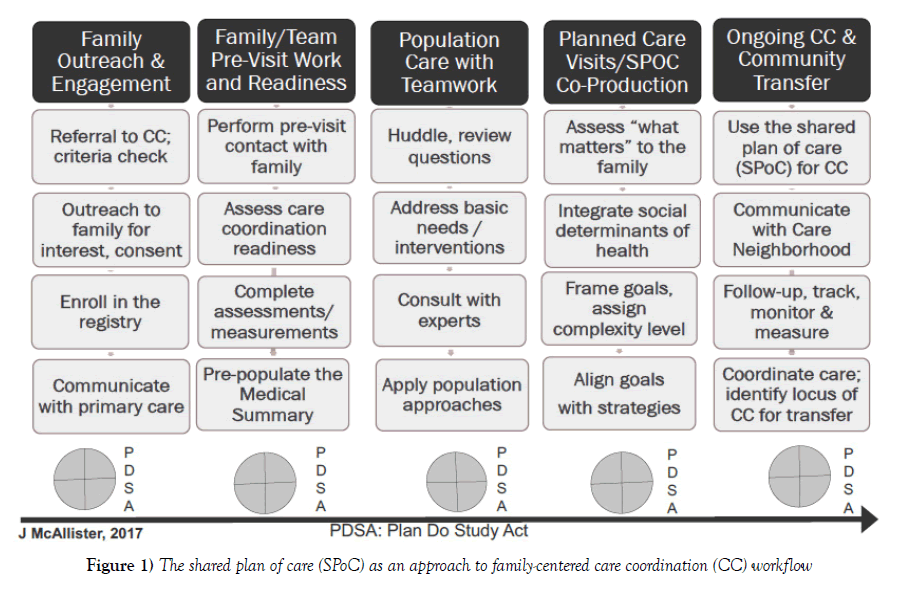
“Planned-care visit”, SPoC co-production, and 6-months of care coordination. RCCP activities included five workflow phases (Figure 1).
Phase 1) Family outreach/engagement
Following family enrollment, a “planned-care visit” was scheduled and referring subspecialist and primary care providers were notified. Coordinators briefed these “Care Neighborhood” [20], partners and invited their input. Families were mailed a visit confirmation, program brochure, pre-visit assessment tool, and a SPoC example.
Phase 2) Family and team pre-visit work
Care coordinators initiated phone/e-mail/mail contact to learn about each family, help with expectations, and address participation challenges and questions. Coordinators collaborated with the larger team to troubleshoot access barriers and ensure visit success (e.g. addressing transportation, insurance, interpretation, and cultural considerations as needed). The team prepared for visits by reviewing medical records and reports and using these data to pre-populate the SPoC’s Medical Summary characterizing child/ family strengths, challenges, diagnoses, interventions, and relevant medical and educational providers.
Phase 3) Population-based teamwork
The RCCP team held weekly meetings to prepare for family visits, review family priorities and coordination activities, provide clinical supervision/ oversight, and learn from one-another. Full-team and subgroup gatherings, clinician/coordinator huddles, and/or broader care conferences fostered teamwork and cohesion. Analysis of plan-do-study-act improvement cycles allowed for review of care coordination processes (e.g. communication strategies, referrals, SPoC template updates, and follow-up activities); these activities contributed to RCCP’s learning organization/laboratory approach [21].
Phase 4) Planned-Care Visit/ SPOC “Co-Production”
Children/families participated with a coordinator/clinician dyad in a 90-minute, face-to-face, “planned-care visit” within a child development clinical setting. The visit had three components: 1) time for families to express “what matters” and for clinician/care coordinators to listen and make observations, 2) reflection of family priorities and pertinent clinical concerns framed as short and long-term goals, and 3) prioritization of 3-4 elicited goals with strategic next steps. A drafted SPoC “Negotiated Actions” (goals with aligned strategies and responsibilities) went home with the family; a completed SPoC was sent to families, referring subspecialists, and primary care providers within 2-4 weeks. Agreement between family and team on who may be involved in information exchanges throughout the coordination period was documented.
Phase 5) Ongoing Care Coordination and Community Transfer
The child/family and team used the SPoC to guide their care coordination activities for up-to six months. Follow-up contacts between families and their coordinator occurred primarily by telephone and email/mail. The SPoC was made available to all identified care neighborhood partners (e.g. specialists, primary care, and school and community professionals). Transfer of care coordination back to community providers occurred when families “exited” RCCP. Primary care was explicitly asked to help address any outstanding and ongoing need. If they were unable/unwilling to assume this coordinating role, the team worked to identify alternative supports.
Evaluation
Following Indiana University guidelines and IRB approval, a confidential, HIPPA compliant electronic-portal was used to create a participant registry and input data from SPoCs, multiple related medical records, coordinator logs, child/family complexity scores, and pre-post family survey results. Data informed real-time quality improvement efforts including referral issues, primary care communications, and redundant or conflicting recommendations. Financial data included clinical charges/payments and non-reimbursable care plan oversight claims.
Results
As with most pilot programs, the RCCP experience included significant successes, challenges and lessons learned. Each stakeholder group (children/ families; clinicians/coordinators; and specialists/primary care providers) reported different but overlapping observations, summarized below.
Children and families
Caregivers in this cohort included a diverse array of parents, grandparents, aunts/uncles, siblings, cousins, and friends, yet all expressed strikingly similar goals. Prior to the RCCP, these children and families did not have access to explicit care coordination services. As a result of the RCCP, family goals were documented within a SPoC which led to family-centered solutions. A common family goal was to meet their children’s needs. “How can we help our child to be their best” was a frequent question, yet few knew what nextsteps to take. Using a modified Delphi process [22], family goals were coded into seven thematic categories summarized in Table 2.
| 1) Getting the Right Interventions and Treatment |
| • Accessing developmental interventions (e.g. Applied Behavioral Analysis (ABA), social skills training; occupational, physical and speech therapy) |
| • Coordinating medical interventions (e.g. surgeries, subspecialty referrals, and medication management) |
| • Obtaining diagnostic evaluations |
| • Gaining nursing or home health support |
| 2) Paying for Healthcare and Related Needs |
| • Accessing/funding, insurance & related programs |
| • Managing out-of-pocket expenses |
| • Accessing Medicaid Waivers, other grant funding |
| • Accessing Medicaid for supplies (e.g. diapers) |
| 3) Quality of Family Life Needs |
| • Recreational & social activities |
| • Respite care |
| • Child-care |
| • Parenting, co-parenting and sibling supports |
| • Mental health support for family members |
| 4) Access and Communication Across Complex Healthcare Systems |
| • Communication among providers & organizations |
| • Partnerships with primary care/ the medical home |
| • Cohesion and collaboration among varied subspecialists |
| 5) Getting an Appropriate Education |
| • Access to early intervention services |
| • Communication and educational planning of support and services |
| • Advocacy & support |
| • Educationally related legal needs |
| • Health action plans for school |
| 6) Understanding the Diagnosis & Treatment |
| • Helping family, friends and relatives understand & accept the diagnosis |
| • Identifying evidence-based resources, quality information & support groups |
| 7) Meeting Basic Needs |
| • Nutritious food, adequate housing, transportation |
| • Overall safety interventions (e.g. car seats, gates, protective devices, identification tags) |
| • Social determinants of health related legal needs |
Table 2: Family/Caregiver goals: thematic categories (7) with examples
Engagement of families to co-create the SPoC as a care coordination approach connected them with a family-centered process and useful care tool. They valued being asked what was important to them and being listened to Table 3.
| Riley Care Coordination Program (RCCP) Family Quotes |
RCCP Team Member Quotes |
|---|---|
| “If you can bring us real care coordination, you will have saved our family” (Parent of a 9-year-old child with autism spectrum disorder) | “I can focus on my clinical responsibilities when I know my CC team members are following up with the children and families I see; I am confident they are getting the help they need” (Child Psychologist) |
| “I have felt so alone in this but care coordination has opened my mind. I now know how to use the many special services available to our daughter” (Parent of a 5-year-old with autism spectrum disorder). | “I have spent a lifetime learning the evidence-based strategies for children and families, yet the constraints of our payment system prevent me from ensuring that families access best practices and optimal services. Care coordination addresses this dilemma head on. It makes a difference (Developmental Pediatrician).” |
| “No one has ever asked questions about what matters to us before” (Parent of two children, ages 3 and 5, with neurodevelopmental disabilities). | “Learning family goals and using them to drive CC is better, more effective. I cannot go back to working the way I did before” (Care Coordinator). |
Table 3: RCCP Family, Clinician, and Care Coordinator Feedback Examples
They appreciated having ongoing access to a designated, prepared care coordinator. The coalesced information of the SPoC served to ease the burden of communication for families and was educational for their care neighborhood.
Few families fully comprehended the extent to which communication and coordination across multiple people, services, and systems would be an ongoing necessity. Many found developmental, behavioral, and educational systems intimidating and difficult to navigate. Families varied in their ability to take initiative with certain goals, some required significant assistance while others preferred more independence. Certain families had straightforward goals and needed a clear pathway (e.g. understanding a diagnosis or addressing safety needs), others necessitated more prolonged assistance and supports (e.g. regular check-ins or significant help with next-steps).
Riley care coordination team
Team members expressed their “passion” for ensuring that children and families get critical services and supports. When coordinator/clinician dyads met with families each week, establishing a trusting rapport was their priority. Each dyad used individualized approaches to balance the skills families brought to care coordination with areas requiring assistance. Family needs were continuous and ever-changing and coordinating care was demanding. Considerable day-to-day responsibilities included establishing networks across healthcare, insurance, education, and public programs within ever changing environments. Coordinators were challenged regarding where to draw professional boundaries such as determining how much to do with/ for families, for how long, and when a goal was unattainable. Program and system changes, such as new personnel or health insurance rules created a “Chutes and Ladders” effect causing coordination efforts to “start over”. Team members performed to their full capacity while relying upon one another’s distinct expertise. Demanding coordination work amidst frequent system changes coupled with uncertainty about what defines success created team stress. Vigilant program and team oversight, balancing care tasks and data collection, simplifying processes, and protecting time for reflective practice were strategies used to address these stressors.
RCCP adapted a theoretical model to help families gain early, more effective interventions and treatments. Detailed team roles and care processes required testing and redesign. Necessary program modifications included the number of families served per/coordinator; visit guidelines; SPoC templates; number of goals addressed per/family; follow-up, and specifications around exiting the RCCP. In spite of challenges, clinicians and coordinators reported satisfaction seeing families get what they needed, often comparing their RCCP experience with past “best efforts” that failed due to lack of care coordination capacity Table 3.
Specialists and primary care providers
Neurodevelopmental expertise is typically located within an urban children’s hospital. Primary care clinicians in urban, suburban and rural locations struggle to benefit from this knowledge. Primary care providers views regarding the optimal medical home location for children with complex needs are mixed. Some embrace chronic care as part of their practice, others choose to refer children with chronic care needs to subspecialists [23]. Certain clinicians request shared-care approaches to help bridge these knowledge gaps [24].
The RCCP provided technical assistance to primary care around health, educational and fiscal resources; this communication and SPoC related requests have been met with variable uptake. Some providers expressed gratitude for guidance and assumed a coordinating role; others showed more eagerness for RCCP staff to address tasks independent of them (e.g. Medicaid forms/waiver applications or school advocacy). Others asked for technical support before assuming coordination functions, thereby signaling a willingness to learn. One particular success was when a physician agreed to take a child into their practice in spite of it being “closed” as a result of the “usefulness of the SPoC”. These primary care partnerships are essential to locally support families and sustain care coordination. Strengthening relationships by offering medical and coordination expertise can systematically build primary care capacity as a fundamental cornerstone of healthcare.
Subspecialists welcomed access to care coordination for their patients and provided positive feedback regarding accomplishments. Soon they were referring all of their eligible patients causing the team to analyze whether coordination was being “prescribed” for families. Communication about family choices and timing of optimal enrollment are areas for future improvement.
Funding and sustainability
RCCP is set among, but not integrated within, six separate neurodevelopmental subspecialty divisions of a children’s hospital. Coordination served as a unifying force across these divisions. Still, daily communications, operations, fiscal challenges and capacity tested the RCCP’s equilibrium and capacity. Funding came from blended philanthropic, academic, and public support which proved challenging to sustain. In 2001 care coordination was described as an essential, cross-cutting innovation [25], yet today sustained funding for pediatric care coordination remains elusive [11]. Related savings requires time to demonstrate and may be accrued across multiple organizational budgets (e.g. health care, employers, education); thus, convincing health system leaders to invest in care coordination for children is extremely difficult. If networks working towards integrated, population health cannot adopt a pediatric model of care coordination, then children and family’s medical, developmental and social needs will go unmet.
Discussion
Co-creation and use of a SPoC to achieve care coordination with children and families with neurodevelopmental disabilities in a children’s hospital ambulatory care setting is a feasible endeavor. RCCP generated a pathway to family-centered care by eliciting and using family goals, documented in a SPoC, to drive care coordination activities. Families and providers benefited from this proactive approach which went beyond episodic, reactive care and coordination. These achievements required:
• Learning partnerships with families
• Teamwork with engagement among “Care Neighborhood” partners
• Studied implementation, analysis of lessons learned, and ongoing program redesign
Next steps include a quantitative analysis of RCCP’s impact upon families. Positive findings will facilitate movement from application of national standards and lessons learned, to a future adopted, supported and sustainable program.
Lessons are drawn from work applied with a subpopulation of children with neurodevelopmental disabilities. We cannot assume generalizability to all CYSHCN, but model testing with additional subpopulations will generate insight. Care coordination literature focuses predominantly on primary care medical home interventions, yet primary care may not always be the preferable or possible locus of clinical coordination for certain children.
What does it take to deliver quality, or in the words of one family “real” care coordination? The answer may be found by learning what matters most to children and families and addressing these priorities in partnerships. Investing in quality care coordination by using a shared plan of care approach with fidelity to national standards holds promise. Integrated health care networks working towards better care and population health would benefit from using this type of care coordination approach.
Funding Source
Funding for the RCCP implementation was provided by the Riley Children’s Foundation, the Indiana University School of Medicine, Department of Pediatrics and the Indiana State Department of Health.
Acknowledgement
What allowed this care coordination endeavor to be conceived and launched is the trans-disciplinary team who joined to support its application, study and ongoing improvement. In addition to the authors, recognition and significant gratitude go to: Care Coordinators (Margo Ramaker, MSW; Holly Paauwe, Family Leader, and Mary Heskett, RN); Project Coordinator (Ann Clark), and colleagues and leaders (Mary Cicarelli, MD, Nancy Swigonski, MD, MPH, Jordan Huskins, MD, Angela Tomlin, PhD, HSPP, Stephen Downs, MD, and IUSM Chairman of Pediatrics, D. Wade Clapp, MD).
REFERENCES
- McPherson M, Arango P, Fox H, et al. A new definition of children with special health care needs. Pediatrics. 1998;102:137-40.
- National Survey of Childrens Health. http://www.childhealthdata.org/.
- Kuo D, Cohen E, Agrawal R, et al. A national profile of caregiver challenges among more medically complex children with special health care needs. Arch Pediatr Adolesc Med. 2011;165:1020-6.
- Spencer N. Social, economic, and political determinants of child health. Pediatrics. 2003;112:704-6.
- Kogan M, Strickland B, Singh G, et al. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States 2005-2006. Pediatrics. 2008;22:1149-58.
- Hodgetts S, Zwaigenbaum L, Nicholas D. Profile and predictors of service needs for families of children with autism spectrum disorders. Autism. 2015;19:673-83.
- Carbone P, Behl D, Azor V. The medical home for children with autism spectrum disorders: parent and pediatrician perspectives. J Autism Dev Disord. 2010;40:317-24.
- Levy S, Frasso R, Colantonio S, et al. Shared Decision Making and Treatment Decisions for Young Children With Autism Spectrum Disorder. Acad Pediatr. 2016;16:571-78.
- Antonelli R, McAllister J, Popp J. Making Care Coordination a Critical Component of the Pediatric Health Care System: A Multidisciplinary Framework. New York, NY: The Commonwealth Fund; 2009.
- Berwick D, Nolan T, Whittington J. The Triple Aim. Health Affairs 2008;27:759-69.
- American Academy of Pediatrics. Patient and Family Centered Care Coordination: A Framework for Integrating Care for Children and Youth Across Multiple Systems Pediatrics. 2014;133.
- Baker A, Cronin K, Conway P, et al. Making the Comprehensive Shared Care Plan a Reality. NEJM Catalyst 2016.
- Berry JG. What Children with Medical Complexity, Their Families and Healthcare Providers Desearve for an Ideal Healthcare System. Lucile Packard Foundation for Children’s Health; 2015.
- Kuo D, McAllister J, Rossignol L, et al. Care Coordination for Children with Medical Complexity: Whose Care Is It, Anyway? Pediatrics 2018.
- AMCH: Standards for Systems of Care for Children and Youth with Special Health Care Needs. Lucile Packard Foundation for Childrens Health; 2014.
- Lucile Packard Foundation for Children's Health. The Super Parents The Super Parents Exhibit 2016.
- McAllister J. Achieving a Shared Plan of Care for Children and Youth with Special Health Care Needs: An Implementation Guide. Lucille Packard Foundation for Children's Healthcare: Lucille Packard Foundation for Children's Healthcare; 2014.
- Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Affairs. 2001;20:64-78.
- Gittell J. High Performance Healthcare Using the Power of Relationships to Achieve Quality, Efficiency and Resilience. NYC: The McGraw-Hill Companies; 2009.
- Nutting PA, Miller WL, Crabtree BF, et al. Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. Annals of Family Medicine. 2009;7:254-60.
- Senge P. The Fifth Discipline: The Art and Practice of the Learning Organization. USA: Doubleday; 2006.
- Dalkey N, Helmer O. An experimental application of the Delphi method to the use of experts. Management Science. 1963;9:458-67.
- Van CJ, Okumura M, Swigonski N, et al. Medical Homes for Children With Special Health Care Needs: Primary Care or Subspecialty Service. Acad Pediatr. 2016;16:366-72.
- Nolan R, Walker T, Hanson J, et al. Developmental Behavioral Pediatrician Support of the Medical Home for Children with Autism Spectrum Disorders. Developmental & Behavioral Pediatrics. 2016;37:687-93.
- IOM. Crossing the Quality Chasm: A New Health System for the 21st Century. 2001.