Intriguing variations of the tibial arteries and their clinical implications
Maria Atanasova1, Georgi P. Georgiev2* and Lazar Jelev1
1Department of Anatomy, Histology and Embryology, Medical University Sofia, Sofia, Bulgaria
2University Hospital of Orthopaedics “Prof. B. Boychev”, Medical University Sofia, Sofia, Bulgaria
- *Corresponding Author:
- Georgi P. Georgiev, MD
University Hospital of Orthopaedics, “Prof. B. Boychev”, Medical University Sofia, 56 Nicola Petkov Street, BG–1614 Sofia, Bulgaria
Tel: +359 883 357757
E-mail: georgievgp@yahoo.com
Date of Received: November 23rd, 2010
Date of Accepted: January 30th, 2011
Published Online: March 5th, 2011
IJAV. 2011; 4: 45–47.
[ft_below_content] =>Keywords
tibial arteries, anatomical variation, surgery of the leg
Introduction
The arterial network of the lower limb has a wide range of variations and attracts attention not only by anatomists but also by surgeons [1–9]. These variations are explained from the embryological abnormalities of the arterial pattern of the lower extremity [2,7,10]. From clinical point of view, the variant crural arteries may have an impact in the field of surgery and during catheterization procedures of the lower limb [5,9,11,12].
In this report, we present an interesting variation of the tibial arteries and discuss their anatomical variations. We also emphasize on the clinical implications of the aforementioned arteries.
Case Report
Unusual course of the anterior (AT) and posterior tibial (PT) arteries with interesting correlation was discovered during routine anatomical dissection of the right lower extremity in a 61-year-old formol-carbol fixed female cadaver for whom we have no information for previous diseases. The study was approved by the medico-legal office and the Local Ethics Committee.
In this case the popliteal artery descended obliquely through the popliteal fossa and entered the posterior compartment of the leg where it divided as usual into the AT and tibioperoneal trunk. The AT was hypoplastic and measured only 1.5 mm in diameter. It commenced at the lower border of the popliteus muscle and crossed forward between the two heads of the tibialis posterior muscle. Afterwards the artery passed through the aperture above the upper border of the interosseous membrane and descending on the anterior surface of the latter, where it ended above the ankle-joint.
The tibioperoneal trunk divided into the PT and the peroneal (PA) arteries at the lower border of the popliteal muscle, opposite the interval between the tibia and fibula. Then the PT (diameter 4.2 mm) extended obliquely downward, approaching the tibial side of the leg lying behind the tibia. Around 4.1 cm above the lateral malleolus, the PT gave a large anterior branch (diameter 3.8 mm), which crossed the interosseous membrane and prolonged similar to the distal part of the AT. Then it descended laterally on the anterior surface of the interosseous membrane and passed under tendon of the extensor digitorum longus muscle. After that it gave off the lateral tarsal artery (diameter 1.8 mm) and prolonged as the dorsalis pedis artery (diameter 3.7 mm). This artery passed medially forward from the ankle joint along the tibial side of the dorsum of the foot to the proximal part of the first intermetatarsal space. At this site the vessel divided into two branches, the first dorsal metatarsal and the deep plantar, as usual. After giving the large anterior branch, the rest of the PT continued its course distally, situated between the medial malleolus and the medial process of the calcaneal tuberosity. Under the origin of the adductor hallucis muscle it divided into the medial and lateral plantar arteries, as usual. In this case there was no unusual observation in the course and division of the PA as well as the deep peroneal and tibial nerves.
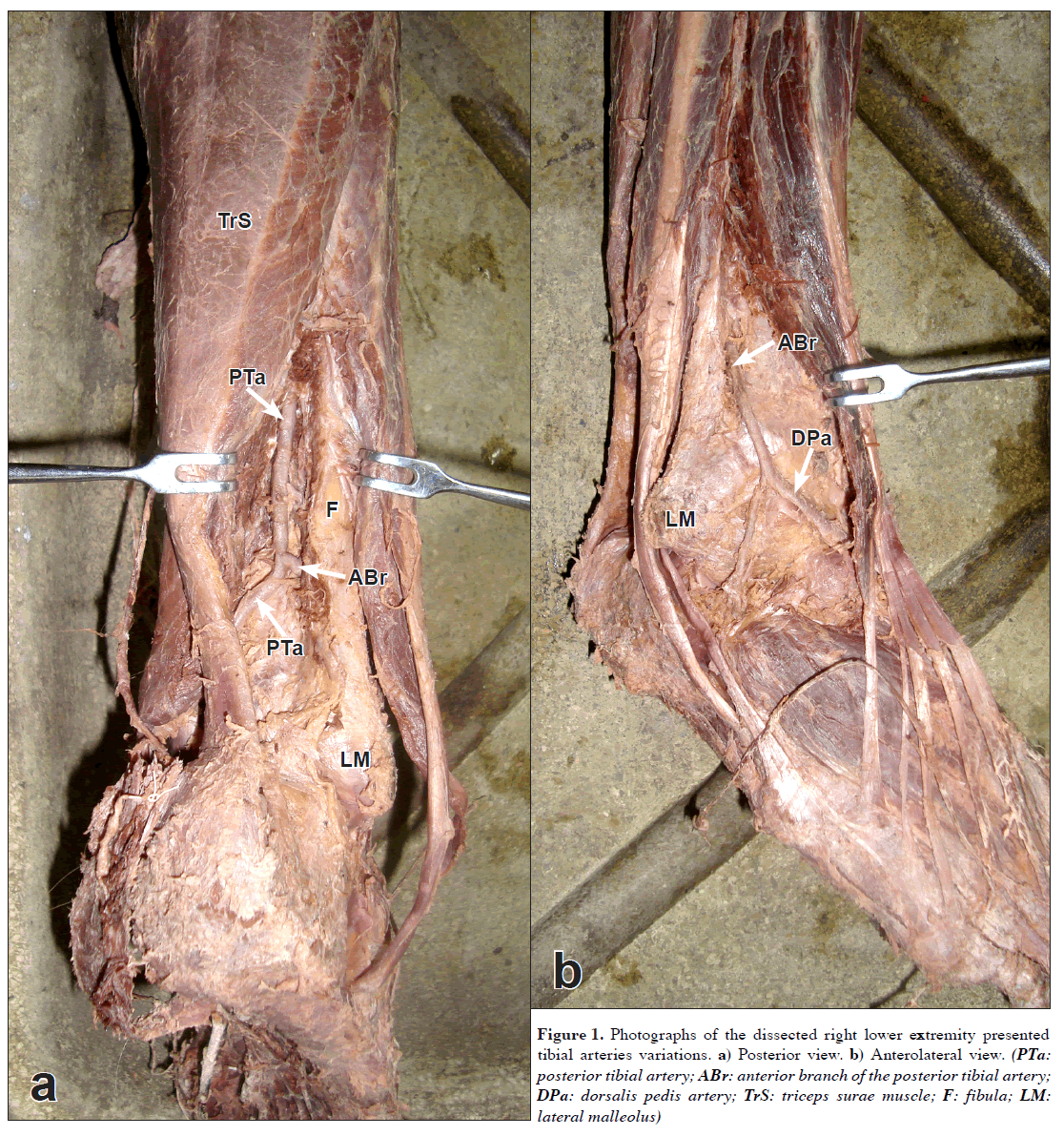
Figure 1: Photographs of the dissected right lower extremity presented tibial arteries variations. a) Posterior view. b) Anterolateral view. (PTa: posterior tibial artery; ABr: anterior branch of the posterior tibial artery; DPa: dorsalis pedis artery; TrS: triceps surae muscle; F: fibula; LM: lateral malleolus)
Discussion
Variations of the arteries of the lower limb, including absence, rudimentary reminders, variant courses and replacement areas of vascularization have been widely studied by anatomists and clinicians [3–7,9,13–16]. These arteries are not only of anatomical interest, but they also have important clinical significance [5,12,16]. The unusual arteries described in our report seem to be related to the aberrant tibial arteries and therefore we reviewed the previously reported variations of these arteries and also emphasized on their clinical implications.
Different anatomical variants of the AT have been described in the current literature. It may be small in diameter or entirely absent and replaced by perforating branches from the PT or PA. AT could also deviates toward the fibular side of the leg, regaining its usual positions anterior to the ankle [1,2,8].
The PT may be hypoplastic and its diameter reduced to 1–2 mm in the lower third of the leg [12]. The artery was described to be absent and replaced by the PA or saphenous artery because they are united by an anastomosis in an early stage of development [1,8]. On occasion, in the distal quarter of the leg PT pierces the interosseous membrane and it may joins to or replaces the AT [1,8]. Often, it flows in the distal part of the PA [1]. The irregular plantar distribution of the PT was also reported [8]. Unusual case of “superficial” PT has been reported by Jelev and Georgiev [16].
The arteries of the lower limb arise from two sources: the primary limb bud artery (sciatic artery) and the femoral artery. By the 14 mm embryonic stage the femoral artery has grown into the thigh and joined the sciatic artery and becomes the major supply artery to the lower limb. The more proximal part of the sciatic artery usually regresses; middle and distal segments persist to form the definitive popliteal artery and PA. The AT arises from the popliteal artery. The popliteal artery and the early distal femoral artery anastomose and form the PT [7]. In conclusion, arterial variations of lower limb can be explained by some combinations of persistent primitive arterial segments, abnormal fusions, and segmental hypoplasia or absence [7].
Arterial variations of the lower limb have definite clinical significance in surgical practice. The awareness of these variations is important to vascular surgeons during arterial reconstructions in femorodistal bypass graft procedures and embolectomy [7,12]. Recent advances in balloon catheter technology, used to treat lower limb ischemia in diabetic patients, allow percutaneous transluminal angioplasty of small arteries, which could be impeding by different AT variations in the leg [11]. The precise knowledge of vascular anatomy and its variations around the ankle is indispensable for surgical techniques, such as ankle arthroscopy or surgical release of clubfoot [5,12]. In addition, the best way to visualize all these variations can be via Doppler ultrasound or arteriography [9].
Conclusion
In conclusion, the reported here constellation of arterial variations of the leg is not only an intriguing anatomical finding. The presence of these structures could be of clinical importance in reconstruction graft procedures, embolectomy, catheterization procedures, surgical release of clubfoot and ankle arthroscopy, as well as complicating imaging observations.
References
- Adachi B. Anatomie der Japaner I. Das Arteriensystem der Japaner. Aorta thoracalis e Arcus plantaris profundus. Bd II., Kyoto, Verlag der Keiserlich-Japan Univ. 1928; 215–241.
- Lippert H, Pabst R. Arterial variations in man: classification and frequency. Munich, J. F. Bergman Verlag. 1985; 63.
- Ali MW, Mohajir AM. Dorsalis pedis artery: variations and clinical significance. J Indian Med Assoc. 1996; 94: 417–418.
- Day CP, Orme R. Popliteal artery branching patterns – an angiographic study. Clin Radiol. 2006; 61: 696–699.
- Vazquez T, Rodriguez-Niedenfuhr M, Parkin I, Viejo F, Sanudo J. Anatomic study of blood supply of the dorsum of the foot and ankle. Arthroscopy. 2006; 22: 287–290.
- Jung W, Oh CS, Won HS, Chung IH. Unilateral arteria peronea magna associated with bilateral replaced dorsalis pedis arteries. Surg Radiol Anat. 2008; 30: 449–452.
- Kil SW, Jung GS. Anatomical variations of the popliteal artery and its tibial branches: analysis in 1242 extremities. Cardiovasc Intervent Radiol. 2009; 32: 233–240.
- Bergman RA, Afifi AK, Miyauchi R. Illustrated encyclopaedia of human anatomic variation. http://www.anatomyatlases.org/AnatomicVariants/Cardiovascular/Text/Arteries/TibialTibialisAnterior.shtml (accessed November 2010).
- Mavili E, Donmez H, Kahriman G, Ozaslamaci A, Ozcan N, Tasdemir K. Popliteal artery branching patterns detected by digital subtraction angiography. Diagn Interv Radiol. 2011; 17: 80–83.
- Sahin B, Bilgic S. Two rare arterial variations of the deep femoral artery in the newborn. Surg Radial Anat. 1998; 20: 233–235.
- Durham JR, Horowitz JD, Wright JG, Smead WL. Percutaneous transluminal angioplasty of tibial arteries for limb salvage in the high-risk diabetic patient. Ann Vasc Surg. 1994; 8: 48–53.
- Jiji PJ, D’Costa S, Nayak SR, Prabhu LV, Pai MM, Vadgaonkar R, Rai R, Sugavasi R. Hypoplastic posterior tibial artery and the enlarged peroneal artery supplying the posterior crural region: A rare variation. J Vasc Bras. 2008; 7: 272–274.
- Sanders RJ, Alston GK. Variations and anomalies of the popliteal and tibial arteries. Am J Surg. 1986; 152: 531–534.
- Kim D, Orron DE, Skillman JJ. Surgical significance of popliteal arterial variants. A unified angiographic classification. Ann Surg. 1989; 210: 776–781.
- Yamada T, Gloviczki P, Bower TC, Naessens JM, Carmichael SW. Variations of the arterial anatomy of the foot. Am J Surg. 1993; 166: 130–135.
- Jelev L, Georgiev GP. A unique case of “superficial” posterior tibial artery: Anatomical and clinical considerations. Eur J Vasc Endovasc Surg Extra. 2010; 20: e30–31.
Maria Atanasova1, Georgi P. Georgiev2* and Lazar Jelev1
1Department of Anatomy, Histology and Embryology, Medical University Sofia, Sofia, Bulgaria
2University Hospital of Orthopaedics “Prof. B. Boychev”, Medical University Sofia, Sofia, Bulgaria
- *Corresponding Author:
- Georgi P. Georgiev, MD
University Hospital of Orthopaedics, “Prof. B. Boychev”, Medical University Sofia, 56 Nicola Petkov Street, BG–1614 Sofia, Bulgaria
Tel: +359 883 357757
E-mail: georgievgp@yahoo.com
Date of Received: November 23rd, 2010
Date of Accepted: January 30th, 2011
Published Online: March 5th, 2011
IJAV. 2011; 4: 45–47.
Abstract
Unusual course and branching pattern of the tibial arteries were discovered during routine anatomical dissection of the right lower extremity of a 61-year-old female cadaver. The arteries of the crural region arose from the popliteal artery, as usual. However, the anterior tibial artery was hypoplastic and supplying the anterior calf muscles ended above the ankle joint. Instead, the posterior tibial artery gave off a large anterior branch, which crossed the lowest portion of the interosseous membrane and prolonged as the most distal continuation of the anterior tibial artery –the dorsalis pedis artery. The rest of the posterior tibial artery continued its course distally and divided into the usual medial and lateral plantar arteries. We briefly review the reported variations of the tibial arteries and discussed their clinical relevance.
-Keywords
tibial arteries, anatomical variation, surgery of the leg
Introduction
The arterial network of the lower limb has a wide range of variations and attracts attention not only by anatomists but also by surgeons [1–9]. These variations are explained from the embryological abnormalities of the arterial pattern of the lower extremity [2,7,10]. From clinical point of view, the variant crural arteries may have an impact in the field of surgery and during catheterization procedures of the lower limb [5,9,11,12].
In this report, we present an interesting variation of the tibial arteries and discuss their anatomical variations. We also emphasize on the clinical implications of the aforementioned arteries.
Case Report
Unusual course of the anterior (AT) and posterior tibial (PT) arteries with interesting correlation was discovered during routine anatomical dissection of the right lower extremity in a 61-year-old formol-carbol fixed female cadaver for whom we have no information for previous diseases. The study was approved by the medico-legal office and the Local Ethics Committee.
In this case the popliteal artery descended obliquely through the popliteal fossa and entered the posterior compartment of the leg where it divided as usual into the AT and tibioperoneal trunk. The AT was hypoplastic and measured only 1.5 mm in diameter. It commenced at the lower border of the popliteus muscle and crossed forward between the two heads of the tibialis posterior muscle. Afterwards the artery passed through the aperture above the upper border of the interosseous membrane and descending on the anterior surface of the latter, where it ended above the ankle-joint.
The tibioperoneal trunk divided into the PT and the peroneal (PA) arteries at the lower border of the popliteal muscle, opposite the interval between the tibia and fibula. Then the PT (diameter 4.2 mm) extended obliquely downward, approaching the tibial side of the leg lying behind the tibia. Around 4.1 cm above the lateral malleolus, the PT gave a large anterior branch (diameter 3.8 mm), which crossed the interosseous membrane and prolonged similar to the distal part of the AT. Then it descended laterally on the anterior surface of the interosseous membrane and passed under tendon of the extensor digitorum longus muscle. After that it gave off the lateral tarsal artery (diameter 1.8 mm) and prolonged as the dorsalis pedis artery (diameter 3.7 mm). This artery passed medially forward from the ankle joint along the tibial side of the dorsum of the foot to the proximal part of the first intermetatarsal space. At this site the vessel divided into two branches, the first dorsal metatarsal and the deep plantar, as usual. After giving the large anterior branch, the rest of the PT continued its course distally, situated between the medial malleolus and the medial process of the calcaneal tuberosity. Under the origin of the adductor hallucis muscle it divided into the medial and lateral plantar arteries, as usual. In this case there was no unusual observation in the course and division of the PA as well as the deep peroneal and tibial nerves.
Figure 1: Photographs of the dissected right lower extremity presented tibial arteries variations. a) Posterior view. b) Anterolateral view. (PTa: posterior tibial artery; ABr: anterior branch of the posterior tibial artery; DPa: dorsalis pedis artery; TrS: triceps surae muscle; F: fibula; LM: lateral malleolus)
Discussion
Variations of the arteries of the lower limb, including absence, rudimentary reminders, variant courses and replacement areas of vascularization have been widely studied by anatomists and clinicians [3–7,9,13–16]. These arteries are not only of anatomical interest, but they also have important clinical significance [5,12,16]. The unusual arteries described in our report seem to be related to the aberrant tibial arteries and therefore we reviewed the previously reported variations of these arteries and also emphasized on their clinical implications.
Different anatomical variants of the AT have been described in the current literature. It may be small in diameter or entirely absent and replaced by perforating branches from the PT or PA. AT could also deviates toward the fibular side of the leg, regaining its usual positions anterior to the ankle [1,2,8].
The PT may be hypoplastic and its diameter reduced to 1–2 mm in the lower third of the leg [12]. The artery was described to be absent and replaced by the PA or saphenous artery because they are united by an anastomosis in an early stage of development [1,8]. On occasion, in the distal quarter of the leg PT pierces the interosseous membrane and it may joins to or replaces the AT [1,8]. Often, it flows in the distal part of the PA [1]. The irregular plantar distribution of the PT was also reported [8]. Unusual case of “superficial” PT has been reported by Jelev and Georgiev [16].
The arteries of the lower limb arise from two sources: the primary limb bud artery (sciatic artery) and the femoral artery. By the 14 mm embryonic stage the femoral artery has grown into the thigh and joined the sciatic artery and becomes the major supply artery to the lower limb. The more proximal part of the sciatic artery usually regresses; middle and distal segments persist to form the definitive popliteal artery and PA. The AT arises from the popliteal artery. The popliteal artery and the early distal femoral artery anastomose and form the PT [7]. In conclusion, arterial variations of lower limb can be explained by some combinations of persistent primitive arterial segments, abnormal fusions, and segmental hypoplasia or absence [7].
Arterial variations of the lower limb have definite clinical significance in surgical practice. The awareness of these variations is important to vascular surgeons during arterial reconstructions in femorodistal bypass graft procedures and embolectomy [7,12]. Recent advances in balloon catheter technology, used to treat lower limb ischemia in diabetic patients, allow percutaneous transluminal angioplasty of small arteries, which could be impeding by different AT variations in the leg [11]. The precise knowledge of vascular anatomy and its variations around the ankle is indispensable for surgical techniques, such as ankle arthroscopy or surgical release of clubfoot [5,12]. In addition, the best way to visualize all these variations can be via Doppler ultrasound or arteriography [9].
Conclusion
In conclusion, the reported here constellation of arterial variations of the leg is not only an intriguing anatomical finding. The presence of these structures could be of clinical importance in reconstruction graft procedures, embolectomy, catheterization procedures, surgical release of clubfoot and ankle arthroscopy, as well as complicating imaging observations.
References
- Adachi B. Anatomie der Japaner I. Das Arteriensystem der Japaner. Aorta thoracalis e Arcus plantaris profundus. Bd II., Kyoto, Verlag der Keiserlich-Japan Univ. 1928; 215–241.
- Lippert H, Pabst R. Arterial variations in man: classification and frequency. Munich, J. F. Bergman Verlag. 1985; 63.
- Ali MW, Mohajir AM. Dorsalis pedis artery: variations and clinical significance. J Indian Med Assoc. 1996; 94: 417–418.
- Day CP, Orme R. Popliteal artery branching patterns – an angiographic study. Clin Radiol. 2006; 61: 696–699.
- Vazquez T, Rodriguez-Niedenfuhr M, Parkin I, Viejo F, Sanudo J. Anatomic study of blood supply of the dorsum of the foot and ankle. Arthroscopy. 2006; 22: 287–290.
- Jung W, Oh CS, Won HS, Chung IH. Unilateral arteria peronea magna associated with bilateral replaced dorsalis pedis arteries. Surg Radiol Anat. 2008; 30: 449–452.
- Kil SW, Jung GS. Anatomical variations of the popliteal artery and its tibial branches: analysis in 1242 extremities. Cardiovasc Intervent Radiol. 2009; 32: 233–240.
- Bergman RA, Afifi AK, Miyauchi R. Illustrated encyclopaedia of human anatomic variation. http://www.anatomyatlases.org/AnatomicVariants/Cardiovascular/Text/Arteries/TibialTibialisAnterior.shtml (accessed November 2010).
- Mavili E, Donmez H, Kahriman G, Ozaslamaci A, Ozcan N, Tasdemir K. Popliteal artery branching patterns detected by digital subtraction angiography. Diagn Interv Radiol. 2011; 17: 80–83.
- Sahin B, Bilgic S. Two rare arterial variations of the deep femoral artery in the newborn. Surg Radial Anat. 1998; 20: 233–235.
- Durham JR, Horowitz JD, Wright JG, Smead WL. Percutaneous transluminal angioplasty of tibial arteries for limb salvage in the high-risk diabetic patient. Ann Vasc Surg. 1994; 8: 48–53.
- Jiji PJ, D’Costa S, Nayak SR, Prabhu LV, Pai MM, Vadgaonkar R, Rai R, Sugavasi R. Hypoplastic posterior tibial artery and the enlarged peroneal artery supplying the posterior crural region: A rare variation. J Vasc Bras. 2008; 7: 272–274.
- Sanders RJ, Alston GK. Variations and anomalies of the popliteal and tibial arteries. Am J Surg. 1986; 152: 531–534.
- Kim D, Orron DE, Skillman JJ. Surgical significance of popliteal arterial variants. A unified angiographic classification. Ann Surg. 1989; 210: 776–781.
- Yamada T, Gloviczki P, Bower TC, Naessens JM, Carmichael SW. Variations of the arterial anatomy of the foot. Am J Surg. 1993; 166: 130–135.
- Jelev L, Georgiev GP. A unique case of “superficial” posterior tibial artery: Anatomical and clinical considerations. Eur J Vasc Endovasc Surg Extra. 2010; 20: e30–31.