Large vestibular aqueduct syndrome: report of 3 cases
Guler Berkiten1*, Mahmut Babalik2, Muhlis Bal1, Suzan Onol3
1Department of Otorhinolaryngology, Okmeydani Education and Research Hospital, Istanbul, Turkey.
2Department of Otorhinolaryngology, Vakfikebir Hospital, Trabzon, Turkey.
3Department of Radiology, Okmeydani Education and Research Hospital, Istanbul, Turkey.
- *Corresponding Author:
- Guler Berkiten, MD
Department of Otorhinolaryngology, Okmeydani Education and Research Hospital, Istanbul, 34384, Turkey.
Tel: +90 505 7278724
E-mail: gulerberkiten@gmail.com
Date of Received: August 11th, 2011
Date of Accepted: November 19th, 2011
Published Online: December 21st, 2011
© IJAV. 2011; 4: 200–203.
[ft_below_content] =>Keywords
large vestibular aqueduct syndrome, sensorineural hearing loss, sudden hearing loss
Introduction
Large vestibular aqueduct syndrome (LVAS) is characterized by the enlargement of the vestibular aqueduct associated with sensorineural hearing loss (SNHL) [1].
It was first described by Valvassori and Clemis in 1978 [2]. LVAS may be present in 1.5% of childhood and adolescent cases of SNHL [1,3]. LVAS is generally bilateral (59–94%) and commonly observed in females (60–66%) [4].
We analyzed three cases of LVAS encountered at the ENT Department of Okmeydani Education and Research Hospital. Diagnosis, manifestations and treatment of LVAS, which is rarely seen, are presented with literature data.
Case Report
Case 1
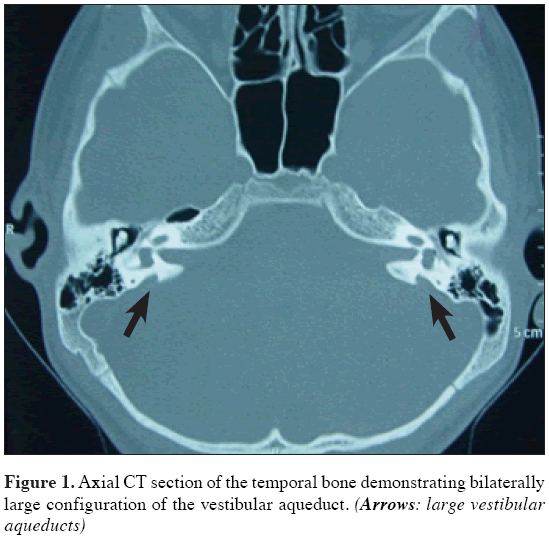
E.K., 14-year-old male. His mother reported that he experienced progressive hearing loss beginning in childhood and delay in language development (bilateral mixed hearing loss diagnosed at audiometry), using bilateral hearing aid since the age of 2 years. At that time he was misdiagnosed as having otitis media with effusion, whereas he was diagnosed as having SNHL later at about 2 years ago. In his clinical history he presented language development delay in childhood. He presented a family history of deafness in grandfather and brother. His gestation and delivery history were uneventful. Serological tests were negative. Thyroid function tests and neck palpation were normal (negative Pendred syndrome screening). The physical examination presented normal otoscopy. The pure tone threshold averages of right and left ears were 95 and 92 dB, respectively. Tympanograms showed type C in both of the ears. Both ears showed no acoustic reflex. Temporal bone computed tomography (CT) scan demonstrated bilateral large vestibular aqueduct (LVA), approximately 3 mm in width, with normal aspect of cochlea and vestibule (Figure 1).
Case 2
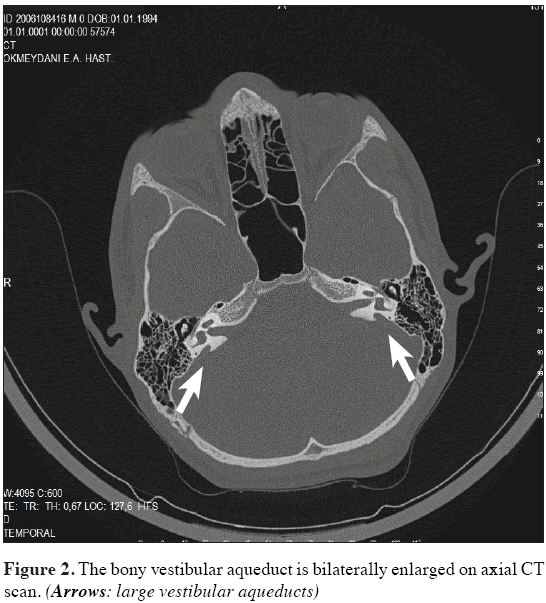
E.C.K, 16-year-old male, sibling of the case 1. His mother first noticed that he spoke too loud and needed the TV volume always up and did not respond to sounds. He saw an otolaryngologist, who asked for audiometry and confirmed severe hearing loss on the left and moderate hearing loss on the right without any apparent defined cause. He was using bilateral hearing aid since the age of 3.5 years. His grandfather and brother have hearing loss. His gestation and delivery history were uneventful. Thyroid function tests and neck palpation were normal. ENT examination was normal. The pure tone threshold averages of right and left ears were 67 and 105 dB, respectively. Tympanograms showed type A in both ears. Acoustic reflex was bilaterally absent. Temporal bone CT scan evidenced bilateral LVA with normal cochlea and vestibule (Figure 2). The mean diameter of the vestibular aqueduct was 3 mm on the right and 4 mm on the left side.
Case 3
N.K., 23-year-old female. She admitted to our hospital with sudden hearing loss in the right ear and ringing, tinnitus, fullness, vertigo, following 3 days after upper respiratory tract infection. The patient had been diagnosed with profound SNHL on the left and moderately severe SNHL on the right at the age of 2 years, and she had been recommended a hearing aid. Subsequently, the progressing hearing loss in the patient with pure tone average for the left ear was 110 dB and for the right ear 70 dB. Owing to the SNHL, patient had been using hearing aid in right ear, since she was 15. Current hearing worsened during the recent 3 days and the patient could not benefit from the hearing aid. The patient was hospitalized in our clinic with a pre-diagnosis of right sudden hearing loss. She did not have the history of barotrauma, or head and ear trauma. No familial hearing loss was present. No clinical manifestations presented in the patient, except psoriasis.
ENT examination was normal. In the pure tone audiometry, bilateral pure tone averages were 110 dB. Tympanograms revealed to be type A in both ears. Acoustic reflex was bilaterally absent. Thyroid function tests and neck palpation were normal. Other routine and immunologic tests had no significance.
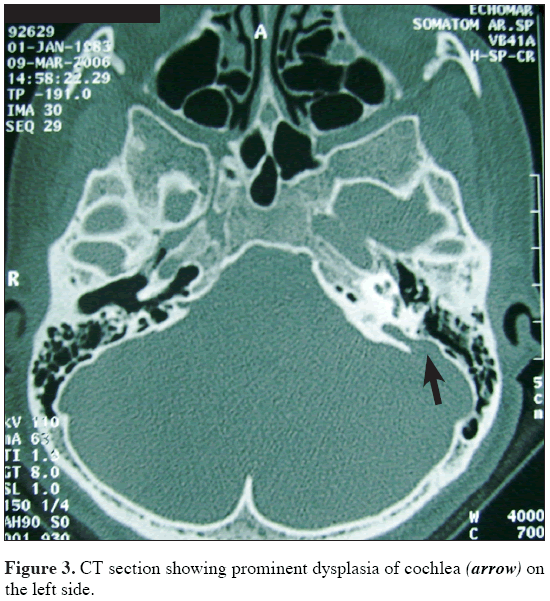
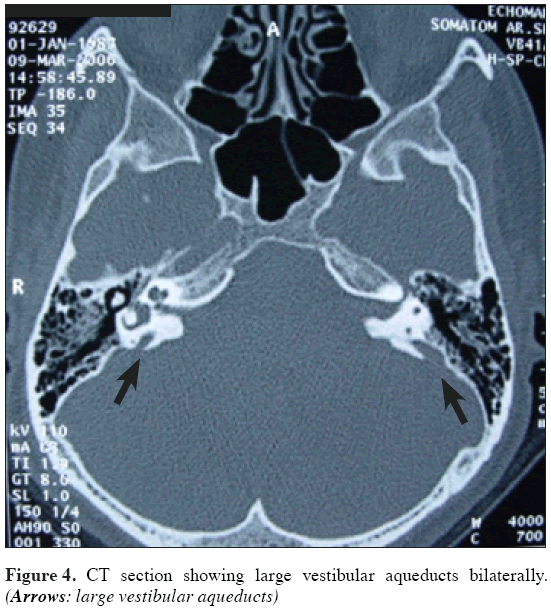
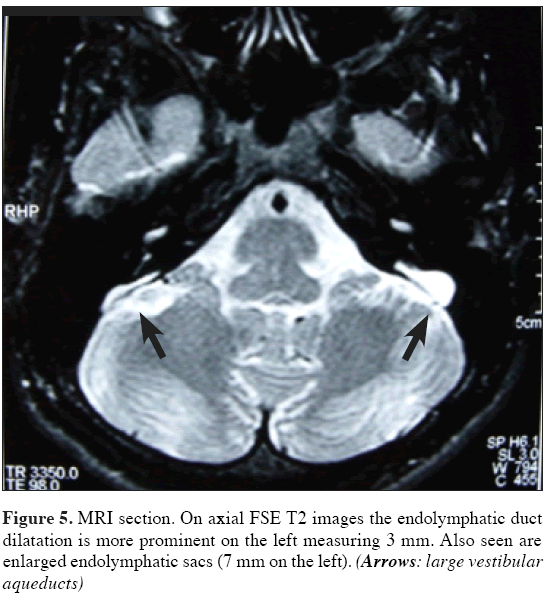
The temporal bone CT detected bilateral LVA (approximately 5 mm in width) and prominent dysplasia of cochlea in the left side (Figures 3, 4). MRI results were consistent with the CT (Figure 5).
1 mg/kg methyl-prednisolone was initiated to the patient and continued for 10 days, thereafter; dose was gradually decreased and stopped on the 20th day. The patient was administered with Dextran 40 (Rheomacrodex®, 2x1) for 5 days and Pentoxifylline 300 mg ampule (Trental®, 2x2) for 7 days. At the 13th day of the treatment, the hearing level was improved to the previous level.
Discussion
LVA is the most common malformation of inner ear which is detectable via radiological imaging [2,3]. LVAS is defined as the combination of the clinically apparent sensorineural hearing loss in a child and the identification of the large vestibular aqueduct (LVA) detected on a temporal bone CT or by the presence of large endolymphatic duct or sac on inner ear MRI [3].
Even after investigating such factors, the etiology may remain unknown. There are several theories on LVA formation. Some authors have suggested that it results from an arrest of embryological development at an early 5-week stage [3,4], but others suggested that the associated hearing loss develops in early childhood [5].
Some authors reported that LVAS had familial characteristics [1,3,4,6,7]. Griffith et al. first described familial occurrence of LVAS which seemed to have been inherited in a autosomal recessive manner [7]. Nowak and Messner reported 2 cases (including sister and little brother) suffered from LVA [8]. In our cases, patient 1 and 2 were siblings and they also presented family history of deafness in their grandfather.
LVAS is generally associated with other cochlear and vestibular abnormalities [2]. Our patient 3 also had cochlear dysplasia. In addition, tinnitus and vertigo were associated with sudden hearing loss. LVAS may be associated with Mondini’s dysplasia and Pendred Syndrome. We also investigated congenital symptoms such as Pendred Syndrome and Mondini’s Dysplasia but results were negative.
Hearing loss generally develops during the early childhood, less commonly in adolescence and rarely in adulthood. Hearing level may be variable [1]. Hearing loss in LVAS is usually bilateral SNHL or sometimes with mixed hearing loss; but rarely, conductive hearing loss may also be observed. Sudden hearing loss may also be observed as a result of minor head traumas, sudden pressure changes, increased intracranial pressure, upper respiratory tract infection or exercise [2,5,9,10]. Our patient 3 had also sudden hearing loss after upper respiratory tract infection.
Treatment of LVAS is medical or surgical [1,6]. Surgical treatment is still controversial. For treatment of sudden hearing loss in LVAS, vasodilator medications, steroids and neuronourishing medications are used [10]. In our patient 3, we obtained good results with steroid treatment. Conservative treatments may be considered to try to reduce the risk of hearing loss by trauma; hearing aids and speech therapy may also be considered [1,5,7].
Conclusion
LVAS should be considered primarily for the differential diagnosis of SNHL, which develops in patients during early childhood and adolescence. As soon as the hearing deterioration of a child with LVAS is recognized, aggressive treatment such as corticosteroid therapy should be implemented immediately.
Acknowledgements
Our sincere thanks to all people who helped and supported during the writing of this manuscript.
References
- Jackler RK, De La Cruz A. The large vestibular aqueduct syndrome. Laryngoscope. 1989; 99: 1238–1243.
- Valvassori GE, Clemis JD. The large vestibular aqueduct syndrome. Laryngoscope. 1978; 88: 723–728.
- Pyle MG. Embryological development and large vestibular aqueduct syndrome. Laryngoscope. 2000; 110: 1837–1842.
- Emmett JR. The large vestibular aqueduct syndrome. Am J Otol. 1985; 6: 387–415.
- Okumura T, Takahashi H, Honjo I, Takagi A, Mitamura K. Sensorioneural hearing loss in patients with large vestibular aqueduct. Laryngoscope. 1995; 105: 289–294.
- Ramirez-Camacho R, Ramon Garcia Berrocal J, Arellano B, Trinidad A. Familial isolated unilateral large vestibular aqueduct syndrome. ORL J Otorhinolaryngol Relat Spec. 2003; 65: 45–48.
- Griffith AJ, Arts A, Downs C, Innis JW, Shepard NT, Sheldon S, Gebarski SS. Familial large vestibular aqueduct syndrome. Laryngoscope. 1996; 106: 960–965.
- Nowak KC, Messner AH. Isolated large vestibular aqueduct syndrome in a family. Ann Otol Rhinol Laryngol. 2000; 109: 40–44.
- Lin CY, Lin SL, Kao CC, Wu JL. The remediation of hearing deterioration in children with large vestibular aqueduct syndrome. Auris Nasus Larynx. 2005; 32: 99–105.
- Wang J, Huang X, Chen H, Cheng Q. Sudden deafness with large vestibular aqueduct (case report and literatures review). Lin Chuang Er Bi Yan Hou Ke Za Zhi. 2002; 16: 515–517. (Chinese)
Guler Berkiten1*, Mahmut Babalik2, Muhlis Bal1, Suzan Onol3
1Department of Otorhinolaryngology, Okmeydani Education and Research Hospital, Istanbul, Turkey.
2Department of Otorhinolaryngology, Vakfikebir Hospital, Trabzon, Turkey.
3Department of Radiology, Okmeydani Education and Research Hospital, Istanbul, Turkey.
- *Corresponding Author:
- Guler Berkiten, MD
Department of Otorhinolaryngology, Okmeydani Education and Research Hospital, Istanbul, 34384, Turkey.
Tel: +90 505 7278724
E-mail: gulerberkiten@gmail.com
Date of Received: August 11th, 2011
Date of Accepted: November 19th, 2011
Published Online: December 21st, 2011
© IJAV. 2011; 4: 200–203.
Abstract
Large vestibular aqueduct syndrome (LVAS) is characterized by the enlargement of the vestibular aqueduct associated with sensorineural hearing loss (SNHL). The aim of this study was to report three cases of LVAS encountered at the Okmeydani Education and Research Hospital. Two of these three cases were siblings. Subjects included two males and one female, with an age range from 14 to 23 years. Siblings also presented a family history of deafness in their grandfather. The other case was a 23-year-old female who had been diagnosed with SNHL. Diagnosis, manifestations and treatment of LVAS are presented with literature data.
-Keywords
large vestibular aqueduct syndrome, sensorineural hearing loss, sudden hearing loss
Introduction
Large vestibular aqueduct syndrome (LVAS) is characterized by the enlargement of the vestibular aqueduct associated with sensorineural hearing loss (SNHL) [1].
It was first described by Valvassori and Clemis in 1978 [2]. LVAS may be present in 1.5% of childhood and adolescent cases of SNHL [1,3]. LVAS is generally bilateral (59–94%) and commonly observed in females (60–66%) [4].
We analyzed three cases of LVAS encountered at the ENT Department of Okmeydani Education and Research Hospital. Diagnosis, manifestations and treatment of LVAS, which is rarely seen, are presented with literature data.
Case Report
Case 1
E.K., 14-year-old male. His mother reported that he experienced progressive hearing loss beginning in childhood and delay in language development (bilateral mixed hearing loss diagnosed at audiometry), using bilateral hearing aid since the age of 2 years. At that time he was misdiagnosed as having otitis media with effusion, whereas he was diagnosed as having SNHL later at about 2 years ago. In his clinical history he presented language development delay in childhood. He presented a family history of deafness in grandfather and brother. His gestation and delivery history were uneventful. Serological tests were negative. Thyroid function tests and neck palpation were normal (negative Pendred syndrome screening). The physical examination presented normal otoscopy. The pure tone threshold averages of right and left ears were 95 and 92 dB, respectively. Tympanograms showed type C in both of the ears. Both ears showed no acoustic reflex. Temporal bone computed tomography (CT) scan demonstrated bilateral large vestibular aqueduct (LVA), approximately 3 mm in width, with normal aspect of cochlea and vestibule (Figure 1).
Case 2
E.C.K, 16-year-old male, sibling of the case 1. His mother first noticed that he spoke too loud and needed the TV volume always up and did not respond to sounds. He saw an otolaryngologist, who asked for audiometry and confirmed severe hearing loss on the left and moderate hearing loss on the right without any apparent defined cause. He was using bilateral hearing aid since the age of 3.5 years. His grandfather and brother have hearing loss. His gestation and delivery history were uneventful. Thyroid function tests and neck palpation were normal. ENT examination was normal. The pure tone threshold averages of right and left ears were 67 and 105 dB, respectively. Tympanograms showed type A in both ears. Acoustic reflex was bilaterally absent. Temporal bone CT scan evidenced bilateral LVA with normal cochlea and vestibule (Figure 2). The mean diameter of the vestibular aqueduct was 3 mm on the right and 4 mm on the left side.
Case 3
N.K., 23-year-old female. She admitted to our hospital with sudden hearing loss in the right ear and ringing, tinnitus, fullness, vertigo, following 3 days after upper respiratory tract infection. The patient had been diagnosed with profound SNHL on the left and moderately severe SNHL on the right at the age of 2 years, and she had been recommended a hearing aid. Subsequently, the progressing hearing loss in the patient with pure tone average for the left ear was 110 dB and for the right ear 70 dB. Owing to the SNHL, patient had been using hearing aid in right ear, since she was 15. Current hearing worsened during the recent 3 days and the patient could not benefit from the hearing aid. The patient was hospitalized in our clinic with a pre-diagnosis of right sudden hearing loss. She did not have the history of barotrauma, or head and ear trauma. No familial hearing loss was present. No clinical manifestations presented in the patient, except psoriasis.
ENT examination was normal. In the pure tone audiometry, bilateral pure tone averages were 110 dB. Tympanograms revealed to be type A in both ears. Acoustic reflex was bilaterally absent. Thyroid function tests and neck palpation were normal. Other routine and immunologic tests had no significance.
The temporal bone CT detected bilateral LVA (approximately 5 mm in width) and prominent dysplasia of cochlea in the left side (Figures 3, 4). MRI results were consistent with the CT (Figure 5).
1 mg/kg methyl-prednisolone was initiated to the patient and continued for 10 days, thereafter; dose was gradually decreased and stopped on the 20th day. The patient was administered with Dextran 40 (Rheomacrodex®, 2x1) for 5 days and Pentoxifylline 300 mg ampule (Trental®, 2x2) for 7 days. At the 13th day of the treatment, the hearing level was improved to the previous level.
Discussion
LVA is the most common malformation of inner ear which is detectable via radiological imaging [2,3]. LVAS is defined as the combination of the clinically apparent sensorineural hearing loss in a child and the identification of the large vestibular aqueduct (LVA) detected on a temporal bone CT or by the presence of large endolymphatic duct or sac on inner ear MRI [3].
Even after investigating such factors, the etiology may remain unknown. There are several theories on LVA formation. Some authors have suggested that it results from an arrest of embryological development at an early 5-week stage [3,4], but others suggested that the associated hearing loss develops in early childhood [5].
Some authors reported that LVAS had familial characteristics [1,3,4,6,7]. Griffith et al. first described familial occurrence of LVAS which seemed to have been inherited in a autosomal recessive manner [7]. Nowak and Messner reported 2 cases (including sister and little brother) suffered from LVA [8]. In our cases, patient 1 and 2 were siblings and they also presented family history of deafness in their grandfather.
LVAS is generally associated with other cochlear and vestibular abnormalities [2]. Our patient 3 also had cochlear dysplasia. In addition, tinnitus and vertigo were associated with sudden hearing loss. LVAS may be associated with Mondini’s dysplasia and Pendred Syndrome. We also investigated congenital symptoms such as Pendred Syndrome and Mondini’s Dysplasia but results were negative.
Hearing loss generally develops during the early childhood, less commonly in adolescence and rarely in adulthood. Hearing level may be variable [1]. Hearing loss in LVAS is usually bilateral SNHL or sometimes with mixed hearing loss; but rarely, conductive hearing loss may also be observed. Sudden hearing loss may also be observed as a result of minor head traumas, sudden pressure changes, increased intracranial pressure, upper respiratory tract infection or exercise [2,5,9,10]. Our patient 3 had also sudden hearing loss after upper respiratory tract infection.
Treatment of LVAS is medical or surgical [1,6]. Surgical treatment is still controversial. For treatment of sudden hearing loss in LVAS, vasodilator medications, steroids and neuronourishing medications are used [10]. In our patient 3, we obtained good results with steroid treatment. Conservative treatments may be considered to try to reduce the risk of hearing loss by trauma; hearing aids and speech therapy may also be considered [1,5,7].
Conclusion
LVAS should be considered primarily for the differential diagnosis of SNHL, which develops in patients during early childhood and adolescence. As soon as the hearing deterioration of a child with LVAS is recognized, aggressive treatment such as corticosteroid therapy should be implemented immediately.
Acknowledgements
Our sincere thanks to all people who helped and supported during the writing of this manuscript.
References
- Jackler RK, De La Cruz A. The large vestibular aqueduct syndrome. Laryngoscope. 1989; 99: 1238–1243.
- Valvassori GE, Clemis JD. The large vestibular aqueduct syndrome. Laryngoscope. 1978; 88: 723–728.
- Pyle MG. Embryological development and large vestibular aqueduct syndrome. Laryngoscope. 2000; 110: 1837–1842.
- Emmett JR. The large vestibular aqueduct syndrome. Am J Otol. 1985; 6: 387–415.
- Okumura T, Takahashi H, Honjo I, Takagi A, Mitamura K. Sensorioneural hearing loss in patients with large vestibular aqueduct. Laryngoscope. 1995; 105: 289–294.
- Ramirez-Camacho R, Ramon Garcia Berrocal J, Arellano B, Trinidad A. Familial isolated unilateral large vestibular aqueduct syndrome. ORL J Otorhinolaryngol Relat Spec. 2003; 65: 45–48.
- Griffith AJ, Arts A, Downs C, Innis JW, Shepard NT, Sheldon S, Gebarski SS. Familial large vestibular aqueduct syndrome. Laryngoscope. 1996; 106: 960–965.
- Nowak KC, Messner AH. Isolated large vestibular aqueduct syndrome in a family. Ann Otol Rhinol Laryngol. 2000; 109: 40–44.
- Lin CY, Lin SL, Kao CC, Wu JL. The remediation of hearing deterioration in children with large vestibular aqueduct syndrome. Auris Nasus Larynx. 2005; 32: 99–105.
- Wang J, Huang X, Chen H, Cheng Q. Sudden deafness with large vestibular aqueduct (case report and literatures review). Lin Chuang Er Bi Yan Hou Ke Za Zhi. 2002; 16: 515–517. (Chinese)