Laugier-Hunziker syndrome: a rare case report
Received: 02-Sep-2022, Manuscript No. puldcr-22-5440; Editor assigned: 05-Sep-2022, Pre QC No. puldcr-22-5440 (PQ); Accepted Date: Sep 24, 2022; Reviewed: 19-Sep-2022 QC No. puldcr-22-5440 (Q); Revised: 21-Sep-2022, Manuscript No. puldcr-22-5440 (R); Published: 26-Sep-2022, DOI: 10.37532. puldcr-22.6.5.16-18
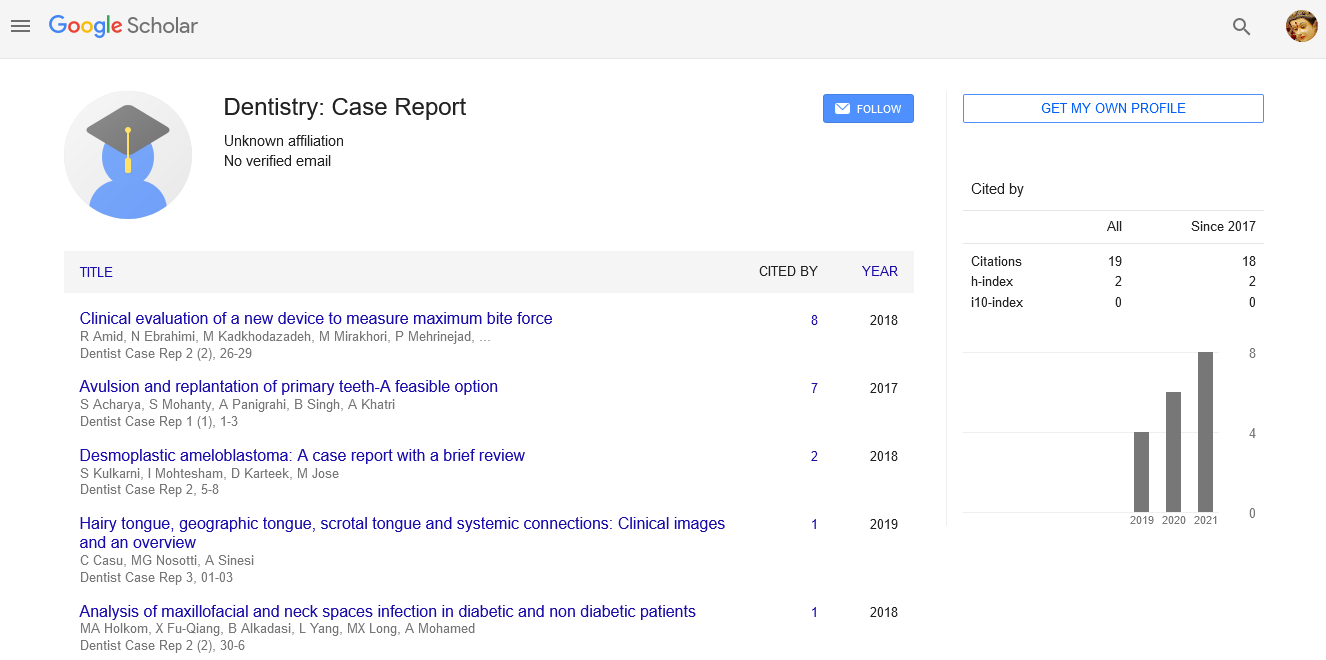
Citation: Arem S. Laugier - Hunziker syndrome: a rare case report. Dentist Case Rep. 2022;6(5):16-18.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Pigmented disorders were commonly encountered in the oral cavity, varying from a focal to diffuse presentation with the varied etiological causes ranging from the exogenous to endogenous sources. Laugier-Hunziker syndrome is a rare, hereditary pigmentary disorder characterized by mucocutaneous lentiginous lesions and melanonychia. It is regarded as a diagnosis of exclusion. Here we present a case of a 70-year female with uncommon intra and extra oral pigmentation along with the melanonychia who was diagnosed with Laugier-Hunziker syndrome. Careful examination of other disorders causing the similar pigmentation has to be carefully evaluated before arriving at a final diagnosis
Keywords
Laugier-Hunziker syndrome; primary adrenal insufficiency; oral pigmentation; longitudinal melanonychia
Introduction
Pigmentation is a darkening of the gingiva or oral mucosa that can be brought on by a variety of clinical entities ranging from physiological changes to manifestation of systemic illness and malignant neoplasms. In the oral cavity, pigmented lesions are frequently found. These lesions can range in size from a small nodular growth to a large mass, or from a focal to diffused macule. Understanding the etiology of the pigmentation and carefully evaluating the pigmented lesion is of the highest importance because pigmentation can be normal or pathological. It could be either endogenous or exogenous. Exogenous pigmentation results from the implantation of foreign bodies, whereas endogenous pigments including melanin, hemoglobin, hemosiderin, and carotene are the cause of endogenous pigmentation [1].
The most commonly encountered pigmentation in the oral cavity is melanin. Melanin is the pigment derivative of tyrosine and is synthesized by melanocytes, which typically reside in the basal cell layer of the epithelium. Melanin is thought to be cytoprotective in the skin but the role of melanin in oral mucosa is unclear. Physiological pigmentation is common in darker-skinned individuals due to the increased production of melanin by melanocytes, which can range from light brown to almost black. Pathologic melanin production within the oral mucosa may be associated with various lesions and underlying various systemic conditions [2]. In this case report, we are going to discuss one such entity Laugier and Hunziker Syndrome (LHS).
In 1970, Laugier and Hunziker reported five cases of uncommon acquired macular hyperpigmentation on the lips and oral mucosa, and two of these patients showed longitudinal pigmented streaks on the nails [3,4].
The pathogenesis is unknown, but no systemic involvement or malignant predilection has been illustrated [5]. Nails are affected in about 60% of cases, and findings include longitudinal streaks affecting the nail plate [6]. The age range of individuals affected is reported to be between the second and ninth decades, after puberty, and predominantly in middle-aged adults, with a mean onset of 50 years of age. It is more prevalent in females, and most documented cases have been in the white ethnic group, most commonly in those of French and Italian descent [7]. A biopsy of the lesions can be performed to verify the diagnosis of LHS and rule out malignancies. Histopathologic changes associated with LHS show the morphologic appearance of melanocytes and increased basal layer pigmentation with an average number [6].
Case Presentation
A 70-year-old woman was referred by her primary healthcare provider to evaluate multiple asymptomatic pigmented melanin pigmentations on the oral mucosa, hands, and face. Initially patient noticed the pigmentation five years back, there was a gradual increase in the size attained to the present size.
Although the patient had a complex medical history and extensive medication list, Non- contributory medical history, or medications causing the hyperpigmentation [Table 1]. Family, social, personal, and dental histories were unremarkable. The systemic examination doesn’t reveal any significant findings.
TABLE 1 Medical history and medication list of the patient
| Medical History: | Medications |
|---|---|
| Pigmented actinic keratosis. | Fluocinonide 0.05% |
| Glaucoma | Triamcinolone acetonide 0.1% |
| Diabetes Mellitus type II | Tretinoin 0.05% |
| Hypertension | Metformin 500mg |
| Osteoporosis | Glipizide 2.5mg |
| Anemia | Amlodipine 2.5mg |
| High cholesterol | Losartan 50mg |
| Asthma | Boniva (ibandronate) 150mg |
| Acid Reflux | Crestor (rosuvastatin) 20 mg |
| Depression | Flovent HFA 110 mcg/actuation |
| Clotrimazole 1% | |
| Pantoprazole 40mg | |
| Trazodone 100mg | |
| Ondansetron 4mg | |
| Lactobacillus acidophilus 100 million cell | |
| Sennosides 8.6mg | |
| Aspirin 81 mg |
Extraoral examination showed bilateral brown/black macules on the face Figure 1, commissures, lower lip Figure 2, and longitudinal melanonychia Figure 3.
Intraoral examination showed multiple brown/black macules on the tongue Figure 4, soft palate, the floor of the mouth Figure 5, and bilateral buccal mucosa Figure 6.
After the careful evaluation of history and the clinical examination, the differential diagnosis included metal-induced pigmentation, drug-induced hyperpigmentation, Laugier- Hunziker Syndrome (LHS), Primary adrenal insufficiency, Peutz – Jeghers Syndrome, Cushing’s disease was considered.
An incisional biopsy from the lower lip revealed a melanotic macule. There was no evidence of dysplasia or malignancy Figure 7. Referral to an endocrinologist was made; all the biochemical variables like ACTH, Cortisol, Sodium, Potassium, and androgen levels were normal. The test for 21-Hydroxylase Ab was negative [Table 2].
Figure 7: (A and B) Epithelium contains evenly distributed pigmented melanocytes in the basal layer and melanin within macrophages of the superficial lamina propria.
TABLE 2 Laboratory values.
| Ref. Range | Value | |
|---|---|---|
| ACTH, Plasma | 6 ng/L - 50 ng/L | 32 |
| Aldosterone, serum | <29 ng/dL | 17 |
| Cortisol, serum | 4 ug/dL - 19 ug/dL | 14 |
| Na | 135 mEq/L -145 mEq/L | 137 |
| K | 3.6 mmol/L - 5.2 mmol/L | 5 |
| 21-Hydroxylase Ab | NEGATIVE | NEGATIVE |
| ACTH- Adrenocorticotropic Hormone; Na- Sodium; K- Potassium; Ab- Antibodies | ||
Chest X-ray and abdominal ultrasound showed no pathological findings. A colonoscopy was performed to exclude any gastrointestinal disease associated with oral hyperpigmentation. Findings were negative for any tumorous formations in the distal and proximal regions of the colon.
Clinical and histological features confirmed the diagnosis as LaugierHunziker syndrome.
Discussion
Pigmented lesions in the oral cavity were normally encountered and routinely seen in clinical practice. It is to ascertain whether this pigmentation is physiological or pathological. Quantity, depth, or location of the pigment influences the manifestation of the color of the pigment. It may vary from brown (surface) to black or blue (deeper).
The color, location, duration, distribution, and appearance of the pigmented lesion(s) may be of diagnostic importance. A thorough family, medical, dental and social history helps to come to arrive at a diagnosis. The presence of any other signs and symptoms along with the cutaneous pigmentation may help in arriving at a differential diagnosis. Clinical laboratory testing and if needed biopsy help in ascertaining a confirmative diagnosis [8].
Physiologically melanin pigmentation appears as a multifocal or diffuse oral pigmentation. Various pathological entities may produce similar patterns such as drug-induced pigmentation, smoking-induced melanosis, hypoadrenocorticism, Cushing’s disease, Peutz-Jeghers syndrome, Laugier - Hunziker Syndrome, HIV pigmentation, biliary cirrhosis, Graves disease and Vitamin B12 deficiency [9].
Only around 172 cases of LHS have been defined; some cases have been correlated to a family member and other few cases with nonclassical features or atypical oral and skin presentations [10]. But in our case, there is no significant familial history.
LHS is primarily considered as there were multiple asymptomatic pigmented melanin pigmentations on the oral mucosa, hands, and face along with the longitudinal melanonychia.
Metal-induced pigmentation is also ruled out as the metal crowns were placed at an early age but the onset of pigmentation was five years back. If the pigment is induced by the metal, intraoral lesions appear relatively early and have relatively very less chances for extraoral site involvement and melanonychia.
As the patient was on multi drugs, drug-induced pigmentation may be considered the differential diagnosis. But after a thorough evaluation of the medications, there was no significant contribution by any drug to induce the hyperpigmentation. So, this was also ruled out.
Primary Adrenal Insufficiency (PAI) is a rare disorder and potentially lethal if unnoticed, with a prevalence of 1 in 8,000 people [11]. The diagnosis of adrenal insufficiency is made by revealing low basal or stimulated serum cortisol and should be followed by appropriate investigations to establish the underlying etiology [12]. 90% of people with primary adrenal failure come with skin pigmentation at the elbows, lips, and gingiva [11]. It is marked by the destruction of the adrenal cortex, most often of autoimmune origin, resulting in glucocorticoid, mineralocorticoid, and adrenal androgen lacks. Initial signs and symptoms can be non-specific, contributing to late diagnosis [13]. The adrenal gland is regulated by the pituitary gland by a feedback mechanism. As the steroid levels decrease, it stimulated the production of adrenocorticotropic hormone (ACTH). ACTH then acts on the adrenal cortex to stimulate corticosteroid production. The alphamelanocyte-stimulating hormone (α-MSH) gene is an alternatively spliced gene originating from the same host gene that harbors ACTH. Thus, as serum ACTH levels rise, there is a concomitant increase in α-MSH secretion. In addition to its many functions, α-MSH is thought to directly stimulate melanocytes. This induces the cells to increase melanin production [2].
Diagnosis of PAI is established by unequivocally low morning serum cortisol/aldosterone and elevated ACTH and renin concentrations. Endocrinologist evaluation reveals no significant abnormalities in the estimated parameters like ACTH, cortisol, and 21-Hydroxylase Ab was negative, so this was ruled out.
Peutz-Jeghers syndrome is a rare genetic disease associated with germline mutations in the STK11/LKB1 tumor suppressor gene that commonly occurs in young children and adolescents [14,15]. This autosomal dominant disorder is characterized by intestinal polyposis along with diffuse pigmentation over the labial and acral surfaces mimicking freckling. As such in our case, there are no abdominal complaints, an elderly presentation, ultrasound, and colonoscopic findings were negative, but it was ruled out.
Conclusion
Cushing disease may present with diffuse melanin pigmentation is the primary manifestation that results from excessive ACTH / α-MSH secretion, increased corticosteroid levels, and likely high levels of other hormones, including growth hormone, being released from the pituitary neoplasm. But in our case ACTH and cortisol levels were normal. So, this was ruled out.
LHS is mainly a disease of exclusion and is idiopathic in nature. It is similar in our case as such there is no systemic involvement or any significant drug that causes pigmentation and also the clinical and histological features confirmed the diagnosis as Laugier-Hunziker syndrome.
This case highlights the importance of ruling out adrenal insufficiency in patients with diffuse oral hyperpigmentation and the role of Oral Medicine specialists in making the diagnosis.
References
- Kauzman A, Pavone M, Blanas N, et al. Pigmented lesions of the oral cavity: review, differential diagnosis, and case presentations. J Can Dent Assoc. 2004;70(10):682-3. [Google Scholar]
- Alawi F. Pigmented lesions of the oral cavity: an update. Dent Clin North Am. 2013;57(4):699-710. [Google Scholar] [Crossref]
- Laugier P, Hunziker N. Essential lenticular melanic pigmentation of the lip and cheek mucosa. Arch Belg Dermatol Syphiligr 1970; 26: 391-399. [Google Scholar]
- Duan N, Zhang YH, Wang WM, et al. Mystery behind labial and oral melanotic macules: Clinical, dermoscopic and pathological aspects of Laugier-Hunziker syndrome. World J Clin Cases. 2018;6(10):322. [Google Scholar] [Crossref]
- Montebugnoli L, Grelli I, Cervellati F, et al. Laugier-Hunziker Syndrome: An Uncommon Cause of Oral Pigmentation and a Review of the Literature. Int J Dent. [Google Scholar] [Crossref]
- Mahmood T, Menter A. The Laugier-Hunziker syndrome. Proc Bayl Univ Med Cent. 2015;28(1):41-42. [Google Scholar] [Crossref]
- Nayak RS, Kotrashetti VS, Hosmani JV. Laugierâ??Hunziker syndrome. J Oral Maxillofac Pathol. 2012;16(2):245-250. [Google Scholar] [Crossref]
- Gondak RO, da Silva-Jorge R, Jorge J, et al. Oral pigmented lesions: Clinicopathologic features and review of the literature. Med Oral Patol Oral Cir Bucal. 2012;17(6):919-24. [Google Scholar] [Crossref]
- Aguirre A, Alawi F, Tapia JL. Pigmented Lesions of the Oral Mucosa. Burket's Oral Med. 2021:139. [Google Scholar] [Crossref]
- Toedtling V, Crawford FC. Clinical and histopathological differential diagnosis of Laugier- Hunziker syndrome: An extremely rare case with unusual extensive oral hyperpigmentation. Clin Case Rep. 2020;9(1):309-313. [Google Scholar] [Crossref]
- Pazderska A, Pearce SH. Adrenal insufficiency â?? recognition and management. Clin Med (Lond). 2017;17(3):258-262. [Google Scholar] [Crossref]
- Bornstein SR, Allolio B, Arlt W, et al. Diagnosis and Treatment of Primary Adrenal Insufficiency: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(2):364-389. [Google Scholar] [Crossref]
- Younes N, Bourdeau I, Lacroix A. Latent Adrenal Insufficiency: From Concept to Diagnosis. Frontiers in Endocrinology. 2021;12. [Google Scholar] [Crossref]
- Feelders RA, Pulgar SJ, Kempel A, et al. The burden of Cushing's disease: clinical and health-related quality of life aspects. Eur J Endocrinol. 2012; 167:311â??326. [Google Scholar] [Crossref]
- Shah KR, Boland CR, Patel M, et al. Cutaneous manifestations of gastrointestinal disease: part I. J Am Acad Dermatol. 2013; 68:189â??221. [Google Scholar] [Crossref]