Left-sided inferior vena cava or transposition of inferior vena cava: A case report
2 Ceará State University, Health Sciences Center, Medical Course, Fortaleza, Brazil, Email: Bezerrahcb1452@hotmail.com
3 Department of Kidney Transplantation, Fortaleza General Hospital, Fortaleza, Brazil, Email: romerodematosesmeraldo@gmail.com
4 Ceará State University, Health Sciences Center, Medical Course, Fortaleza, Brazil, Email: ivelisereginacanitobrasil@gmail.com
Received: 27-Feb-2020 Accepted Date: Apr 20, 2020; Published: 27-Apr-2020, DOI: 10.37532/1308-4038.20.13.1
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
This is a case report of an inferior vena cava (IVC) variation found during organ recovery for transplantation. Some considerations about anatomy and embryology, based on bibliographic research data, as well as the clinical implications for surgery, especially in the area of transplantation, are also presented.
Keywords
Surgery; Inferior Vena Cava; Embriology; Anatomic variation
Introduction
In the study of anatomy, the definition of normal can be divided into an idealistic or statistical concept. According to the idealistic concept, normal is the best or best prepared to develop a function. In the statistical concept, normal is the most frequent, that is, the one that occurs in most cases and serves as a basis for anatomical description. However, in the organ systems, there are small morphological differences that do not impair function; they are called anatomical variations [1].
Variations have been reported in all systems of the human body, including the vascular system; e.g., events related to the inferior vena cava (IVC). Anatomical variations related to the normal course of the IVC have already been described in the literature, with a growing increase in reports described in imaging examinations, during endovascular procedures or laparoscopic surgeries. These variants should be differentiated from pathologies, especially lymphadenopathies, in imaging studies, since the presence of variants can hinder surgical or interventional procedures in the retroperitoneum [2].
This study reports a case of an anatomical finding verified during an abdominal organ recovery procedure. A bibliographic survey was conducted in the Scielo and PubMed databases, and anatomy and embryology textbooks were consulted.
Case Report
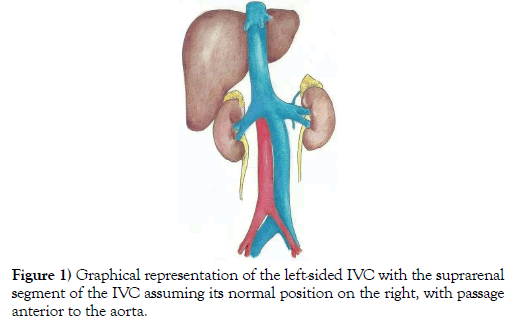
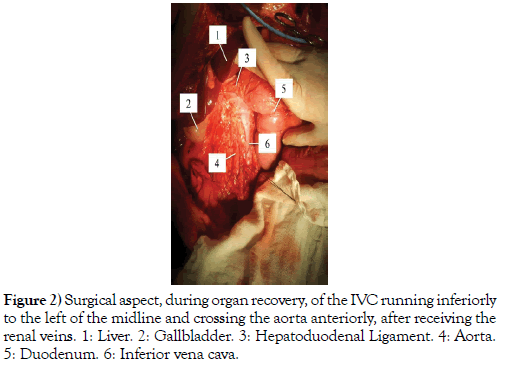
During organ recovery from a 26-year-old male multiple-organ donor, an important anatomical and surgical finding was observed: the presence of IVC with initial course to the left of the midline and, above the point of entry of the renal veins, crossing the aorta and continuing its normal path, posteriorly to the liver (Figure 1).
The common iliac veins converged at the level of the sacral promontory to form the IVC to the left of the aorta. This vessel ascended along the abdomen and curved to the right at the level of the superior mesenteric artery, forming an angle of about 150°. Its passage from left to right occurred anteriorly to the aorta and posteriorly to the duodenum, after draining the renal veins, which were normal, assuming, from there, its topography on the right, lying in the groove for vena cava in the liver (Figure 2).
Discussion
In intrauterine development, the IVC begins to form from the appearance, development, and regression of three pairs of embryonic veins: the posterior cardinal vein, the subcardinal vein, and the supracardinal vein. Initially, the embryo is drained by three pairs of veins: the vitelline veins, the umbilical veins, and the common cardinal veins. The latter are formed by the confluence of the anterior (right and left) and posterior (right and left) cardinal veins [3].
As the embryo develops, the posterior cardinal veins regress and are gradually replaced by the subcardinal and supracardinal veins. Subcardinal veins originate first and will contribute to the formation of the left renal vein, the suprarenal veins, the gonadal veins, and part of the IVC. The supracardinal veins, posteriorly, contribute to the formation of part of the azygos and hemiazygos veins, with subsequent regression of the left supracardinal vein, while the right supracardinal vein develops and becomes part of the IVC [3,4].
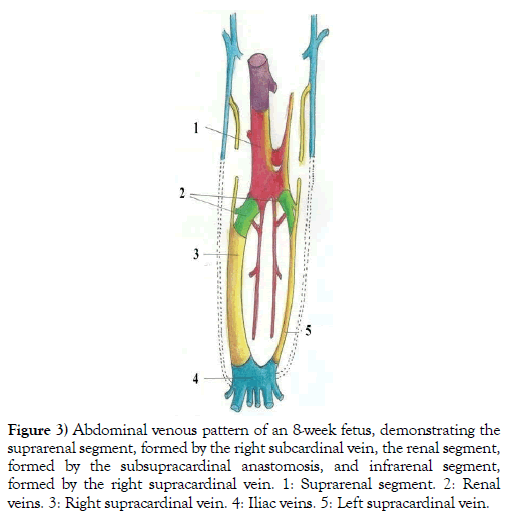
The IVC is formed, therefore, from four segments: a hepatic segment (derived from the hepatic vein, which develops from the left vitelline vein), a pre-renal segment (derived from the right subcardinal vein), a renal segment (derived from anastomoses between the subcardinal and supracardinal veins), and a post-renal segment (derived from the right supracardinal vein) (Figure 3) [4,5].
Figure 3: Abdominal venous pattern of an 8-week fetus, demonstrating the suprarenal segment, formed by the right subcardinal vein, the renal segment, formed by the subsupracardinal anastomosis, and infrarenal segment, formed by the right supracardinal vein. 1: Suprarenal segment. 2: Renal veins. 3: Right supracardinal vein. 4: Iliac veins. 5: Left supracardinal vein.
In adults, the IVC has an abdominal course that begins anteriorly to the L5 vertebra, after the union of the common iliac veins, approximately 2.5 cm to the right of the median plane. The IVC ascends, runs over the right psoas major muscle and lies to the right of the aorta. Finally, the IVC leaves the abdomen through the vena caval foramen in the diaphragm, entering the chest at the level of the T8 vertebra [6].
Left-sided IVC, or transposition of IVC, occurs when, embryologically, there is regression of the right supracardinal vein with persistence of the left supracardinal vein, which is the opposite of what normally occurs, characterizing a variant of the infrarenal segment, with IVC’s final position to the left of the midline. The prevalence of this anatomical variation in the population is about 0.2% to 0.5%. In this case, the IVC receives the left renal vein, crosses the midline to the right, drains the right renal vein, and assumes the normal course of the suprarenal IVC [5,7]. Other reported variations in the formation of the IVC, with their possible embryological origins, are:
Double Inferior Vena Cava
It results from the persistence of both supracardinal veins [5,7].
Azygos Continuation of the Inferior Vena Cava
It occurs when there is failure of formation of the right subcardinal-hepatic anastomosis, resulting in atrophy of the right subcardinal vein [7].
Double Inferior Vena Cava with Retroaortic Right Renal Vein and Hemiazygos Continuation of the Inferior Vena Cava
There is persistence of the thoracic and lumbar parts of the left supracardinal vein and left subsupracardinal anastomosis, along with failure of formation of the right subcardinal-hepatic anastomosis. Associated with this, the right renal vein and the right IVC meet and cross the aorta posteriorly to join the left-sided IVC, which continues cranially as hemiazygos vein [7].
Double Inferior Vena Cava with Retroaortic Left Renal Vein and Azygos Continuation of the Inferior Vena Cava
It results from the persistence of left supracardinal vein and dorsal arch of renal collar with regression of the ventral arch of renal collar. Associated with this, there is failure of formation of the subcardinal-hepatic anastomosis [7].
Absent Infrarenal Inferior Vena Cava with Preservation of the Suprarenal Segment
There are some reports in the literature about this variation, but there are controversies regarding the hypothesis of its embryological formation [8-10].
Conclusion
Study and knowledge of normal anatomy and its variations are essential for the success of any surgical or hemodynamic procedure, especially for transplant surgeries, as organ recovery is a dissection lesson, with the organs and their vascularization totally individualized. During kidney recovery, for example, the surgeon must properly isolate the renal vessels, identifying vascular variations, especially the multiplicity of renal arteries, so that the arteries are properly anastomosed to ensure a satisfactory perfusion of the kidney in the recipient. In liver recovery, the surgeon must pay attention to the anatomy of the portal vein, variations of the hepatic artery and of the celiac trunk, and hepatic drainage, because the variations, which are frequent, can determine the type of vascular reconstruction required for each specific case, for perfect functioning of the organ in the recipient. These vascular reconstructions are performed during organ preparation on the back table. Therefore, knowledge of the variations of the IVC will not only allow better surgical results, but will also be able to prevent inadvertent injuries with often disastrous results.
REFERENCES
- Dangelo JG, Fattini CA. Anatomia Humana Sistêmica e Segmentar. 3nd Ed., São Paulo: Atheneu. 2000;1-3.
- Brisinda G, Crocco A, Cina A, et al. Left-sided IVC in left renal cell carcinoma. Ann Ital Chir. 2013;84(1):107-10.
- Standring, S. Gray's anatomia: a base anatômica da prática clínica. 40ª Ed, Rio de Janeiro: Elsevier. 2010;1219-23.
- Moore KL, Persaud TVN. Embriologia clínica. 8nd Ed., Rio de Janeiro: Elsevier. 2008, 377-384.
- Bass FE, Redwine MD, Kramer LA, et al. Spectrum congenital anomalies of the inferior vena cava: cross-sectional imaging findings. Radiographics, 2000;20:639-52.
- Moore KL, Dalley AF. Anatomia orientada para clínica. 5nd Ed. Rio de Janeiro: Guanabara e Koogan, 2007;388-90.
- Viana SL, Mendonça JLF, Freitas FMO, et al. Anomalias congênitas da veia cava inferior: valor dos métodos multiplanares em seu diagnóstico - ensaio iconográfico. Rev Imagem. 2006;28(4):233-39.
- Gensas CS, Pires LM, Kruse ML, et al. Agenesia de veia cava inferior. Revista Brasileira de Cardiologia Invasiva, 2012;20(4):427-30.
- Alves EC, Ferro GBR, França LKL, et al. Ausência de veia cava inferior: relato de caso. J Vasc Bras, 2010;9(4):254-56.
- Fernandes AM, Rathi V, Yamrozik J, et al. Ressonância magnética cardiovascular em veia cava inferior interrompida não prevista. Arquivo Brasileiro de Cardiologia, 2012;98(2):e24-e27.