Living with stoma - A phenomenological study
2 Surgical Nursing Department, Dokuz Eylul University, Izmir, Turkey, Email: vural@yahoo.com
Received: 07-Nov-2017 Accepted Date: Nov 08, 2017; Published: 17-Nov-2017
Citation: Ceylan H, Vural F. Living with stoma - A phenomenological study. J Nurs Res Pract. 2017;1(1): 06-12.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Aim: It is to understand the experiences of patients with stoma.
Design: Descriptive study was carried out by using a phenomenologic design.
Settings: 19 patients having a stoma for at least 3 months selected via purposeful sampling method constituted the research sample. Data were collected with “in-depth interview method” by using the “unstructured interview form”. Data were analyzed with the content analysis method.
Patients: One of the investigators interviewed face to face with the 19 patients who admitted to stoma therapy unit and urology service of an university hospital between April and December 2012.
Results: Three themes were determined. These themes are; first encounter, challenges and coping. The first encounter theme consists of shock, embarrassment and feeling despair subthemes. Challenges theme consists of four subthemes which are difficulty in daily activities, difficulty in maintaining sex-life, social isolation and economic distress. Coping theme consists of five subthemes; accepting to live with stoma, failing to accept the life with stoma, looking positively, fatalism and support systems.
Conclusion: The results of the study define that stoma influences the patients significantly and it causes emotional, physical, sexual, and social changes in their lifestyles. And also, adaptation process was different in patients who had taken social and professional support. To adapt to the life with stoma, it is recommended to receive professional support beginning in the pre-operative period and continue in the post-operative period and patients who has positive/negative experiences with stoma can take social support by joining to the support groups.
Keywords
Experiences of individuals with stoma; Nursing; Qualitative
Introduction
Whatever the reason for stoma surgery is, its purpose is to elongate the survival and help the patients to return to normal and productive life. However, the problems related with stoma cause important changes in individual’s life and also isolation from the society [1-4].
The changes in physiological, psychological and social life influence the life style and quality of life of the individuals [4-7].
In literature there are many quantitative studies examining the psychological, physiological, sexual, compliance problems of the individuals with stoma at hospital and after discharging [3,8-14]. But qualitative studies are limited on evaluating the experiences of the individuals with stoma after the surgery [13,15-19]. The feelings and ideas, positive and negative conditions and the experiences about the life with stoma of the patients can only be learned with in-depth interviews. This study was conducted to understand how the lives of the patients were affected by the stoma surgery, what are the positive and negative effects of the stoma and experiences with the stoma.
Aim
The purpose of this study is to understand the experiences of the patients after the stoma surgery.
Material and Method
Study design
Phenomenological design and purposeful sampling method were used in this study.
Setting and sample
One of the investigators interviewed face to face with the 19 patients who admitted to stoma therapy unit and urology service of an university hospital between April and December 2012. Personal information form and unstructured in-depth interview form which were developed by the investigators, were used. Data were recorded with Olympus Digital Voice Recorder VN-3500PC. Interviews lasted 20 to 60 minutes. Personal information form included 18 items as; sociodemographic features, defining questions about the stoma, the duration since stoma surgery, the hospitalization duration after the surgery. The unstructured interview form was formed by the investigator to understand the physical, psychologic and social experiences of the individuals after the stoma surgery and qualitative investigations were consulted with the experts. Before the interview, investigator introduced himself/herself and gave information about the aim, pattern of the study and the voice record and written and verbal approvals were taken. Three assistant professors whom were expert about qualitative investigations were consulted the study items. If necessary the following questions were asked after the “How was your life effected after the stoma? Can you explain?” question:
• What did you feel when you see it first or after first stoma operation? How it worked?
• What were the positive experiences you faced after the operation?
• What were the negative experiences you faced after the operation?
• How it feels to live with stoma? Can you explain?
Ethical consideration
Approvals were taken from Dokuz Eylül University Non-invasive Ethics Board (date: 29.03.2012, protocol no: 535-GOA and no:2012/12-18 [App- IV]), and from the institution (date: 02.03.2012 and no:596 [App.-VI]). Investigator informed the cases having the inclusion criteria and written consents were taken.
Data analysis
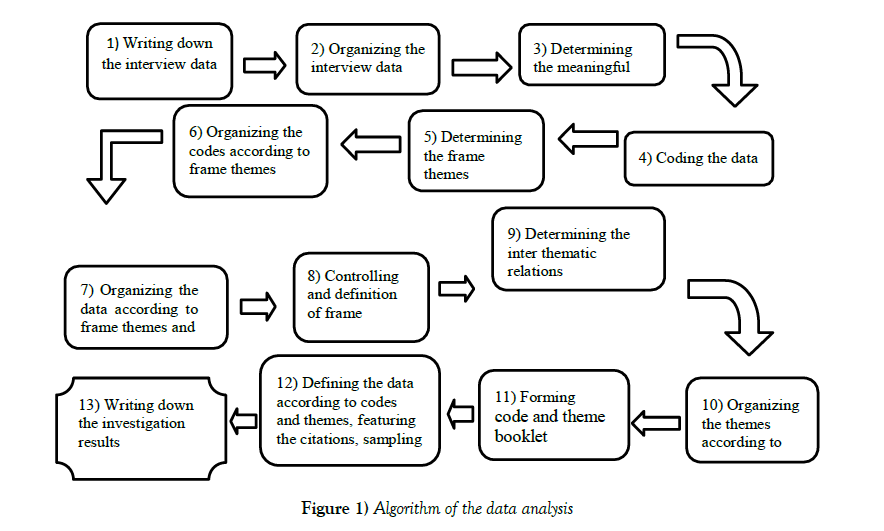
Personal information of the patients was evaluated with descriptive analysis. The interviews those were recorded with voice recorder were evaluated with content analysis. The interviewer listened and documented the data, formed them as meaningful data and coded the writings. The other investigator and a teaching staff blinded to study evaluated the writings by listening the voice record reliability [7,14,20]. Content analysis was held due to phenomenological data analysis. The algorithm of the content analysis was shown at Figure 1. Investigators red the patient expressions separately for the integrity of the meaning. As evaluating the data investigator also used the observation notes he/she wrote during the interview. Important expressions and sentences convenient for the aim of the study were determined and meanings were formed. After designing the meanings, themes were arranged. Finally data analysis was united with the individuals’ experiences. For the reliability of the study a teaching staff blinded to study also analyzed the data and results were compared. The minimal differences between the words were discussed face to face and final coding was formed. General categories were formed with acquired similar expressions and three main themes were determined. For the validity of the study, after ending the voice recording all patients were questioned whether the investigator understand their expressions correctly or not and the convenience of the meanings were confirmed [7,14,20,21].
Findings Due to Experiences of the Individuals with Stoma
Three main themes for these experiences are; first encounter, challenges and coping (Figure 2).
Theme 1. First encounter
The interviews with the patients having a stoma for at least 3 months, showed that first encounter theme comprises of 3 sub-categories. These are shock, embarrassment and despair.
A) Shock
The feeling of the patients at first encounter with the stoma is defined as shock.
“When I opened my eyes, I couldn’t look at the stoma. It was a shock for me. I didn’t look for what happened. I didn’t touch it” (5th. case, f, 78 y, colostomy)
B) Embarrassment
Individuals with stoma expressed that they are embarrassed because of stoma; beside the smell, gas, and influence in the physical image, solely the existence of the stoma is a shame for them.
“…. No one knows… (pause) I’ll never talk about it. I didn’t tell anybody except my family.” (1st. case, f, 52 y, colostomy)
“I avoid swimming in order to hide it from the others. I’m embarrassed. (15th. case, m, 82 y, colostomy)
C) Feeling despair
Individuals with stoma expressed that they don’t know what to do about the stoma care and with the extra burden due to it and sometimes they feel so desperate and think to suicide.
“I was almost going to do it. I mean I thought about suicide (3rd case., 50 y, colostomy).
“If it explodes, what can I do…..desperation” (4th case., m, 66 y, colostomy)
Theme 2. Challenges
The challenges the individuals with stoma had to deal with after the stoma operation had subthemes as; difficulties in daily activities, difficulties in sex-life, social isolation and economic distress.
A) Difficulty in daily activities
This category has some subcategories as; difficulty in physical exercises, shortage of social activities, sleep disorder, restriction in diet attitudes and trouble in religious practice.
a) Difficulty in physical activity
After the stoma operation individuals denoted that they have restriction in physical activities and their daily activities were decreased.
“Laying and standing up were so difficult after the stoma operation” (5th case, f, 78 y, colostomy)
Also one of the cases denoted that he had troubles in restricting the physical activity like difficulty in weight lifting.
“For example I want to buy vegetables and fruits in bazaar but over a certain weight it is difficult to carry them. You cannot carry them.” (13th case, m, 46 y, ileostomy)
b) Sleep disorder
They stated that they cannot sleep deeply and have to wake up frequently because they afraid of loosening of the appliance and getting the bed dirty.
“I did not have sleep. You cannot sleep. It has such negative things” (12th case, f, 64 y, colostomy)
“I have sleep disorder” (16th case, f, 60 y, colostomy)
d) Difficulty in religious practice
After the stoma operation individuals had difficulties in religious practices. They were reluctant to go to mosque because they afraid that the bag can be explode and they have difficulty in performing prayer because they have difficulty in bending and standing.
“Mosque is troublesome. I’m not going to mosque anymore. I was used to go. What mosque with this? How can you go with this? This explodes there.” (4th case, m, 66 y, colostomy)
“How it is now. I pray on a chair without ruku.” (15th case, m, 82 y, colostomy)
B) Difficulty in maintaining sex life
Individuals wits stoma expressed that they have sexual problems, and they avoid from sexual relationship because they afraid of smell and gas and appearance of the stoma.
“We cannot have sexual intercourse approximately for 4 months, my husband is so complaintive about this.” (3rd case, f, 50 y, colostomy)
“There isn’t any intercourse since my operation. No erection. My wife do not want sexual relation. She wants to divorce. Does not want to live with me.”(17th case, m, 66 y, urostomy)
Also individuals with stoma expressed that they don’t have any sexual relationship because they afraid that their partners can damage the stoma.
“Our sex life has ended. In fact, no intimacy. No intimacy because it can smell, or cause gas. My wife is affected too. Our intercourse frequency is so low. I think my wife escapes because she afraid of damaging the bag.” (6th case, m, 43 y, colostomy)
C) Social isolation
Individuals with stoma dictated that they could not maintain social activities because of the existence of stoma. Also they have to look for a toilet everywhere they can go and carry all the material necessary for nurturing.
“I cannot join the community. This is my greatest problem. We used to meet in certain days but now I can’t join.” (4th case, m, 66 y, colostomy)
“I cannot swim either. Normally I like to swim so much. But sometimes this condition annoys me. (8th case, f, 49 y, colostomy)
Before stoma operation individuals could get ready in a few minutes but postoperatively this duration was elongated.
“You have to carry the things you don’t need in normal life. You have to take some materials with you when going somewhere. Maybe it will be easier to accept this condition without these materials.”(8th case, f, 49 y, colostomy)
D) Economical distress
One individuals with stoma expressed that he was in financial shortage because of stoma material shopping and that his life was influenced.
“Also there is financial trouble. Bag quantity is insufficient, I buy extra bags, I pay extra money because my health insurance does not cover all. My retirement salary is insufficient.” (17th case, m, 66 y, urostomy)
Theme 3. Coping
Sub-categories of coping with stoma are; accepting the life with stoma, failing to accept the life with stoma, looking positively, fatalism and support systems.
A) Accepting the life with stoma
Individuals with stoma stated that they accepted the stoma although postoperatively they had negative feelings for a short time.
“It didn’t effect a bit. I’m so positive. Even still I forget it. (When I saw first) I was not affected.
I wasn’t demoralized.” (2nd case, f, 62 y, colostomy)
“Nothing changed in my life with operation, neither before nor after it......I have no complaints……” (5th case, f, 78 y, colostomy)
B) Failing to accept the life with stoma
The individuals with stoma directly expressed that they don’t accept the stoma and also used nick names for it which shows that they don’t accept it.
“Ayse (stoma) never upsets me. I diaper it… I don’t care. I wander with Ayse…… Ayse never upsets me.” (2nd case, f, 62 years, colostomy)
“I didn’t touch it. Still I can’t look at it.” (5th case, f, 78 y, colostomy)
C) Looking positively
Individuals with stoma stated that they don’t have difficulty in accepting the stoma because they got rid of cancer or something worse could have happen.
“It is worse to have stroke, I cannot walk or talk. I can beat this, we are old stagers. I’m positive.” (2nd case, f, 62 y, colostomy)
“I got rid of cancer, I’m pleased. Was it better if I die because of cancer?. I thank god and consent to it” (19th case, m, 58 y, urostomy)
D) Fatalism
Individuals with stoma thought that it is from God and in their destiny, and accepted it.
“It happened. Fate…You’ll die once not more..” (4th case, m, 66 y, colostomy)
“I said that God gave it to me, I accepted it and then I became comfortable.” (17th case, m, 66 y, urostomy)
E) Support systems
a) Social support
Individuals with stoma expressed that family and friends are very important to cope with and take care of the stoma.
“My daughter was there too. She said; mommy you can do and learn.” (2nd case, f, 62 y, colostomy)
“My family supported me very much.”(7th case, f, 54 y, ileostomy)
They also indicated that psychologically, and for maintaining the physical activities the important ones are significant supports.
“Morale is the most important thing in my wellbeing, also my wife supported me very much. We do everything together.” (14th case, m, 72 y, ileostomy)
b) Professional support
In accepting the stoma, the support of health professionals had very positive influence and the support of stomatherapy nurse and doctor were extremely beneficial for the individuals with stoma.
“I want to thank to Nurse D. (stomatherapy nurse). I gather strength with her support. I used to it after her support.” (3rd case, f, 50 y, colostomy)
“When I have problem with stoma, I always come to nurse D. Her existence is really a support.”(8th case, f, 49 y, colostomy)
In addition, during the interviews individuals learned that there are other people having the same problem and this provided a support for them.
“When you talked with me and gave information, I realized that there are many individuals with stoma in the world. This made me feel comfortable.” (15th case, m, 82 years, colostomy)
Discussion
Theme 1. First Encounter
A) Shock
In literature it was stated that patients feel sorry and frequently can percept the stoma as a disability when they see it for the first time. Also, the individuals can be shocked, and have the feelings of loss, hate, shame, and disgusting [5,9,22,23]. Our study showed that even if they informed about stoma before the operation, they had an emotional shock when they awaked and see the stoma in the recovery room after the operation. The qualitative study of Persson and Hellström 36 showed that even teaching before the operation cannot prepare them emotionally for the first encounter with the stoma. First encounter with the stoma is a hard period for the individual and even informing before the operation cannot sufficiently prepare them to see the stoma. This can be explained by the necessity of emotional preparation beside the physical preparation for the first encounter with the stoma.
B) Embarrassment
Similar with our results, the other studies showed that individuals are ashamed of having stoma and tried to hide it [9,10]. The individuals with stoma didn’t want to talk about stoma with the others and share it only with their families because of this shame. Some of them even didn’t tell it to their children because they afraid that the children will be disgusted of the smell. Stoma can be filled with uncontrolled farting and defecation and becomes visible from outside so, individuals are reluctant to socialize and don’t use public transportation [19]. Their shame can be explained with the problems due to smell and gas and with this dishonorable condition.
C) Feeling despair
Previous studies showed that individuals can deny, be afraid, be angry, resentful, be anxious, feel grief and hostility because of the stoma and also, they feel desperate [5,24]. Our study cases declared that they don’t know what to do because of the extra and recondite burden of the stoma and feel desperate.
These feelings of the patients can be explained with the new condition they have to face and multiple negative feelings they have to cope with.
Similar with our results, previous studies in the literature found that appearance, care burden and physical problems due to stoma cause them to afraid [24,25]. Serious psycho-social problems the individuals face with beside the fear can be linked with support lack.
Similar with our results, literature showed that psycho-social problems like anxiety, social-phobia, depression and major depression and even suicidal thoughts can be seen after the stoma operation [1,26]. We have to emphasize that although the stoma aims to lengthen the survival, individual prefers to die instead of living with stoma because of the problems due to it. Individuals must be supported emotionally before and after the operation in order to comply with the stoma. It is necessary to be alerted for the psychosocial problems of the individuals with stoma and determine them in the early period.
Theme 2. Challenges
A) Difficulties in daily activities
a) Difficulty in physical movement
Similar with the previous studies, we determined that patients limited the physical movements because of pain and fear of damaging the stoma [1,23,27,28]. They can feel limited because they have difficulty in lying and standing, cannot stay in sitting position continuously and afraid of explosion of the bag. This condition causes them to feel limited and have difficulty in daily activities.
In this context, to maintain their daily activities and raise their quality of life it is important to inform them about the physical activities after the stoma and what they can or cannot do.
a) Sleeping disorder
In a qualitative study, similar with our results, individuals were anxious that the stoma can leak and could not sleep deeply because it bothers them. 43 Patients cannot fell into sleep because they afraid of the explosion of the stoma.
We found that they have to wake up frequently, hesitate to turn in the bed and even stay awake till morning because they don’t want to contaminate the bed. They have to cope with many negative conditions in addition to stoma and this insomnia prevents them from living healthy.
Similar with the previous study results, our study cases avoid sleeping with their partners beside the fear of bag explosion; and these effected their relationship with their partners [11,29,30]. The social support need and bad relations with their spouses may have negative influences on their lives. Because of this, spouses must attend to the teachings of the patients for stoma compliance.
b) Restriction of diet
Our results showed that patients have trouble in diet and have nutrition disorder because they restrict the diet content. Similar with the literature they have trouble in food selection, have to change their attitudes to avoid from gas, bag inflation and explosion [31,32]. It may be due to insufficient information about the diet. They must know that only some food can cause gas and smell, stoma does not change their digestive system and they must avoid eating the food those cause problem for them [33,34,35].
c) Difficulties in religious practice
Dabirian, et al. [11] indicated group stated that they don’t as clean and valuable as the ones going to mosque and the others have no difference in their beliefs or ideas but just pray. In our study patients had trouble in religious practice because they cannot ruku or kowtow. The other trouble was the fear of explosion and smell of the bag which prevents them from going to the mosque.
It must be explained that restriction of the religious practices due to these reasons is not a sin according to Islam. Individual can perform slat on the chair by sitting and he/she must not feel bothered because it is not prejudicial according to Islam. Also they can empty the bag before going to mosque, prefer mono-bag system and use deodorizer and filters to go to the mosque with a clear conscience.
B) Difficulty in maintaining sex-life
Our study showed that individual find her/his self-dirty, repulsive and insufficient for sex-life because they are not attractive any more.
These troubles can be connected to the appearance of the stoma during sexual relationship, smell and noise of the stoma, fear of loosening and injury of the stoma and decreased libido.
In a previous study [27] like our results patients thought that their body is changed when compared with their preoperative body and avoid from sexual relations because they think they are not attractive anymore. The sexuality of the individuals with stoma was affected negatively because they find themselves less attractive and do not share this feeling with their partners.
As in a qualitative study [32] we found that individuals with stoma prefer to determine the relation according to their partner’s approach to the stoma because they abstain from the others’ reactions. The individuals with positive spouse support do not have trouble so, spouses must be informed and they must support the individuals with stoma.
It is thought that the sexual disfunction in three urostomy patients is due to surgical operation. This condition causes them to feel as they loss their manhood and negatively affected the relation with their partners. The male cases in Zmijewski’s study 52 had erectile dysfunction and retrograde ejaculation as in our study. Beside the negative feelings about sex, they had problems due to surgery. Because of this male patients must be referred to urology outpatient clinic postoperatively, to share their concerns about sexuality.
C) Social isolation
Our study patients faced with social isolation because of smell, leak, gas, embarrassment after the stoma operation like the previous studies. Patients have social problems after the ostomy surgery and they avoid from; some daily activities, sports, meeting with friends, going to the movie, becoming acquainted with new friends.
Almost all of them felt sorry when they are out, avoided to be in social environments with their friends, gave up to go holiday and swimming. It is important to realize that they waived from serious social attitudes like swimming or going to a holiday. They must be informed and encouraged about this issue. Nurses must support the patients to continue the social activities because giving up these social events leads to more serious problems [11,23,31].
D) Economical distress
Beside that they cannot go to work, they stay in hospital for a long time and necessary materials are expensive and all these causes economical shortage [9,11,28,31].
In our study group females were house wives and majority of the males were retired or bosses that they did not have economical problem due to work. However one patient expressed that he had economical shortage after the stoma and his family life was influenced negatively. In our country health insurance covers a limited part of the materials and especially after the operation in the early period patients have to buy the materials themselves and this leads to economic distress. One case in our study told that he had financial problem because he had to change the leaking bag so frequent. This shows that patient can need more bags and adapters because of stoma problems (fistula, retraction etc.) and there can be shortage of material [31].
Theme 2. Coping
Accepting to live with stoma
As in previous studies, we found that patients accept the stoma more easily if they have the following factors; patients with crohn disease or ulcerative colitis get rid of diarrhea attacks and cancer patients relieved from cancer. If they see the stoma as a salvation from a worse condition they accept the stoma more easily [28,36].
The negative feelings were disappeared quickly with social and professional support. Patients accept the stoma as a bridge to life and a chance for survival and the strength of family relations and physical and psycho-social supports of them are very important factors in Turkish population for this acceptation.
Similar with a previous study, our study showed that if patients are informed and operation field is signed before the operation they do not influenced by the operation and do not have negative feelings when they see it and do not need to hide it [8,15]. It is thought that informing the patient clearly about the purpose and location of the stoma will be beneficial for the compliance process.
A) Failing to accept the life with stoma
Studies found that not accepting the stoma is affected with following factors; body image change, thinking that she/he is not normal and cannot have a normal life anymore, and feeling useless [30,37,38]. Also, patients in our study who felt insufficiency were hardly accepted the stoma. The situation must be discussed with the patient not accepting herself/himself as normal and they must be helped for compliance [18].
However, some individuals whom expressed that they have accepted the stoma, used nick names for the stoma which is a sign of unacceptance. Even if they expressed compliance it may not be true. Because of this, nurse must observe their behavior’s closely. During compliance period patients can use ineffective defense mechanisms and these preventions can be beneficial. However, in long-term, patient must learn to live with stoma and develop technical skills for stoma Care [36,15].
B) Looking positively
As in a previous qualitative study, our patients also accepted the stoma as a bridge to life [28].
In our study most of the cases took it from the positive side and thought they get rid of a worse condition so, accepted the stoma more easily. They were happy not being in a worse condition like stroke. Also the patients with cancer accepted the stoma as salvation and survival chance, and do not have difficulty in coping with it.
For the patients preferring to be consoled with thinking worse conditions, positivity is an effective coping method. However, it is important to realize whether if the patient accommodate to this new condition and percept himself/herself normal or not. Nurse must question this issue and support the patients.
C) Fatalism
We thought that as in a qualitative study, because all of our cases were Muslim and believe in God, they did not have any difference in their lives after the stoma. 15 Patients come round to stoma as coming from God, and as fate so they think that denying the stoma is a rebel and refusing the fate. The patients using belief for coping, didn’t have any difficulty in accepting the stoma. It must be remembered that religious beliefs and ideas are very important to facilitate their lives with stoma.
D) Support Systems
a) Social Support
Similar with our results a qualitative study found that stoma assumption duration is shorter in the patients whom were supported physically and psychologically by their families and friends [32]. Also, we found that family and friends are very important in getting used to the life with stoma. Family has an important role in caring the stoma and an important support in maintaining the psychological and physical activities. If their social environment see the stoma as a problem patients prefer to hide it and change their clothes in the dark.
The patients without positive social support accept the stoma hardly and have more negative feelings [9,23,28,31,39]. Because of this, family must be informed about the stoma preoperatively. Studies showed that positive social support helps patients to accept the new condition easily [9,28,31].
b) Professional Support
Like our results, previous studies found that support of health professionals is very important in accepting the stoma and accommodating to the new life. Informing the patients about the stoma and life with stoma before the operation decreases the negative feelings and fears about the operation and its results, and increases the compliance [3,23,37]. Especially informing them about the necessity of stoma and giving details for the postoperative life by doctor; and stoma teaching and psychosocial support by the nurse have significant importance for patients. Beside the social support, professional support helps them to feel more secure and facilitates the compliance [40-53].
Results
Different from other studies we investigated the experiences of the individuals with stoma and found that there were great differences in their lives after the stoma. Our results showed that patients have been affected significantly and had differences in emotional, physical, sexual and social parts of her/his life. There were patients whom prefer to die instead of having stoma. Not getting supervision and support, except stoma care, and can’t expressing themselves psychosocially and sexually influenced their lives negatively. The individuals with stoma with social and professional support had positive experiences when compared with the negative experiences of the ones without any support during the compliance period. Also, patients stated that their compliance will be facilitated if they take social and professional support.
Trustworties
As a result, if we want the individuals with stoma be in compliance with stoma;
• Patients must be informed about the life with stoma before the operation and must be supported in the post-operative period,
• Patients must take private physical, psychosocial and sexual consultancy in postoperative period,
• It is recommended to form support groups for individuals with stoma to discuss, share their positive/negative experiences after the operation and help them to take part in a group,
• Also it is recommended to held qualitative studies examining the physical, spiritual, social and sexual experiences of the individuals with stoma separately.
Source of Funding
yy This study was presented as an oral proceeding in two congresses, Fourteenth National Colon and Rectum Surgery Congress, Seventh Congress of Nursing in Colorectal Surgery in Antalya, Turkey, on 15-19 May, 2013 and Twelfth European Council of Enterostomal Therapy Congress in Paris, France, on 23-26 June 2013.
• This study was funded by investigator.
• This study was a master thesis at Dokuz Eylul University Health Sciences Intitute Department of Nursing (Surgical Diseases Nursing) in 2012.
Ethics Committee Approval
Ethics committee approval was received for this study from the Dokuz Eylül University Non-invasive Ethics Board (date: 29.03.2012, protocol no:535- GOA and no:2012/12-18 [App-IV].
Informed Consent
Written informed consent was obtained from all patients who participated in this study.
REFERENCES
- Liu L, Herrinton JL, Hornbrook CM, et al. Early and Late complications among long-term colorectal cancer survivors with ostomy or anastomosis. Dis Colon Rectum. 2010;53(2):200-12.
- Holzer B, Matzel K, Schiedeck T, et al. Do geographic and educational factors influence the quality of life in rectal cancer patients with a permanent colostomy? Dis Colon Rectum. 2005;48:2209-16.
- Dorum H, Vural F. Stomada Cinsellik Neden Önemlidir? DEUHYO ED. 2012;5(4):171-4.
- Goldberg M, Aukett KL, Carmel J, et al. Management of the patient with a fecal ostomy. Best Practice Guideline For Clinicians. J Wound Ostomy Continence Nur. 2010;37(6):596-8.
- Baldwin C, Grant M, Wendel C, et al. Influence of intestinal stoma on spiritual quality of life of U.S. veterans. J Holistic Nur. 2008;26,185-94.
- Ayaz S, Kubilay G. Effectiveness of the PLISSIT model for solving the sexual problems of patients with stoma. J Clin Nur. 2008;18:89-90.
- Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory into Practice, 2000;39(3):124-131.
- Haboubi NHJ, Lincoln N. Views of health professionals on discussing sexual issues with patients. Disability and Rehabilitation. 2003;25(6):291-6.
- Gulbiniene J, Markelis R, Tameli A, et al. The impact of preoperative stoma siting and stoma care education on patient’s quality of life. Medicana (Kaunas, Lithuania). 2004;40(11):1045-53.
- Grant M, McMullen KC, Altschuler A, et al. Gender differences in quality of life among long- term colorectal cancer survivors with ostomies. Oncology Nurs Forum. 2011;38(5):587-96.
- Dabirian A, Yaghmaei F, Rassouli M, et al. Quality of life ostomy patients: A qualitative study. Patient Preference and Adherence. 2011;5:1-5.
- Brown H, Randle J. Living with stoma: a review of literature. J Clin Nurs. 2005;14:78-84.
- Colwell JC, Beitz J. Survey of wound, ostomy and continence (WOC) nurse clinicians on stomal and peristomal complications: A content validation study. J Wound, Ostomy and Continence Nur. 2007;34(1):57-69.
- Mitchell AK, Rawl MS, Schmidt MC, et al. Demographic, Clinical, and quality of life variables related to embarrassment in veterans living with an intestinal stoma. J Wound Ostomy Continence Nurs. 2007;34(5):524-32.
- Cengiz B, Bahar Z. Perceived Barriers and Home Care Needs When Adapting to a Fecal Ostomy. A Phenomenological Study. J Wound Ostomy Continence Nurs. 2017;44(1):63-8.
- Dazio EMR, Sanobe HM, Zago MMF. The meaning of being a man with intestinal stoma due to colorectal cancer: an anthropological approach to masculinities. Rev Latino -am Enfermagem setembro-outubro. 2009;17(5):664-9.
- Krouse RS, Grant M, Rawl SM, et al. Coping and acceptance: The greatest challenge for veterans with intesitinal stomas. J Psycomotic Res. 2009;66:227-33.
- Neuman BH, Park J, Fuzesi S. Rectal cancer patients’ quality of life with a temporary stoma: shifting perspectives. Dis Colon Rectum. 2012;55:1117-24.
- Pachler J, Wille-Jorgensen P. Quality of life after rectal resection for cancer with or without permanent colostomy. Cochrane Database Systematic Rewiev. 2005;18(2):CD004323.
- Aksayan S, Bahar Z, Bayik A, et al. Research Principle Processes and Methods in Nursing. 2002.
- Strauss A, Corbin J. Basics of qualitative research: Grounded theory procedures and techniques. Newbury Park, CA: Sage Publications, Inc. 1990.
- Vujnovich A. Pre and post-operative assessment of patients with a stoma. Nursing Standard. 2008;22(19):50-6.
- Richbourgh L, Thorpe MJ, Rapp GC. Diffuculties experienced by the ostomate after hospital discharge. J Wound Ostomy Continence Nurs. 2007;34(1):70-9.
- Gordon AJ. Partners’ experience of living with a person who has undergone colostomy or ileostomy surgery: a phenomenological study. University of New Brunswick, Master Thesis. 2009.
- Harputlu D, Terzi C, Eşrefgil G, et al. Kolostomi ve ileostomili bireylerde benlik saygısı. Kolon Rektum Hastalığı Dergisi. 2007;17:178-85.
- Popek S, Grant M, Gemmil R, et al. Overcoming challenges: Life with an ostomy. J Sur. 2010;640-5.
- Pittman J, Rawl SM, Schmidt CM, et al. Demographic and clinical factors related to ostomy complications and quality of life in veterans with an ostomy. J Wound Ostomy Continence Nur. 2008;35(5):493-503.
- Andersson G, Engström Å, Söderberg S. A chance to live: Women’s experiences of living with a colostomy after rectal cancer surgery. Inter J Nur Prac. 2010;16:603-08.
- Shaffy S, Kaur S, Das K, et al. Physical, nutritional and sexual problems experienced by the patients with colostomy/ileostomy: A qualitative study. Nur Midwifery Res J. 2012;8(3).
- Robertson I, Leung E, Hughes D, et al. Prospective analysis of stoma-related complications. Colorectal Dis. 2005;7:279-85.
- Lincoln SY, Guba GE. Naturalistic Inquiry. 1985.
- Yaşan A, Ünal S, Gedik E, et al. Kalıcı ve geçici ostomi yapılmış kişilerde yaşam kalitesinde değişim, depresyon ve anksiyete. Anadolu Psikiyatri Dergisi. 2008;9(3):162-8.
- Fullham J. Providing dietary advice for the individual with a stoma. British J Nurs. 2008;17:22-7.
- Burch J. Psychological problems and stomas: A rough guide for community nurses. British J Community Nur. 2005;10(5):224-7.
- Burch J. Nutrition and ostomate: input, output and absorption: British J Community Nur. 2006;11(8):349-51.
- Zmijewski HC. The view from here: sexual counselling by the ET nurse: if not you, then who? J Wound Ostomy Continence Nurs. 2002;29:184-5.
- Simmons LK, Smith AJ, Bobb KA, et al. Adjustment to colostomy: stoma acceptance, stoma care self-efficacy and interpersonal relationships. Blackwell Publishing Ltd. 2007.
- Albaugh JA, Kellogg-Spadt K. Sexuality and sexual health: The nurse’s role and initial approach to patients. Urologic Nur. 2003;23(3):227-8.
- Junkin J, Beitz JM. Sexuality and the person with a stoma: implications for comprehensive WOC nursing practice. J Wound Ostomy Continence Nur. 2005;32:121-8.
- Dixon KD, Dixon PN. The PLISSIT Model: Care and management of patients’ psychosexual needs following radical surgery. Lippincotts Case Managing. 2006;11:101-6.
- Altschuler A, Ramirez M, Grant M, et al. The influence of husbands’ or male partners’ support on women’s psychosocial adjustment to having an ostomy resulting from colorectal cancer. J Wound Ostomy Continence Nurs. 2009;36(3):299-305.
- Comb J. Role of the stoma care nurse: patient with cancer and colostomy. British J Nur. 2003;12(14):852-6.
- Danielsen AK, Soerensen EE. Burcharth K, et al. Lerning to Live With a Permanent Intestinal Ostomy: Impact on Everyday Life and Educational Needs. J Wound Ostomy Continence Nurs. 2013;40(4):407-12.
- Gao Y. New stoma patients’ experiences during post-operative nursing care. Jamk University of Applied Sciences, Bachelor’s Thesis, 2012.
- Persson E, Gustavsson B, Hellstrom AL, et al. Ostomy patients’ perception of quality of care. J Advanced Nursing. 2003;49(1):51-8.
- Persson E, Hellstrom AL. Experiences of swedish men and woman 6 to 12 weeks after ostomy surgery. J Wound Ostomy and Continence Nur. 2002;(29):103-8.
- Ringhofer J. Meeting the needs of your ostomy patient. 2005;68(8):37-42.
- Ross L, Abild-Nielsen AG, Thomsen BL, et al. Quality of life of danish colorectal cancer patients with and without a stoma. Support Care Cancer. 2007;15(5):505-13.
- Sohn JY, Moon MS, Shin SU, et al. Incidence and risk factors of parastomal herni. J Korean Society of Coloproctology. 2012;28(5):241-46.
- Sinclair LG. Young adults with permanent ileostomies experiences during the first 4 years after surgery. J Wound Ostomy Continence Nur Society. 2009;36(3)306-16.
- Vural F, Sütsünbüloğlu E, Şelimen D. Literatür İnceleme: Stomalı Bireylere Yönelik Yayınların Türkiye Profili. Turk J Colorectal Dis. 2016;26:59-70.
- Yıldırım A, Şimşek H. Sosyal Bilimlerde Nitel Araştırma Yöntemleri. Ankara: Seçkin Yayıncılık. 2005.
- Dylan SM, Loewenstein G, Rozin P, et al. Sensitivity to disgust, stigma, and adjustment to life with a colostomy. J Res Pers. 2007;41(4):787-803.