Long head of triceps supplied by axillary nerve
Komala Nanjundaiah*,Shashanka MallasandraJayadevaiah and SheshgiriChowdapurkar
Department of Anatomy, M. S. Ramaiah Medical College, Bangalore, India.
- *Corresponding Author:
- Dr. Komala N
Assistant Professor, Department of Anatomy, M. S. Ramaiah Medical College, Msrit Post Bangalore, 560054, India
Tel: +91 (80) 23421593
E-mail: komalananjundaiah@gmail.com
Date of Received: June 23rd, 2011
Date of Accepted: April 16th, 2012
Published Online: September 20th, 2012
© Int J Anat Var (IJAV). 2012; 5: 35–37.
[ft_below_content] =>Keywords
axillary nerve,radial nerve,triceps
Introduction
The axillary nerve comes from the posterior cord of the brachial plexus at the level of the axilla and carries nerve fibers from C5 and C6. The axillary nerve travels through the quadrangular space with the posterior circumflex humeral vessels, and divides into anterior and posterior branches. It supplies deltoid and teres minor. It carries sensory information from the shoulder joint, as well as the skin covering the inferior region of the deltoid muscle – the “regimental badge” area [1].
The radial nerve (C5–T1) is the largest branch of brachial plexus and is the continuation of the posterior cord. It is a nerve of extensor compartments of the arm and forearm. It passes through lower triangular space and spiral groove and pierces the intermuscular septum of arm, to enter into front of the arm and finally divides into superficial and deep branches in front of the elbow joint. It supplies all the 3 heads of triceps brachii muscle by separate branches to each of the head [1].
Most of the anatomy textbooks say that the motor branch of the long head of the triceps brachii arises from the radial nerve, but some cadaveric studies have shown that the triceps is innervated by the axillary nerve. Awareness of such variations is important for clinicians and surgeons.
Case Report
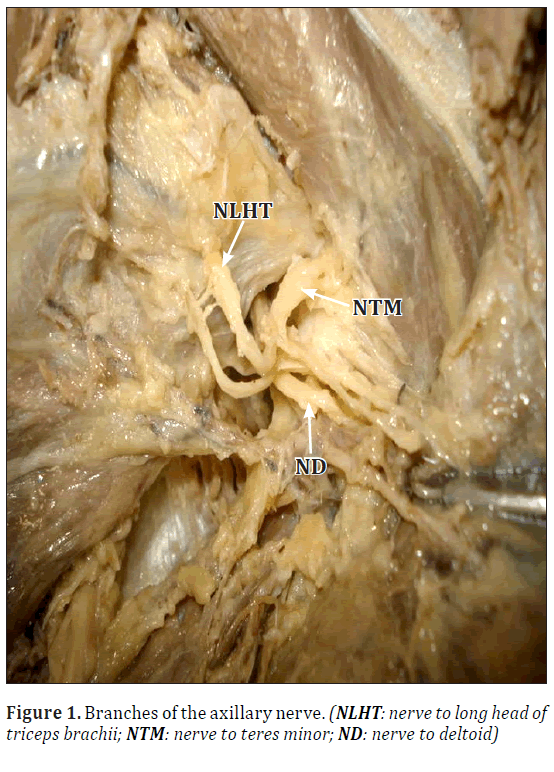
During routine dissection study and teaching to undergraduate students in Anatomy department, MSRMC, Bangalore, We found bilateral variation in the innervation to long head of triceps in an adult male cadaver aged 60–70 years. The motor branch to the long head of the triceps was arising from the axillary nerve bilaterally, instead of its usual origin from radial nerve. The axillary nerve after passing through the quadrangular space instead of bifurcating, was trifurcating into the anterior branch, the posterior branch and a branch to the long head of triceps. The other branches of both the nerves were as usual in origin and course bilaterally (Figure1).
Discussion
Morphological significance
Most of the anatomy textbooks say that the motor branch of the long head of the triceps brachii arises from the radial nerve. But the following studies show that the nerve supply to long head of triceps comes from the axillary nerve.
A retrospective clinical study of traumatic injuries of the axillary nerve with associated paralysis of the long head of triceps suggests that the motor branch of the long head of triceps may arise from the axillary nerve [2]. De Sèze et al. conducted a study to determine the exact origin of the motor branch to the long head of the triceps. The study was performed in two groups. Group 1 included the study on 10 cadavers (20 limb specimens) by anatomical dissection. Group 2 included surgical dissection of posterior cords of 15 patients suffering from C5–C6 injured paralysis, without paralysis of the long head of the triceps (Table 1). Their results suggest that the motor branch to the long head of the triceps never originated from the radial nerve.
Table 1: Origin of the motor branch to the long head of the triceps [2].
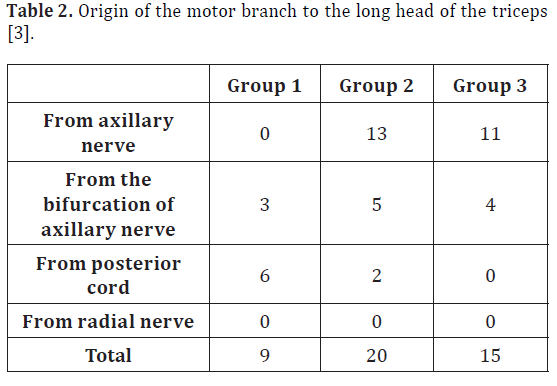
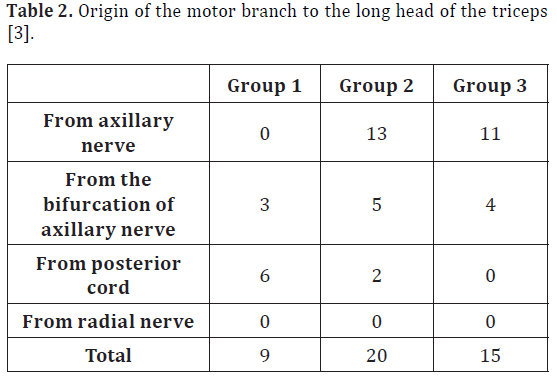
Table 2: Origin of the motor branch to the long head of the triceps [3].
Rezzouk et al. conducted a study in 3 groups. Group 1 included 9 traumatic injuries of the axillary nerve associated with clinical involvement of the long head of triceps; group 2 included 20 secondary posterior trunks dissected from cadaver specimens; group 3 included 15 dissections of infraclavicular plexus with secondary posterior trunks [3]. Their results suggest that the motor branch of the long head of the triceps never originated from the radial nerve (Table 2).
Clinical significance – Axillary neuropathy
The nerve can be injured by traction or compression from a shoulder dislocation, humeral head fracture, or improper crutch use.
Injury to the nerve results in paralysis of the teres minor muscle and deltoid muscle, resulting in loss of abduction of arm (from 15–90 degrees), flat shoulder deformity, loss of sensation in the skin over a small part of the lateral upper arm [1].
Disruption of the C5 and C6 roots results in an Erb’s palsy, with loss of supply to muscles innervated by the suprascapular nerve, axillary nerve, and musculocutaneous nerve. This type of upper brachial plexus injuries is most common root avulsion injuries. Recent developments in nerve transfer procedures promises improved results over traditional reconstructive procedures in such cases [4].
The diameter, the number of axons, and the anatomic proximity of the nerve to the long head of the triceps make it a potential source for re-innervation of the anterior branch of the axillary nerve by direct nerve transfer without nerve grafting [5].
In case of traumatic injury to axillary nerve associated palsy of long head of the triceps is a sign of severe axillary nerve lesion requiring early repair at 3 months [3].
Conclusion
Textbooks say that the motor branch to the long head of triceps arises from the radial nerve, but many cadaver studies have shown that the motor branch of long head of the triceps arise from axillary nerve. Hitchhiking of nerve fibers of brachial plexus is also one of the common variations. The present variation also could be one of this type. Hence while examining patients with traumatic injury of the axillary nerve, it is important to look for paralysis of the long head of the triceps. Awareness of such a variation is also important during infraclavicular brachial plexus block, management of axilla and shoulder repair surgeries and nerve transplant procedures.
References
- Williams PL, ed. Gray’s Anatomy. 38th Ed., ELBS Churchill Livingstone. 1995; 1269–1274.
- de Sèze MP, Rezzouk J, de Sèze M, Uzel M, Lavignolle B, Midy D, Durandeau A. Does the motor branch of the long head of triceps brachii arise from the radial nerve? An anatomic and electromyographic study. Surg Radiol Anat. 2004; 26: 459–461
- Rezzouk J, Durandeau A, Vital JM, Fabre T. Long head of the triceps brachii in axillary nerve injury: anatomy and clinical aspects. Rev Chir Orthop Reparatrice Appar Mot. 2002; 88: 561–564.
- Colbert SH, Mackinnon S. Posterior approach for double nerve transfer for restoration of shoulder function in upper brachial plexus palsy. Hand (N Y). 2006; 1: 71–77.
- Witoonchart K, Leechavengvongs S, Uerpairojkit C, Thuvasethakul P, Wongnopsuwan V. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part I: an anatomic feasibility study. J Hand Surg Am. 2003; 28: 628–632.
Komala Nanjundaiah*,Shashanka MallasandraJayadevaiah and SheshgiriChowdapurkar
Department of Anatomy, M. S. Ramaiah Medical College, Bangalore, India.
- *Corresponding Author:
- Dr. Komala N
Assistant Professor, Department of Anatomy, M. S. Ramaiah Medical College, Msrit Post Bangalore, 560054, India
Tel: +91 (80) 23421593
E-mail: komalananjundaiah@gmail.com
Date of Received: June 23rd, 2011
Date of Accepted: April 16th, 2012
Published Online: September 20th, 2012
© Int J Anat Var (IJAV). 2012; 5: 35–37.
Abstract
The axillary nerve comes from the posterior cord of the brachial plexus at the level of the axilla and carries nerve fibers from C5 and C6. It supplies deltoid and teres minor. The radial nerve (C5–T1) is the largest branch of brachial plexus and is the continuation of the posterior cord. It supplies all the 3 heads of triceps brachii muscle by separate branches to each of the head. During routine dissection study and teaching to undergraduate students, we found bilateral variation in the innervation to long head of triceps in an adult male cadaver aged 60–70 years. The motor branch to the long head of the triceps was arising from the axillary nerve bilaterally, instead of its usual origin from radial nerve. Morphological and clinical implications of the variation are discussed.
-Keywords
axillary nerve,radial nerve,triceps
Introduction
The axillary nerve comes from the posterior cord of the brachial plexus at the level of the axilla and carries nerve fibers from C5 and C6. The axillary nerve travels through the quadrangular space with the posterior circumflex humeral vessels, and divides into anterior and posterior branches. It supplies deltoid and teres minor. It carries sensory information from the shoulder joint, as well as the skin covering the inferior region of the deltoid muscle – the “regimental badge” area [1].
The radial nerve (C5–T1) is the largest branch of brachial plexus and is the continuation of the posterior cord. It is a nerve of extensor compartments of the arm and forearm. It passes through lower triangular space and spiral groove and pierces the intermuscular septum of arm, to enter into front of the arm and finally divides into superficial and deep branches in front of the elbow joint. It supplies all the 3 heads of triceps brachii muscle by separate branches to each of the head [1].
Most of the anatomy textbooks say that the motor branch of the long head of the triceps brachii arises from the radial nerve, but some cadaveric studies have shown that the triceps is innervated by the axillary nerve. Awareness of such variations is important for clinicians and surgeons.
Case Report
During routine dissection study and teaching to undergraduate students in Anatomy department, MSRMC, Bangalore, We found bilateral variation in the innervation to long head of triceps in an adult male cadaver aged 60–70 years. The motor branch to the long head of the triceps was arising from the axillary nerve bilaterally, instead of its usual origin from radial nerve. The axillary nerve after passing through the quadrangular space instead of bifurcating, was trifurcating into the anterior branch, the posterior branch and a branch to the long head of triceps. The other branches of both the nerves were as usual in origin and course bilaterally (Figure1).
Discussion
Morphological significance
Most of the anatomy textbooks say that the motor branch of the long head of the triceps brachii arises from the radial nerve. But the following studies show that the nerve supply to long head of triceps comes from the axillary nerve.
A retrospective clinical study of traumatic injuries of the axillary nerve with associated paralysis of the long head of triceps suggests that the motor branch of the long head of triceps may arise from the axillary nerve [2]. De Sèze et al. conducted a study to determine the exact origin of the motor branch to the long head of the triceps. The study was performed in two groups. Group 1 included the study on 10 cadavers (20 limb specimens) by anatomical dissection. Group 2 included surgical dissection of posterior cords of 15 patients suffering from C5–C6 injured paralysis, without paralysis of the long head of the triceps (Table 1). Their results suggest that the motor branch to the long head of the triceps never originated from the radial nerve.
Table 1: Origin of the motor branch to the long head of the triceps [2].
Table 2: Origin of the motor branch to the long head of the triceps [3].
Rezzouk et al. conducted a study in 3 groups. Group 1 included 9 traumatic injuries of the axillary nerve associated with clinical involvement of the long head of triceps; group 2 included 20 secondary posterior trunks dissected from cadaver specimens; group 3 included 15 dissections of infraclavicular plexus with secondary posterior trunks [3]. Their results suggest that the motor branch of the long head of the triceps never originated from the radial nerve (Table 2).
Clinical significance – Axillary neuropathy
The nerve can be injured by traction or compression from a shoulder dislocation, humeral head fracture, or improper crutch use.
Injury to the nerve results in paralysis of the teres minor muscle and deltoid muscle, resulting in loss of abduction of arm (from 15–90 degrees), flat shoulder deformity, loss of sensation in the skin over a small part of the lateral upper arm [1].
Disruption of the C5 and C6 roots results in an Erb’s palsy, with loss of supply to muscles innervated by the suprascapular nerve, axillary nerve, and musculocutaneous nerve. This type of upper brachial plexus injuries is most common root avulsion injuries. Recent developments in nerve transfer procedures promises improved results over traditional reconstructive procedures in such cases [4].
The diameter, the number of axons, and the anatomic proximity of the nerve to the long head of the triceps make it a potential source for re-innervation of the anterior branch of the axillary nerve by direct nerve transfer without nerve grafting [5].
In case of traumatic injury to axillary nerve associated palsy of long head of the triceps is a sign of severe axillary nerve lesion requiring early repair at 3 months [3].
Conclusion
Textbooks say that the motor branch to the long head of triceps arises from the radial nerve, but many cadaver studies have shown that the motor branch of long head of the triceps arise from axillary nerve. Hitchhiking of nerve fibers of brachial plexus is also one of the common variations. The present variation also could be one of this type. Hence while examining patients with traumatic injury of the axillary nerve, it is important to look for paralysis of the long head of the triceps. Awareness of such a variation is also important during infraclavicular brachial plexus block, management of axilla and shoulder repair surgeries and nerve transplant procedures.
References
- Williams PL, ed. Gray’s Anatomy. 38th Ed., ELBS Churchill Livingstone. 1995; 1269–1274.
- de Sèze MP, Rezzouk J, de Sèze M, Uzel M, Lavignolle B, Midy D, Durandeau A. Does the motor branch of the long head of triceps brachii arise from the radial nerve? An anatomic and electromyographic study. Surg Radiol Anat. 2004; 26: 459–461
- Rezzouk J, Durandeau A, Vital JM, Fabre T. Long head of the triceps brachii in axillary nerve injury: anatomy and clinical aspects. Rev Chir Orthop Reparatrice Appar Mot. 2002; 88: 561–564.
- Colbert SH, Mackinnon S. Posterior approach for double nerve transfer for restoration of shoulder function in upper brachial plexus palsy. Hand (N Y). 2006; 1: 71–77.
- Witoonchart K, Leechavengvongs S, Uerpairojkit C, Thuvasethakul P, Wongnopsuwan V. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part I: an anatomic feasibility study. J Hand Surg Am. 2003; 28: 628–632.