Long pouch and transit bipartition gastric bypass for endoscopic access to the remaining stomach
Received: 03-Feb-2022, Manuscript No. 22-5348; Editor assigned: 06-Feb-2022, Pre QC No. 22-5348 (PQ); Accepted Date: Feb 26, 2022; Reviewed: 18-Feb-2022 QC No. 22-5348 (Q); Revised: 24-Feb-2022, Manuscript No. 22-5348 (R); Published: 28-Feb-2022
Citation: Kuo J. Long pouch and transit bipartition gastric bypass for endoscopic access to the remaining stomach: A review article. J Surg Res. 2022; 6(1):4-6.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
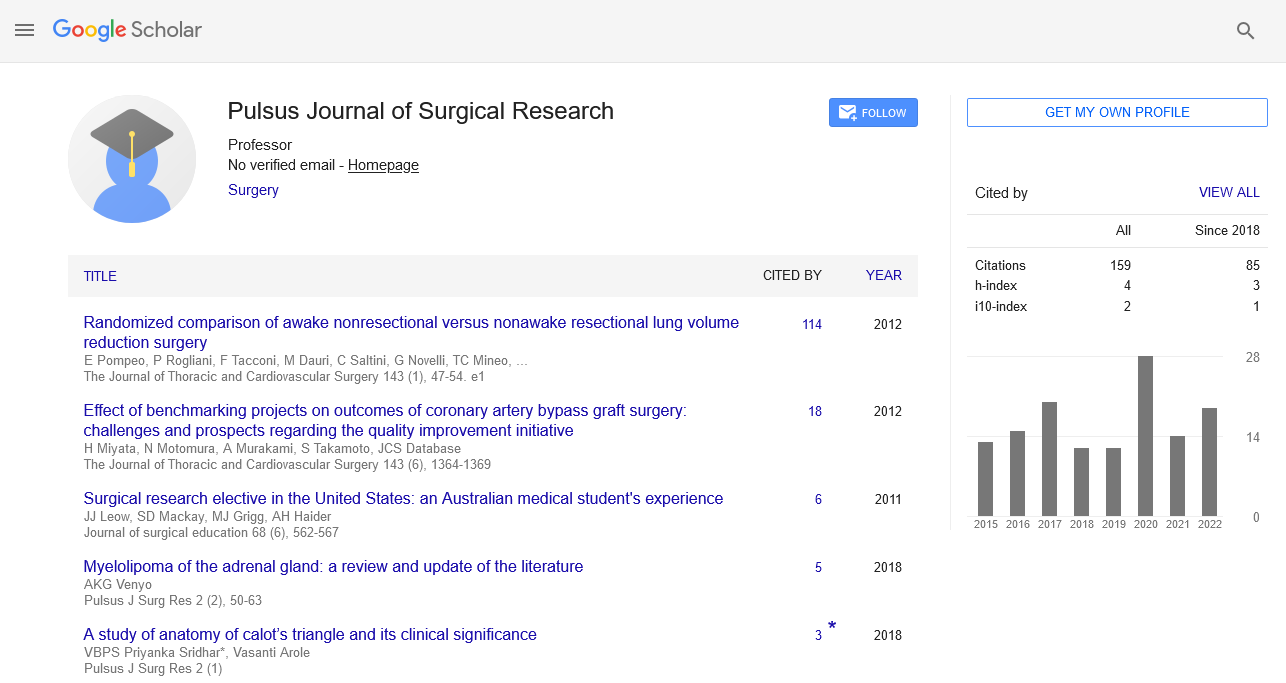
With a difficult to treat aetiology, multivariate complexity, and rising incidence rates in recent years, obesity is a complicated and multifaceted disease. Clinical, pharmacological, and surgical procedures are all part of the treatment. If those don't work, they'll be combined. One of these surgical procedures is the Roux-en-Y Gastric Bypass (RYGB), in which the stomach is cut in half, forming a tiny pouch, and the remaining stomach is excluded and denied endoscopic access to assess the outcomes of modified RYGB with extended pouch and endoscopic access to the unreconstructed stomach. Patients seen at the Alberto Rassi General State Hospital of Goiania (HGG) who were determined to be candidates for bariatric and metabolic surgery by the medical and multidisciplinary team were used as the sample population for a prospective clinical trial. The research was carried out between January 2020 and August 2021. The medical and interdisciplinary team interviewed the chosen patients to obtain their clinical histories and the results of their laboratory tests. The study has twelve participants in it. The mean age of these was 46.3 years, with 11 of them (91.7%) being female. Prior to surgery, the patient weighed 112.17 kg (92.00–150.00), and their BMI was
44.89. (35.06-74.39). Following surgery, the average weight was 80.77 kg (11.92 pounds) and the average BMI was 29.46 (11.00 pounds), both of which had significantly decreased (p=0.003 and p=0.002, respectively). At 12 months after surgery, endoscopic examinations of the pouch, residual stomach, and duodenum were performed on all patients. The average amount of extra weight removed was 68.21%. We come to the conclusion that the suggested modifications to RYGB (GBLP+GIB- Roux-en-Y gastric bypass with long pouch and gastrointestinal bipartition) did not impair weight loss or control of type 2 diabetes and other comorbidities and demonstrated to be a safe and effective alternative without gastroduodenal exclusion, enabling a better postoperative follow-up.
Keywords
Paediatric case report; Survival; Pancreatic surgery; Mortality
Introduction
Obesity has become more prominent in the context of managing Chronic Non-Communicable Diseases (CNCDs) because of its complicated and multiple causes, challenging treatment, and significant development in recent decades. Obesity, which is characterised by excess weight primarily due to the accumulation of fat in subcutaneous and visceral regions, has developed as a result of a complex interaction between genetic variability within an individual, endocrine and neuroendocrine changes, and environmental factors, such as excessive consumption of high-calorie foods and decreased levels of physical activity. Indirect, direct, and intangible expenses for he Unified Health System and other social sectors are involved with the treatment of comorbidities linked to excess weight and the impairment of the individual's functionality. The anticipated annual cost of these disorders in Brazil is R$3.6 billion, with the biggest percentages going to cancer (15%) and cardiovascular diseases (67%) respectively. Clinical, pharmaceutical and surgical procedures are used to treat obesity when other treatment options have failed. These latter procedures, often known as gastroplasty or bariatric surgeries, are characterized by a restriction of the intestine's ability to absorb food and/or gas. They carry out a therapy procedure whose objective is to reduce the health issues brought on by this clinical condition [1].
Bariatric surgery has benefits that go far beyond just significant and long-lasting weight loss. In 76.8% of cases, type II diabetes was completely reversed in highly obese patients who underwent surgery. In up to 85.7% of instances, obstructive apnea resolves; in 78.5% of cases, systemic arterial hypertension improves; and in 88% of cases, the hyperlipidemic syndrome is resolved with a decrease in serum triglyceride and cholesterol levels. The reduction of total mortality by up to 35%, morbidity, and the chance of death from cardiovascular diseases are the most significant effects of this outcome. In this regard, bariatric surgery is more successful than non-surgical methods in improving or curing comorbid disorders in obese patients. Despite the fact that bariatric surgery has numerous advantages, certain studies have revealed that the patient is still susceptible to problems and negative effects related to the anatomical and physiological alterations brought on by this technique [2].
Gallstones, gastroenteric-anastomosis stenosis, digestive fistulas, intraabdominal hemorrhage, occlusion, hernias, and nutritional issues like vitamin, iron, and folic acid deficiencies are a few of these difficulties. Other difficult bariatric surgery outcomes include those linked to the excluded stomach, including bile reflux, gastritis and/or gastric and duodenal ulcers, polyp emergence, and difficulty/impossi bility of endoscopic access for investigation/therapy. Recent research has suggested that the duodenal content of the excluded stomach may enhance the risk of developing gastric cancer by creating a carcinogenic environment that may influence the organ's genetic response. Furthermore, mechanical restriction, malabsorption, or both are used in traditional bariatric procedures performed today. Scientific research has established over time that physiological explanations for mechanical restriction, malabsorption, and omitted segments do not exist. The goal of the ideal process should be to reduce the size of the functioning stomach and avoid eliminating any portions. According to studies, upper digestive endoscopy is the gold standard for the detection of gastric cancer since it is one of the primary exams for gastroduodenal evaluation and one of the methods for finding digestive system neoplasms and other gastric pathologies. Roux-en-Y Gastric Bypass (RYGB) patients' remaining stomachs are excluded during the procedure, making them susceptible to the aforementioned conditions. As a result, modifications to surgical techniques are required to allow endoscopic access to the gastroduodenal region and, consequently, the prevention, diagnosis, and treatment of potential complications in the excluded stomach. Therefore, the current study's objectives were to assess the effectiveness of the RYGB surgery as modified with a long pouch and endoscopic access to the remaining stomach (GBLP+GIB, or Rouxen-Y gastric bypass with long pouch and gastrointestinal bipartition), as well as weight loss and comorbidity control [3].
At the Alberto Rassi General State Hospital of Goiania, a prospective clinical experiment using a convenience sample was conducted. The medical and multidisciplinary team chose the patients who had requested metabolic surgery for the sample. The research was carried out between January 2020 and August 2021. Randomly chosen, twelve patients were asked to take part in the trial. They were fully informed of all dangers, potential advantages, and scheduled procedures. The informed consent form was signed by everyone who agreed to take part in the study. Age between 30 years and 70 years for those with a BMI greater than or equal to 30 kg/m2 and less than or equal to 34.9 kg/m2 , associated with Type 2 Diabetes Mellitus (DM2), and who did not have any medical conditions that would make them ineligible for the procedure. Participants could be either male or female. Dropout before the 12-months multidisciplinary preoperative follow-up period, membership in vulnerable groups, the presence of uncompensated psychiatric disorders or cognitive deficits confirmed by a psychiatrist and/or psychologist, the presence of alcohol or illicit drug abuse confirmed following a psychiatrist and/or psychologist's evaluation were the exclusion criteria. Existence of chronic conditions unrelated to obesity such as cancer, lung disease, nephropathy, heart disease, Parkinson's disease, and Alzheimer's disease; the existence of alcohol or illicit drug misuse confirmed following evaluation by a psychiatrist and/or psychologist; and/or prior bariatric procedures. During multidisciplinary pre-operative consultations, the selected patients' clinical data (age, weight, BMI, blood pressure, presented comorbidities, cardiovascular history, clinical treatments previously used to control DM2, eating habits, and physical activity) were obtained from their clinical records. With a long pouch and endoscopic access to the residual stomach and duodenum, the modified RYGB (GBLP+GI-Roux-en-Y gastric bypass with long pouch and gastrointestinal bipartition) was the surgical approach employed for these patients. First, a median laparotomy was done, and the length of the entire small intestine was measured. According to Chaim, a first horizontal fire approaches the tiny curvature of the stomach and produces a functioning gastric pouch that is about 18 cm long and 150 ml in size. In order to calibrate the functional gastric pouch and maintain the gastro-gastric communication, as described by de Melo, the following firing is performed vertically with a Fouchet probe at a distance of about 1 cm to 1.5 cm from the angle of Hiss, allowing endoscopic access for examinations and/or endoscopic procedures in the remaining stomach. With continuous 3-0 Vicryl suture, the staple lines of the gastric pouch and the residual stomach are strengthened. After that, the gastrointestinal transit is rebuilt in "Roux-en-Y," leaving a 250 cm biliopancreatic loop and a 100 cm alimentary loop from the angle of Treitz. Since the entire small intestine is measured, as was previously noted, it is also possible to determine the common loop's size. Following the roughly 30 mm ante colic gastroenteroanastomosis with a stapler, the abdominal cavity is drained, the gaps are closed and hemostasis is achieved, and the closure by planes and methylene blue test are all carried out [4-6].
The postoperative period, one week after hospital discharge, three months after surgery, and six months after surgery all included visits with a medical and interdisciplinary team. Every visit included standard outpatient clinical evaluation, data gathering, and postoperative exams. Nine months after the operation, an endoscopic evaluation of the access to the duodenum and stomach was performed. Absolute BMI measurements acquired after the surgical period were used to calculate the reduction in body weight that resulted. The pilot study had twelve participants. The mean age of these was 46.3 years, with 11 of them (91.7%) being female. The mean weight and BMI before surgery were 112.17 kg (92.00-150.00) and 44.89 kg/m2 (35.06-74.39). Each patient's small intestine size was measured throughout the procedure, along with the dimensions of the alimentary and gastric bypass loops. Neither during the procedure nor during the follow-up, there were any problems or patient deaths. According to literature statistics, the study subjects lost 18% (20.22 kg) and 28% (31.4 kg) of their body weight in 12 months and 18 months, respectively. Excessive weight loss indicates whether a surgery was successful; losses of more than 50% are regarded as such. In this study, patients presented a mean EWL of 68.21% in 18 months, values even higher than those found in the literature, since weight loss occurs in the first two years after surgery and remains stable after this period. The EWL was maintained at around 64.3% one year after bariatric surgery, which is similar to the values found there. Diabetes was in remission in the research participants. This was anticipated because it has been said that after metabolic surgery, diabetes remission rates can reach 76.8%. In diabetic patients, postoperative glycated hemoglobin readings are 5.8% on average one year after surgery [7].
Even patients who had a bigger gastric chamber formed in the RYGB, with sizes more than 100 ml, demonstrated EWL values that were comparable to those of patients who had a gastric chamber made of regular size, and even less weight gain in three years.
References
- Associaçao Brasileira para o Estudo da Obesidade e da Síndrome Metabólica (2016) Diretrizes brasileiras de obesidade 2016. 4th Edition, ABESO, São Paulo.
- Batsis JA, Romero-Corral A, Collazo-Clavell ML, et al. Effect of bariatric surgery on the metabolic syndrome: a population-based, long-term controlled study. InMayo Clin. Proc. 2008 Aug 1; 83(8): 897-906. Elsevier.
- Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery N. Engl. J. Med.. 2004 Dec 23;351(26):2683-93..
- Miettinen M, Sarlomo-Rikala M, Lasota J, et al. Gastrointestinal stromal tumors: recent advances in understanding of their biology. Hum. pathol.. 1999 Oct 1;30(10):1213-20..
- Blay JY, Von M, Blackstein ME, et al. Perspective on updated treatment guidelines for patients with gastrointestinal stromal tumors. Cancer. 2010 Nov 15;116(22):5126-37.
- Mochizuki Y, Kodera Y, Ito S, et al. Treatment and risk factors for recurrence after curative resection of gastrointestinal stromal tumors of the stomach. World J Surg 2004;28:870-5.
- Fong Y, Coit DG, Woodruff JM, et al. Lymph node metastasis from soft tissue sarcoma in adults. Analysis of data from a prospective database of 1772 sarcoma patients. Ann Surg 1993;217:72-7.