Low dose human menopausal gonadotrophin with clomiphene citrate for ovulation induction in clomiphene citrate resistant polycystic ovarian syndrome women
Received: 05-Mar-2018 Accepted Date: Mar 20, 2018; Published: 29-Mar-2018
Citation: Mathews B, Chitra T, Dasari P. Low dose human menopausal gonadotrophin with clomiphene citrate for ovulation induction in clomiphene citrate resistant polycystic ovarian syndrome women. J Reprod Biol Endocrinol. 2018;2(1):51-54.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
BACKGROUND: To evaluate the efficacy of Clomiphene Citrate (CC) with low dose Human menopausal gonadotrophin (hMG) in CC resistant infertile women with Polycystic Ovarian Syndrome (PCOS).
DESIGN: Prospective single arm interventional study.
SETTING: Infertility clinic attached to Women Child Hospital, JIPMER, India.
PATIENTS AND METHODS: Infertile women diagnosed with PCOS who are Clomiphene Citrate resistance. We excluded women who underwent Laparoscopic Ovarian Drilling (LOD) within 6months or who had other factors of infertility.
INTERVENTION: Ninety-one CC resistant PCOS women were recruited. CC (100 mg/day for 5 days) followed by Human Menopausal Gonadotrophin (hMG) (75IU IM for 3 days) were administered. Three Additional doses of hMG were given if dominant follicular size was not achieved. Intrauterine Insemination (IUI) was not done. If pregnancy was not achieved, course was repeated for 3 cycles.
MAIN OUTCOME MEASURE: Ovulation rate and cumulative pregnancy rate. RESULTS: Ovulation rate was 92.3% and cumulative pregnancy rate observed was 20.9% with sequential clomiphene citrate and low dose hMG among CC resistant PCOS. Thirty three percent of study population ovulated with three doses of hMG whereas 59.3% of cases required additional hMG doses. All patients who underwent LOD ovulated and 37% achieved pregnancy, but lacked clinical significance due to small sample size. We observed four cases of ovarian cysts and only one case each of OHSS and multiple pregnancy.
CONCLUSION: Sequential clomiphene citrate and low dose hMG regimen is a good option for clomiphene citrate resistant PCOS women with a 20% chance of pregnancy over 3 cycles and decreased risk of side effects.
Keywords
Clomiphene citrate; Clomiphene citrate resistance; PCOS; Human menopausal gonadotrophin; Low dose hMG; Ovulation induction
Polycystic ovarian syndrome (PCOS) is still the most common cause of anovulatory infertility accounting for 90-95% (1) with a prevalence rate as high as 15% with Rotterdam criteria (2). Clomiphene citrate (CC) is the first line drug for ovulation induction with a high ovulation rate of 70-80% however it could not be converted to equally high pregnancy rates (8 to 40%) (3-5). The NICE (6) defines CC resistance as: “Anovulatory women who do not ovulate while receiving the 150 mg dose of Clomiphene citrate”. CC resistance accounts for about 25% (7), reasons are unclear; it may be due to the anti-estrogenic effect of CC on endometrium, cervical mucus and associated high LH, resulting in luteal phase dysfunction (8).
When lifestyle modifications proved futile, an extended Clomiphene therapy or combination of Clomiphene with insulin sensitizers, dexamethasone or drugs like aromatase inhibitors, gonadotrophins, dopamine agonists or LOD were all tried with varying success rates. Newer drugs like D-Chiroinositol, Chromium picolinate, N-acetyl cysteine (NAC) and Myoinositol are still in the experimental phase. Widely accepted second line management is gonadotrophin and LOD. Need for expertize, invasive procedure, anaesthetic and surgical complications, cortical damage, decreased ovarian reserve and chances of premature ovarian failure makes LOD secondary to Gonadotrophins. Gonadotrophins were initially administered at a high starting dose of 150 IU once a day. It does not exert a peripheral antiestrogenic effect and hence may be used in CC non-responders. This conventional protocol resulted in an unacceptable rate of excessive follicle development and increased risk of ovarian hyperstimulation (8.4-23%) (9). Hence, focus shifted to develop low-dose protocols (37.5–75 IU/day), which have essentially replaced the original conventional protocol. The purified recombinant version proved lesser incidence of side effects but was not affordable to major crowd. About 20% of women fail to ovulate in spite of increasing dose to maximum daily dose (10,11)
Thus, there is a need for cost effective treatment regimen with success rates equivalent to LOD or conventional high dose hMG regimen and significantly lower side effects. Recently, sequential CC/HMG is used as an alternative, it approaches the effectiveness of standard HMG therapy with a significant economic advantage and markedly lower rate of multiple gestation (12,13). A better endometrial response and comparable ovulation and pregnancy rates among CC resistant women was observed at very cheap per cycle cost (10,14). Most of these studies did not use CC resistant PCOS patients as study subjects and they used intrauterine insemination (IUI) or other assisted reproductive techniques (ART) along with ovulation induction for achieving pregnancy.
There is insufficient data on use of low dose hMG with CC in CC resistant PCOS patients without intrauterine insemination (IUI) or other ART. This study hence gains importance by using CC plus low dose hMG for Ovulation induction in PCOS women with CC resistance and CC failure without the use of ART. Since the hMG is given in low dose, the chance for side effects such as ovarian hypersensitivity syndrome and multiple pregnancies are less with increased ovulation and pregnancy rates.
Objective
To evaluate the efficacy of Clomiphene Citrate (CC) with low dose Human menopausal gonadotrophin (hMG) in CC resistant infertile women with Polycystic Ovarian Syndrome (PCOS).
Patients and Methods
This was a prospective single arm interventional study. We recruited patients from the infertility clinic attached to Women Child Hospital, between February 2016 and February 2017. Study was approved by the Institute Ethics Committee (JIP/IEC/2015/17/631). Women included were between 21-35yrs with (a) PCOS diagnosed by Rotterdam criteria (15) and (b) CC resistance as defined by failure to ovulate with at least 3 cycles of CC 100 mg or more for 5 days. Male factor infertility, tubal infertility, LOD within last 6 months and other causes of infertility were excluded from the study.
Treatment protocol
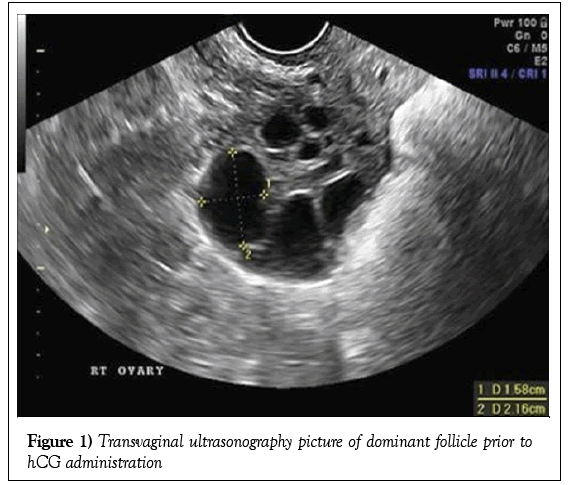
Informed consent was taken from the patient as well as partner. Patients were instructed to take 100 mg CC daily from day 2 of menses at same time of day for 5 days. hMG 75IU intramuscular injection was given daily from day 6 for 3 doses (6th to 8th day). Follicular monitoring was done by TVS (using Voluson E8 machine at 7.5 MHz probe frequency) starting from Day 9 and every alternate day thereafter, additional doses of HMG 75 IU were given IM daily till dominant follicle reached 18 mm in size. Figure 1 shows transvaginal ultrasonography picture of a dominant follicle prior to ovulation. Ovulation trigger was given by HCG 5000 IU IM and was confirmed by disappearance of dominant follicle, change in the shape of the follicle or appearance of internal echoes within the follicle or free fluid in the pouch of Douglas. Couple was advised to have timed intercourse once ovulation was confirmed. Clinical pregnancy was confirmed by visualization of gestational sac in TVS performed 14 days after hCG administration. Luteal phase support was given for 14 days after confirming ovulation with micronized progesterone 200 mg twice daily (Susten, 200 mg tablet Sun pharmaceuticals Bangalore, India). Confirmed pregnancies were followed up for pregnancy outcome. Whenever there was no dominant follicle by Day 18, the cycle was abandoned. If four or more follicles measuring more than 16 mm were present, the cycle was cancelled and the HCG withheld. OHSS occurred was managed according to the protocol.
Variables
Baseline characteristics and investigations were collected from the patients at first visit. Primary outcome measured was ovulation rate, while the secondary outcomes were cumulative pregnancy rate, follicular size and endometrial thickness at HCG administration, OHSS and multiple pregnancies.
Study size
Using data from previous study (10) (80% ovulation rate), setting type I error (α) at 0.05 and assuming a dropout rate of 10%, sample size was estimated to be 92. Calculations were done using NMASTER software with 10% relative precision.
Statistical analysis
Statistical package for social sciences (SPSS), version 20 was used for analysis. Numerical variables were presented as mean and standard deviation. Normality of data was checked using Kolmogorov-Smirnov test. Continuous variables like maximum follicular diameters and endometrial thickness were expressed as mean and standard deviation. Variables, which did not follow the normal distribution curve, were expressed in median with interquartile range. Ovulation rates and pregnancy rates were calculated and presented as percentages with Confidence Intervals. Chi square test and Mann Whitney U test was used to compare the results. A difference with p value <0.05 was considered statistically significant.
Results
During the one-year study period, 95 patients were recruited, of them, four were lost to follow up and 91 patients were finally analysed. Table 1 shows the baseline characteristics of the study population, majority of the study participants belong to the 20-30 years age group. Table 2 depicts the mean number of dominant follicles at hCG, monofollicular rate and endometrial thickness.
| S.no: | Clinical Profile | Total Number (n=91) | Percentage (%) | Mean ± SD |
|---|---|---|---|---|
| 1 | Age | |||
| 21-25 years | 32 | 35.2 | 27.3 ± 3.7 | |
| 26-30 years | 44 | 48.4 | ||
| 31-35 years | 15 | 16.5 | ||
| 2 | BMI (1) | |||
| Underweight | 0 | 0 | 25.73 ± 2.96 | |
| Normal BMI | 33 | 36.3 | ||
| Overweight | 54 | 59.3 | ||
| Obese | 4 | 4.4 | ||
| Morbidly obese | 0 | 0 | ||
| 3 | Type of Infertility | |||
| Primary Infertility | 80 | 87.9 | ||
| Secondary Infertility | 11 | 12.1 | ||
| 4 | No of Years of Infertility | |||
| 1-6 years | 62 | 68.1 | 5.59 ± 2.9 | |
| 7-12 years | 26 | 28.6 | ||
| = 12 years | 3 | 3.3 | ||
| 5 | No of Cycles of Clomiphene citrate received | |||
| 3 cycles | ||||
| 4-6 cycles | 62 | 68.1 | ||
| >6 cycles | 22 | 24.2 | ||
| 7 | 7.7 | |||
| 6 | History of LOD | 19 | 20.9 | |
| 7 | Ovulatory dysfunction | 87 | 95.6 | |
| 8 | Hirsutism | 61 | 67 | |
S.no Serial number; SD Standard deviation; BMI Body mass index; LOD Laparoscopic ovarian drilling
Body Mass Index: Underweight <18.5; Normal 18.6-24.9; Overweight 25-29.9; Obese 30-39.9: Morbidly obese: >40 kg/m2
Table 1: Clinical profile of the study subjects
| Sample size (n) | 91 |
|---|---|
| Cycles (n) | 245 |
| Mean no: of Dominant Follicles at hCG | 1 |
| Monofollicular cycles (%) | 56.9 |
| DF size at hCG (mm) | 20.1 |
| ET at hCG (mm) | 8.2 |
hCG Human chorionic gonadotropin; DF Dominant follicle; ET Endometrial thickness
Table 2: Cycle characteristics
Percentage of ovulatory cycles in 1st, 2nd and 3rd cycles of ovulation induction are given in Table 3. Patients who conceived were excluded in the subsequent cycles. Out of the ninety-one patients, sixty-four ovulated in first cycle and one patient developed mild OHSS. Among the 26 patients who did not ovulate in the first cycle, 16 ovulated in second cycle and four in the third cycle. Six patients did not achieve ovulation in any of the 3 cycles. One third of the patients ovulated with the three doses of low dose hMG without additional doses. Another one third ovulated with additional three doses of low dose hMG, whereas, six women did not respond to additional six doses of hMG also.
| Cycle | Ovulation Achieved (%) | Pregnancy (%) |
|---|---|---|
| 1st Cycle (n=91) | 64 (70.3) | 7 (7.7) |
| 2nd Cycle (n=81) | 66 (81.5) | 7 (8.6) |
| 3rd Cycle (n=73) | 58 (79.5) | 5 (6.8) |
Table 3: Ovulation and pregnancy rates
Hence, among the 91 patients studied, 84 patients achieved ovulation, which accounted for 92.3% (C.I: 84.3-96.6%). Two hundred forty five induction cycles were there, of which 188 cycles achieved ovulation accounting for 77% (C.I: 71.1-82.1%). Nineteen successful pregnancies were reported with Pregnancy rate of 20.9% (C.I: 13.34-30.92). Among the 91 patients, forty of them ovulated in all 3 cycles but failed to achieve pregnancy.
Among the 19 pregnancies, 18 pregnancies were singleton of which four patients had spontaneous first trimester pregnancy loss and other 14 had normal vaginal delivery at term. Only one multiple pregnancy was noted in the study who delivered normally. Clomiphene citrate and Low dose HMG were well tolerated in the study subjects with 93.4% of women reporting no side effects during the study period. Four cases reported ovarian cysts of 4-6 cm size, all four of them developed in second cycle of ovulation induction. Ovarian cysts subsided without surgery when followed up for a period of 3 months. The one mild OHSS developed, was in the first cycle of ovulation induction and the patient had eight follicles with more than 22mm size, was deprived of further dose of HMG and HCG, and was successfully managed conservatively.
Discussion
Global burden on PCOS is on the rise and so is clomiphene resistance. The options for alternate drug for ovulation induction is many but are limited by the side effects and varying success rates. In our study we used combination of clomiphene citrate with low dose human menopausal gonadotrophin for ovulation induction over three cycles and achieved high ovulation rate with reduced side effects. However, the high ovulation rates were not supported by equally high pregnancy rates, which might be attributed to lower endometrial thickness.
Monofollicular cycle rate of the present study is 56.7%, similar to other studies (7,16,17) except for the study Abdelazim et al. (18), who had a 3.2 follicular as mean number of follicles. This study suggests that using low dose HMG with CC for ovulation induction in PCOS women leads to development of fewer dominant follicles thereby reducing risk of OHSS. While most studies there is no mention on monofollicular rate, Cheng et al. (7) had reported 11.8% OHSS rate with 48.4% monofollicular rate and no OHSS with a monofollicular rate of 65.3% in Wenyan et al. (16).
Mean ET of the study group was 8.2 mm and was similar to other studies. Altay et al. in 2007 (19) published with similar findings that the endometrial thickness was significantly lower in the minimal stimulation group with CC and rFSH when compared with rFSH alone. This thin ET may be attributed to the anti-estrogenic effect of CC.
Pregnancy rate observed in our study of 20.9% was comparable to the other similar studies (10) as shown in the Table 4. The low pregnancy rate might be attributed to the anti-estrogenic effects of clomiphene citrate evident by the low mean endometrial thickness at the time of HCG administration. Mathew et al. (7) and Cheng et al. (10) used similar minimal protocols, although on a different population. Mathew et al. (7) studied on general population with a single dose of 150IU along with CC to yield an ovulation rate of 82% and pregnancy rate of 21%. In his study anovulation comprised of only 60% of study population. Whereas Cheng compared two groups from Chinese population, one with CC and HMG and another with additional Metformin to CC and HMG. He concluded that the cumulative pregnancy rate was improved with addition of metformin to CC and hMG in PCOS patients. The difference in the above-mentioned study might be due to difference in selection of patients, they included all patients with infertility history who received minimal stimulation protocol. Whereas in this study, clomiphene citrate with low dose HMG among CC resistant PCOS women achieved a better ovulation rate.
| Sl No | Authors | Year | Study Population | Stimulation Cycles | Dosage | ET (mm) | Monofollicular rate | Ovulation rate | Pregnancy rate |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Mathew et al. (10) | 2000 | 67 | 221 | 100 mg+150IU | >8 | - | 82% | 21% |
| 2 | Rashidi et al. (20) | 2005 | - | 66 | 100 mg+150IU | 9.9 | 65.3 | 12.10% | |
| 3 | Cheng et a.l (7) | 2010 | 30 | 76 | 50 mg+75IU | 8.7 | - | 87.30% | 20% |
| 4 | Abdelazim et al. (18) | 2013 | 45 | 45 | 100 mg+75IU | 8.9 | 48.4 | - | 26.70% |
| 5 | Ghanem et al. (17) | 2013 | 87 | 82 | 100 mg+37.5IU | 8.8 | - | 72.40% | 27.50% |
| 6 | Wenyan et al. (16) | 2015 | 90 | 90 | 50 mg+75IU | 10.6 | - | 80% | 18.90% |
| 7 | Present Study | 2016 | 91 | 245 | 100 mg+75IU | 8.2 | 56.9 | 92.30% | 20.90% |
Table 4: Comparison of ovulation rate, pregnancy rates and endometrial thickness from different studies
Abortion rate of 21% was significantly lower than many other studies (10,20). Only one multiple pregnancy occurred owing to 5.5% who delivered at term. Ghanem et al. (17) had significantly lower abortion rates of 8.3 and 11.7%, respectively. The average endometrial thickness at HCG administration was 10.6 mm in his study as compared to 8.2 mm in this study suggesting the possibility of thicker endometrium being better receptive for pregnancy. We had one case of OHSS in the mild grade which was conservatively managed, the low rate been attributed to the use of low dose hMG and high monofollicular rate.
Limitations
This study had some limitations; the patients were recruited from single hospital, which was tertiary care hospital. Early marriage rampant in the society was responsible for the increased infertility incidence among younger age group. This study was a prospective interventional study. An RCT comparing the low dose regimen with high dose Gonadotrophin therapy would answer the question whether addition of low dose hMG to CC would have an improved pregnancy rate.
Further studies are required to look in to factors necessitating the additional hMG dose, correlation of endometrial thickness with early pregnancy losses and response of LOD with CC and hMG.
Conclusion
Thus, the present study shows that sequential use of CC with hMG is associated with good ovulation rate (92.3%) and pregnancy rate (20.9%) without IUI. It also minimizes the risk of OHSS and Multiple pregnancies, which we found to be 1.1% each. It also leads to an increased monofollicular rate, which further help in reducing the risk of complications. Hence sequential clomiphene citrate and low dose hMG regimen is good option for young clomiphene citrate resistant PCOS women with a 20% chance of pregnancy over 3 cycles without IUI and decreased risk of side effects.
Acknowledgements
This study was conducted in the Women Children Hospital under the Department of Obstetrics and Gynecology. We would like to thank all faculties and family for providing the support and help needed. Extending our gratitude to JIPMER for giving us the opportunity.
REFERENCES
- Farquhar CM, Williamson K, Gudex G, et al. A randomized controlled trial of laparoscopic ovarian diathermy versus gonadotropin therapy for women with clomiphene citrate-resistant polycystic ovary syndrome. Fertil Steril. 2002;78(2):404-11.
- Fauser BC, Tarlatzis BC, Rebar RW, et al. Consensus on women’s health aspects of polycystic ovary syndrome (PCOS): The Amsterdam Eshre/Asrm-Sponsored 3rd PCOS Consensus Workshop Group. Fertil Steril. 2012;97(1):28-38.
- Hammond MG, Halme JK, Talbert LM. Factors affecting the pregnancy rate in clomiphene citrate induction of ovulation. Obstet Gynecol. 1983;62(2):196-202.
- Batukan C, Baysal B. Metformin improves ovulation and pregnancy rates in patients with polycystic ovary syndrome. Arch Gynecol Obstet. 2001;265(3):124-7.
- Amin M, Abdel-Kareem O, Takekida S, et al. Up-date management of non-responder to clomiphene citrate in polycystic ovary syndrome. Kobe J Med Sci. 2003;49(3):59-73.
- Fertility Problems: Assessment and Treatment.
- Cheng J, Lv J, Li CY, et al. Clinical outcomes of ovulation induction with metformin, clomiphene citrate and human menopausal gonadotrophin in polycystic ovary syndrome. J Int Med Res. 2010;38(4):1250-8.
- Mukherjee S, Sharma S, Chakravarty BN. Comparative evaluation of pregnancy outcome in gonadotrophin-clomiphene combination vs. clomiphene alone in polycystic ovarian syndrome and unexplained infertility-a Prospective clinical trial. J Hum Reprod Sci. 2010;3(2):80-4.
- Schenker JG, Weinstein D. Ovarian hyperstimulation syndrome: A current survey. Fertil Steril. 1978;30(3):255-68.
- Mathew M, Al-Busaidi F, Krolikowski A. Minimal stimulation protocol: A cheap and effective method of ovulation induction. J Sci Res Med Sci. 2000;2(1):33-5.
- Moazami Goudarzi Z, Fallahzadeh H, Aflatoonian A, et al. Laparoscopic ovarian electrocautery versus gonadotropin therapy in infertile women with clomiphene citrate-resistant polycystic ovary syndrome: A systematic review and meta-analysis. Iran J Reprod Med. 2014;12(8):531-8.
- Brzechffa PR, Daneshmand S, Buyalos RP. Sequential clomiphene citrate and human menopausal gonadotrophin with intrauterine insemination: The effect of patient age on clinical outcome. Hum Reprod Oxf Engl. 1998;13(8):2110-4.
- Kemmann E, Jones JR. Sequential clomiphene citrate-menotropin therapy for induction or enhancement of ovulation. Fertil Steril. 1983;39(6):772-9.
- Lu PY, Chen AL, Atkinson EJ, et al. Minimal stimulation achieves pregnancy rates comparable to human menopausal gonadotropins in the treatment of infertility. Fertil Steril. 1996;65(3):583-7.
- Rotterdam ESHRE/ASRM-sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19-25.
- Xi W, Liu S, Mao H, et al. Use of letrozole and clomiphene citrate combined with gonadotropins in clomiphene-resistant infertile women with polycystic ovary syndrome: a prospective study. Drug Des Dev Ther. 2015;9:6001-8.
- Ghanem ME, Elboghdady LA, Hassan M, et al. Clomiphene citrate co-treatment with low dose urinary FSH versus urinary FSH for clomiphene resistant PCOS: randomized controlled trial. J Assist Reprod Genet. 2013;30(11):1477-85.
- Abdelazim IA, Makhlouf HH. Sequential clomiphene citrate/hMG versus hMG for ovulation induction in clomiphene citrate-resistant women. Arch Gynecol Obstet. 2013;287(3):591-7.
- Altay M, Gelisen O, Kocak M, et al. Comparison of a novel minimal stimulation protocol with clomiphene citrate plus recombinant follicle-stimulating hormone to recombinant follicle-stimulating hormone alone for ovulation induction: A prospective study.
- Rashidi BH, Gharaie M, Tehraninejad MMES. A comparison of clomiphene citrate and sequential clomiphene citrate plus human menopausal gonadotropin for use in conjunction with intrauterine insemination. Acta Med Iran. 2005;43(3):187-92.