Lung mechanic as predictor of prognosis in COVID-19 ARDS patients in Albaraha hospital from November 2020 till February 2021
Received: 07-Jun-2023, Manuscript No. PULJEDPM-23-6576; Editor assigned: 09-Jun-2023, Pre QC No. PULJEDPM-23-6576 (PQ); Reviewed: 19-Jun-2023 QC No. PULJEDPM-23-6576; Revised: 15-Jan-2024, Manuscript No. PULJEDPM-23-6576 (R); Published: 22-Jan-2024
Citation: Elhasan REM. Lung mechanic as predictor of prognosis in COVID-19 ARDS patients in Albaraha hospital from November 2020 till February 2021. J Emerging Dis Prev Med. 2024;7(1):1-8.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: COVID-19 also known as the Coronavirus is a contagious disease caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV- 2). Acute respiratory distress syndrome is a life-threatening condition of seriously ill patients, characterized by poor oxygenation, pulmonary infiltrates, and acuity of onset.
Objective: The aim of this study is to determent the association between lung mechanics, outcome and prognosis of ARDS COVID-19 patient.
Methods: This is an analytical retrospective hospital-based study was conducted in AL-Baraha private hospital during the period from November 2020 to February 2021. Total coverage method was used in this study. A number of 50 COVID-19 patients were included in this study. The data were collected from the statistic department and from the ICU records of the COVID-19 patients.
Results: In this study, the mean age of the participants was 70 years (SD=10) and most of the study participants were males (72%). The mean oxygen saturation (SpO2) was 90.3 (SD=5.5), the mean tidal volume in this study was 452.9 ml (SD=99.6), all the participants had a peak pressure of more than 30 cm H2O. In this study, 42 (84%) of the participants had a low lung compliance. The mean duration of endotracheal intubation among the study participants was 9.7 days (SD=6.6). All the study participants in this study were died. This study found no association between the lung compliance and the duration of endotracheal intubation among the study participants (p-value=0.78).
Conclusion: COVID-19 may cause hypoxemic respiratory failure and Acute Respiratory Distress Syndrome (ARDS). Recent data have shown that ARDS related to COVID-19 shares common pathophysiological and clinical features with ARDS of other causes. This study found no association between the lung compliance and the duration of endotracheal intubation among the study participants. This study also found that there is no statistical association between the gender and lung compliance among the study participants.
Keywords
Endotracheal intubation; COVID-19; Pulmonary injury; Lung compliance; Respiratory failure
Abbreviations
ARDS: Acute Respiratory Distress Syndrome; CARDS: COVID ARDS; PEEP: Positive End Expiratory Pressure; IRV: Inspiratory Reserve Volume; TV: Tidal Volume; ERV: Expiratory Reserve Volume; RV: Residual Volume; IC: Inspiratory Capacity; FRC: Functional Residual Capacity; VC: Vital Capacity; TLC: Total Lung Capacity; FEV1: Forced Expiratory Volume; PaO2:Patient's Oxygen in arterial blood; FiO2:Fraction of the Oxygen in the Inspired air; CPAP: Continuous Positive Airway Pressure; APRV: Airway Pressure Release Ventilation; BiPAP: Bi-level Airway Pressure; SPSS: Statistical Package for the Social Sciences; SMSB: Sudan Medical Specialization Board
Introduction
COVID-19 is an acute illness classified as a global pandemic caused by a new strain of Coronavirus called SARS-CoV-2; firstly reported in December 2019 with the number of confirmed cases till march 2021 reach 124.215.843 and number of death reaches 2,759,891 with the pandemic now reaches its third wave [1]. It does not only affect the respiratory system but it also affects other systems, symptoms can range from mild sickness to life threatening conditions associated with multi-organ failure and with a mortality rate of about 2% most of the deaths take place when the patient develops ARDS (CARDS) [2].
Acute Respiratory Distress Syndrome (ARDS) is an acute diffuse, inflammatory lung injury, leading to increase pulmonary vascular permeability, increased lung weight, and loss of aerated lung tissue with hypoxemia and bilateral radiographic opacity, associated with increase venous admixture, increase physiological dead space and decrease lung compliance; CARDS it is classified into three categories according to PaO2/FiO2 ratio into: Mild, moderate and severe with mortality rate increases with its severity, about 25% are classified as mild and 75% as moderate or severe, I and it’s mortality rate are about 27%, 32% and 45%. ARDS have many causes including severe pneumonia, sepsis, trauma and COVID-19 patients, COVID ARDS (CARDS) have clinical differences from ARDS from other causes in: Delay time of onset, higher compliance and oxygenation index [3].
Lung mechanics is an expression of lung function through measures of pressures and slow which includes: Tidal volume which defines as the amount of air that moves in or out of the lung with each respiratory cycle plateau pressure which is the pressure applied to small airways during positive pressure ventilation, Positive End Expiratory Pressure (PEEP) which define as the pressure that will remain in the airways at the end of the respiratory cycle, compliance define as change in volume that occur per unit change in the pressure and the driving pressure is the pressure above PEEP applied to the entire respiratory system to achieve tidal ventilation; this mechanics can reflect the ability of each patient lung to function which linked to their survival; some of them are obtained directly from the ventilator and some are calculated [4-7].
COVID-19 patients who develop ARDS are one of the most challenging patients to deal with in terms of medical approach and treatment with the disease pathophysiology not fully understood yet, with the lung mechanics of the patients differ from each other, research on how lung mechanics may predict the prognosis and outcome of CARDS patients may play a role in the future management of this patient.
Lung and lung mechanics
The lungs are the foundational organs of the respiratory system, whose most basic function is to facilitate gas exchange from the environment into the bloodstream. Oxygen gets transported through the alveoli into the capillary network, where it can enter the arterial system, ultimately to perfuse tissue. The lungs further divide into individual lobes, which ultimately subdivide into over 300 million alveoli. The alveoli are the primary location for gas exchange. The diaphragm is the primary respiratory muscle and receives innervation by the nerve roots of C3, C4, and C5 via the phrenic nerve. The external inter-costal are inspiratory muscles used primarily during exercise and respiratory distress [8].
The function of the pulmonary system is to extract oxygen from the environment and provide it for aerobic respiration at the cellular level. Oxygen is ultimately used to produce ATP, and carbon dioxide is breathed out with other metabolic byproducts [9].
Respiratory tract organs facilitate the process of gas exchange, including the nose, oral cavity, throat, trachea, bronchi, and lungs. The lungs divide into five major lobes: Three lobes on the right and two lobes on the left. Each lobe is made up of many small alveoli, which are the primary site of gas exchange. At the alveoli, diffusion of gases into the arterioles occurs [10-11].
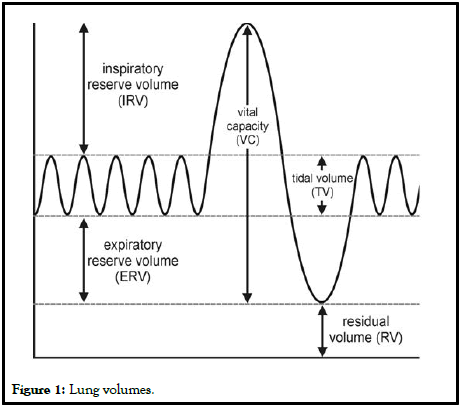
The significant (Figure 1) lung volumes/capacities and their definitions are listed below:
• Inspiratory Reserve Volume (IRV): Volume that can be breathed after
a normal inspiration.
• Tidal Volume (TV): Volume inspired and expired with each breath.
• Expiratory Reserve Volume (ERV): Volume that can be expired after a
normal breath.
• Residual Volume (RV): Volume remaining in lung after maximal
expiration (cannot be measured by spirometry).
• Inspiratory Capacity (IC): Volume that can be breathed after normal
exhalation.
• Functional Residual Capacity (FRC): Volume remaining in the lungs
after normal expiration.
• Vital Capacity (VC): Maximum volume able to be expired after
maximal inspiration.
• Total Lung Capacity (TLC): Volume of air in the lungs after maximal
inspiration.
• Forced Expiratory Volume (FEV1): Volume that can be expired in 1
second of maximum forced expiration.
COVID-19
COVID-19 also known as the coronavirus is a contagious disease caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). The first known case was identified in Wuhan, China, in December 2019 then the disease spread worldwide, leading to an ongoing pandemic [12].
Transmission of COVID-19 occurs when people are exposed to virus-containing respiratory droplets and airborne particles exhaled by an infected person. Those particles may be inhaled or may reach the mouth, nose, or eyes of a person through touching or direct deposition [13]. The risk of infection is highest when people are close for a long time, however; the virus particles can be inhaled even over longer distances, mainly indoors in poorly ventilated and crowded spaces. These conditions help the small particles to remain suspended in the air for minutes to hours. In addition, touching a contaminated surface or object may lead to infection although this does not contribute substantially to transmission [14,15].
Symptoms of COVID-19 vary in the general population; however; often include fever, cough, fatigue, headache, breathing difficulties, and loss or change of smell and taste. Symptoms may begin 1 to 14 days after exposure to the virus. However, it is important to mention that a third of people who are infected do not develop obvious symptoms. On the other hand, for those people who develop noticeable symptoms enough to be classed as patients, 81% develop mild to moderate symptoms, while about 14% develop severe symptoms, and only 5% experience critical symptoms (like shock, respiratory failure, or multi-organ dysfunction). Older people are at a higher risk of developing severe symptoms. Furthermore, some people continue to experience a range of effects for months after recovery [16].
Regarding the preventive measures of the COVID-19, it includes physical or social distancing, ventilation of indoor spaces, quarantining, hand washing, covering coughs and sneezes, and keeping unwashed hands away from the face. To minimize the risk of transmission; the use of face masks or coverings has been recommended in public. Moreover, several vaccines have been developed and many countries have initiated mass vaccination campaigns [17].
Management involves the treatment of symptoms, supportive care, isolation, and experimental measures. Although work is underway to develop drugs that inhibit the virus, the primary treatment is symptomatic.
ARDS
Overview: Acute Respiratory Distress Syndrome (ARDS) is a lifethreatening condition of seriously ill patients, characterized by poor oxygenation, pulmonary infiltrates, and acuity of onset. On a microscopic level, the disorder is associated with capillary endothelial injury and diffuse alveolar damage [18].
ARDS is defined as an acute disorder that starts within 7 days of the inciting event and is characterized by bilateral lung infiltrates and severe progressive hypoxemia in the absence of any evidence of cardiogenic pulmonary edema. ARDS is defined by the patient's oxygen in arterial blood (PaO2) to the fraction of the oxygen in the inspired air (FiO2). These patients have a PaO2/FiO2 ratio of less than 300. The definition of ARDS was updated in 2012 and is called the Berlin definition. It differs from the previous American European consensus definition by excluding the term acute lung injury; it also removed the requirement for wedge pressure <18 and included the requirement of Positive End-Expiratory Pressure (PEEP) or Continuous Positive Airway Pressure (CPAP) of greater than or equal to 5.
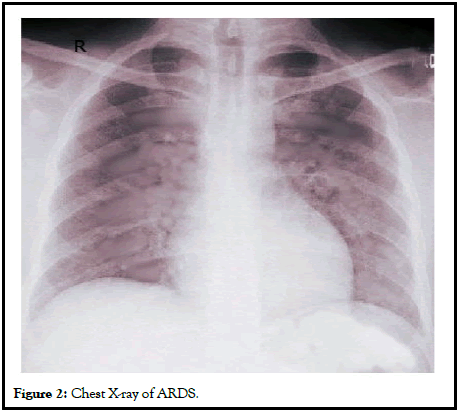
Etiology: ARDS has many risk factors. Besides pulmonary infection or aspiration, extra-pulmonary sources include sepsis, trauma, massive transfusion, drowning, drug overdose, fat embolism, inhalation of toxic fumes, and pancreatitis. These extra-thoracic illnesses and/or injuries trigger an inflammatory cascade culminating in pulmonary injury (Figure 2) [19].
Pathophysiology: It progresses through different phases, starting with alveolar-capillary damage, a proliferative phase characterized by improved lung function and healing, and a final fibrotic phase signaling the end of the acute disease process. The pulmonary epithelial and endothelial cellular damage is characterized by inflammation, apoptosis, necrosis, and increased alveolar-capillary permeability, which leads to the development of alveolar edema and proteinosis. Alveolar edema, in turn, reduces gas exchange, leading to hypoxemia. A hallmark of the pattern of injury seen in ARDS is that it is not uniform. Segments of the lung may be more severely affected, resulting in decreased regional lung compliance, which classically involves the bases more than the apices [20].
Management: There is no drug that has been proven to be effective in preventing or managing ARDS. The chief treatment strategy is supportive care and focuses on:
• Reducing shunt fraction.
• Increasing oxygen delivery.
• Decreasing oxygen consumption.
• Avoiding further injury. Patients are mechanically ventilated, guarded
against fluid overload with diuretics, and given nutritional support
until evidence of improvement is observed [21,22].
Novel invasive ventilation strategies have been developed to improve oxygenation. These include Airway Pressure Release Ventilation (APRV) and high-frequency oscillation ventilation (children). Patients with mild and some with moderate ARDS may benefit from non-invasive ventilation to avoid endotracheal intubation and invasive mechanical ventilation. These modalities include Continuous Positive Airway Pressure (CPAP), bi-level airway pressure (BiPAP), proportional-assist ventilation, and a high slow nasal cannula.
Previous studies
A study was conducted by Daniel Jafari et al., regarding the hypoxemia and respiratory system mechanics of COVID-19 ARDS. They create the Northwell COVID ARDS database in 2021 including 1595 patients categorized into three groups: Very low compliance, low normal and high. Out of these patients, 34.6% had very low compliance, 63.2% had low normal compliance and 2.2% had high lung compliance. The patients with very low compliance have double the median time in intubation in comparison with low normal which in turn had a longer time in comparison with high lung compliance patients [23].
A study conducted by Antoni Torres et al., in 2021 regarding the evolution of the ventilatory ratio is a prognostic factor in mechanically ventilated COVID-19 ARDS patients in Spain, in which this study included 2,095 patients with COVID-19 admitted to the ICU. In this study, 1,118 (53.3%) were intubated on day 1 and remained under mechanical ventilation at day three. From days 1 to 3, PaO2/FiO2 increased from 115.6 to 180.0 mmHg. This study found no association between mortality and the PaO2/FiO2 variation [24].
Another study was conducted by William Bain et al., in the USA to compare the COVID-19 versus non–COVID-19 acute respiratory distress syndrome in 2021, in which 27 patients with COVID-19 ARDS, 14 patients with viral ARDS, 21 patients with bacterial ARDS, and 30 patients with ARDS due to culture- negative pneumonia were enrolled in this study. This study found no differences in static compliance, hypoxemic indices, or carbon dioxide clearance between the study groups. Moreover, patients with COVID-19 had a longer duration of mechanical ventilation [25].
Another study was conducted by Huniqing Ge et al., regarding the lung mechanics of mechanically ventilated patients with COVID-19 in 2020. The study was conducted in China, where 7 patients were included. It was a retrospective study using the analysis of a respiratory cycle wave form, calculating the compliance and obtaining the outcome from discharge records. Results demonstrated that survivors had increased lung compliance over time whereas non-survivors showed persistently low compliance also it concluded that prone positioning was associated with improve in lung compliance and so improve the outcome [26].
Problem statement
COVID-19 pandemic has been a major concern around the world, with its recent emerge there is no enough information about it and the guidelines of treatment are continuously edited. Patients with COVID-19 who develop ARDS may be very challenging to deal with especially because it is different from non-COVID ARDS, the prediction of the outcome and the different indicators of it is still a place of research. Lung mechanics and its efficacy can affect the outcome of each patient, with a lack of understanding of how it can affect the outcome and prognosis of these patients.
Research question
What is the relation between lung mechanics and prognosis and outcome of ARDS COVI-19 patient?
Justification
Understanding the lung mechanics of the CARDS patients may predict the outcome and improve the medical approach which improves the outcome.
To the best of my knowledge, there were no published studies regarding lung mechanics as a predictor for prognosis in COVID-19 patients who develop ARDS.
Objectives
General objectives: To determent the relation between lung mechanics and outcome and prognosis of ARDS COVID-19 patient.
Specific objectives: To calculate the number of COVID-19 patients above the age of 15 who develop ARDS in Albaraha hospital COVID-19 ICU.
• To measure the PEEP of each patient.
• To measure the Peak airway pressure of each patient.
• To measure the tidal volume of each patient.
• To calculate the lungs compliance of each patient by dividing delivered
tidal volume over the driving pressure.
• To calculate the driving pressure (peak pressure minus the PEEP).
• To assess the outcome and prognosis of each patient through length of
days of intubation and their mortality.
• To assess the relation between high lung compliance and the outcome
of the patient.
• To assess the relation between low lung compliance and the outcome of
the patient.
• To compare the outcome of the patients with low and high compliance.
Materials and Methods
Study design
This is an analytical comparative cross sectional hospital record based.
Study area
This study was conducted in AL-Baraha private hospital located in BAHRI, it’s a large square area and well equipped COVID-19 center.
Study duration
This study was conducted during the period from November 2020 to February 2021.
Study population
The study population of this study was the COVID-19 patients and ARDS who were admitted to Albaraha hospital.
Inclusion criteria
• Adult patient (aged more than 15 years).
• Diagnosed with COVID-19.
• Admitted to ICU.
• Developed ARDS and on the mechanical ventilator.
Exclusion criteria
• Any patient not falling under the inclusion criteria.
• Pregnant patients.
• Patient with obstructive lung diseases.
• Patient with lung fibrosis.
• Patient under the age of 20.
• Patient with collapsed lung partial or all.
Sampling
Total coverage method was used in this study. A number of 50 COVID-19 patients were included in this study. Due to small number of targeted population.
Data collection
Data were collected using a data collection form after obtaining consent from the hospital. The data were collected from the statistic department and from the ICU records of the COVID-19 patients. The researcher was collected the data.
Data analysis
Data were reviewed, ordered then entered into the excel spreadsheets. The Statistical Package for the Social Sciences (SPSS) version 26 was used to analyze the data. The Chi-square test was used to determine the association between the variable and a p-value less than 0.05 was considered as statistically significant. The appropriate tables and figures were used to demonstrate the results.
Study variables
Dependent variables
• Compliance.
• Driving pressure.
• Peak pressure.
• Tidal volume.
• Peep.
Independent variables
• Age.
• Gender.
Results
Socio-demographic characteristics
Age: In this study, the mean age of the participants was 70 years (SD=10) (Table 1 and Figure 3).
| Age distribution | Age |
|---|---|
| N | 50 |
| Minimum | 42 |
| Maximum | 85 |
| Mean | 70.08 |
| Std. Deviation | 10.026 |
TABLE 1: Age distribution among the study participants.
Gender: In this study, most of the study participants were males (72%).
Lung function
Oxygen saturation: The mean Oxygen Saturation (SpO2) in this study was 90.3 (SD=5.5) (Table 2).
| Oxygen saturation | |
|---|---|
| N | 50 |
| Minimum | 69 |
| Maximum | 97.8 |
| Mean | 90.318 |
| Std. Deviation | 5.58463 |
TABLE 2: Oxygen Saturation (SpO2) among the study participants.
Fraction of inspired Oxygen (FiO2): The mean Fraction of inspired Oxygen (FiO2) among the participants was 0.8 (SD=0.18) (Table 3).
| Fraction of inspired oxygen | |
|---|---|
| N | 50 |
| Minimum | 0.36 |
| Maximum | 1.5 |
| Mean | 0.805 |
| Std. Deviation | 0.18799 |
TABLE 3: Fraction of inspired oxygen among the study participants.
Positive end-expiratory pressure: In this study, the mean Positive End-Expiratory Pressure (PEEP) was 14.9 (SD=17.5) (Table 4).
| Positive end-expiratory pressure | |
|---|---|
| N | 50 |
| Minimum | 5 |
| Maximum | 135 |
| Mean | 14.994 |
| Std. Deviation | 17.58952 |
TABLE 4: Positive End-Expiratory Pressure (PEEP) among the study participants.
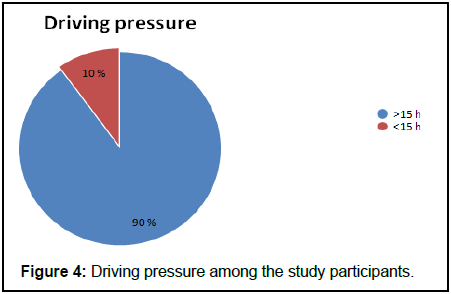
Driving pressure: Figure 4 and Table 5 demonstrates the driving pressure among the study participants. The mean driving pressure among the participants was 19.8 (SD=4.3).
| Driving | |
|---|---|
| N | 50 |
| Minimum | 8.5 |
| Maximum | 30 |
| Mean | 19.8896 |
| Std. Deviation | 4.30412 |
Table 5: Driving pressure among the study participants.
Tidal volume: The mean tidal volume in this study was 452.9 ml (SD=99.6) (Table 6).
| Tidal | |
|---|---|
| N | 50 |
| Minimum | 242.5 |
| Maximum | 691.5 |
| Mean | 452.922 |
| Std. Deviation | 99.63844 |
TABLE 6: Tidal volume among the study participants.
Peak pressure: Among all the participants, the peak pressure was more than 30 cm H2O.
| P peak pressure | Frequency | Percent |
|---|---|---|
| >30 | 50 | 100 |
| <30 | 0 | 0 |
| Total | 50 | 100 |
TABLE 7: Peak pressure among the study participants.
Lung compliance: In this study, 42 (84%) of the participants had low lung compliance (Table 8).
| Frequency | Percent | |
|---|---|---|
| Low | 42 | 84 |
| Normal | 5 | 10 |
| High | 3 | 6 |
| Total | 50 | 100 |
TABLE 8: Lung compliance among the study participants.
Endotracheal intubation
Duration of endotracheal intubation: The mean duration of endotracheal intubation among the study participants was 9.7 days (SD=6.6) (Table 9).
| Duration of intubation (in days) | |
|---|---|
| N | 50 |
| Minimum | 2 |
| Maximum | 33 |
| Mean | 9.7 |
| Std. Deviation | 6.662 |
TABLE 9: Duration of endotracheal intubation (in days) among the study participants.
Outcome: All the study participants in this study were died (Table 10).
| Outcome | Frequency | Percent |
|---|---|---|
| Death | 50 | 100% |
| Other | 0 | 0% |
| Total | 50 | 100% |
TABLE 10: Outcome of the study participants.
Associations
Association between the lung compliance and the duration of endotracheal intubation: This study found no association between the lung compliance and the duration of endotracheal intubation among the study participants (p-value=0.78) (Table 11).
| N | Mean | Std. deviation | p-value | |
|---|---|---|---|---|
| Low | 42 | 9.86 | 7.114 | 0.788 |
| Normal | 5 | 7.8 | 3.899 | |
| High | 3 | 10.67 | 2.887 | |
| Total | 50 | 9.7 | 6.662 |
TABLE 11: Association between the lung compliance and the duration of endotracheal intubation among the study participants.
Association between gender and lung compliance: This study found that there is no statistical association between the gender and lung compliance among the study participants (p-valu=0.61) (Table 12).
| Gender | N | Mean | Std. Deviation | P-Value | |
|---|---|---|---|---|---|
| Compliance | Male | 36 | 25.7639 | 10.56193 | 0.619 |
| Female | 14 | 24.2071 | 7.71626 |
TABLE 12: Association between gender and lung compliance among the study participants.
Association between gender and duration of intubation: This study found no association between the gender and duration of intubation among the study participants (p-value=0.37) (Table 13).
| Gender | N | Mean | Std. Deviation | P-Value | |
|---|---|---|---|---|---|
| Duration of intubation | Male | 36 | 9 | 5.082 | 0.37 |
| Female | 14 | 11.5 | 9.638 |
TABLE 13: Association between gender and duration of intubation among the study participants.
Discussion
The aim of this study is to determent the association between lung mechanics, outcome and prognosis of ARDS COVID-19 patients. The mean Oxygen Saturation (SpO2) was 90.3 (SD=5.5), the mean tidal volume in this study was 452.9 ml (SD=99.6), all the participants had a peak pressure of more than 30 cm H2O. In this study, 42 (84%) of the participants had a low lung compliance. The mean duration of endotracheal intubation among the study participants was 9.7 days (SD=6.6). All the study participants in this study have died. This study found no association between lung compliance and the duration of endotracheal intubation among the study participants (p-value=0.78).
In this study, a number of 50 COVID-19 patients were included in this study. The mean age of the participants was 70 years (SD=10) and most of the study participants were males (72%).
The mean Oxygen saturation (SpO2) in this study was 90.3 (SD=5.5). The optimal Oxygen saturation (SpO2) in adults with COVID-19 who are receiving supplemental oxygen is uncertain. However, a target SpO2 of 92% to 96% seems logical, considering that indirect evidence from patients without COVID-19 suggests that a SpO2<92% or >96% may be harmful [27].
The mean Positive End-Expiratory Pressure (PEEP) was 14.9 (SD=17.5). This finding is comparable to another study conducted by Michael W. Sjoding et al., among COVID-19 patients with ARDS, the mean PEEP was 12 [28]. The mean driving pressure among the participants was 19.8 (SD=4.3). This finding is comparable to another study conducted by Michael W. Sjoding et al., among COVID-19 patients with ARDS, the mean driving pressure was 11.
In this study, 42 (84%) of the participants had low lung compliance. This fining is higher than another study conducted by Daniel Jafari et al., where 538 (34.6%) had very low lung compliance and 982 (63.2%) were with low-normal compliance.
The mean duration of endotracheal intubation among the study participants was 9.7 days (SD=6.6). This Sindings is comparable to another study conducted by, in which the mean duration for endotracheal intubation was 13.5 days.
All the study participants in this study have died. This finding is different from another study conducted by Michael W. Sjoding et al., among COVID-19 patients with ARDS in the USA, in which 57 (44%) of the participants were discharged alive and 39 (30%) died [28]. This difference could be due to the difference of the characteristics of the participants, for example, the mean age in this study was 70 years while it was 64 in the study that conducted by Michael W. Sjoding et al., Moreover, this difference can be due to the difference in health facilities.
This study found that there is no statistical association between the gender and the lung compliance or duration of endotracheal intubation among the study participants. These Sindings are consistent with another study conducted by Antoni Torres et al., which found no association between gender and the prognosis of COVID-19 patients with ARDS [24]. Determining prognostic factors is crucial to detect those that are amenable to medical intervention.
Conclusion
COVID-19 may cause hypoxemic respiratory failure and Acute Respiratory Distress Syndrome (ARDS). Recent data have shown that ARDS related to COVID-19 shares common pathophysiological and clinical features with ARDS of other causes. The mean Oxygen saturation (SpO2) was 90.3, and the mean tidal volume in this study was 452.9 ml. In this study, 42 (84%) of the participants had a low lung compliance. The mean duration of endotracheal intubation among the study participants was 9.7 days. All the study participants in this study have died. This study found no association between the lung compliance and the duration of endotracheal intubation among the study participants. This study also found that there is no statistical association between the gender and lung compliance among the study participants.
Ethical Consideration
• Ethical approval was obtained from the ethical review committee of the
Sudan Medical Specialization Board (SMSB) and from research unit
EDC.
• Ethical clearance will be obtained from hospital administration.
• Confidentiality will be ensured by the researcher by not mentioning the patient’s name.
Recommendations
Further studies should be conducted with cohort study design, larger sample size.
References
- Worldmeter.com. COVID Live Update: 186,356,010 Cases and 4,026,894 Deaths from the Coronavirus. Updated December 1, 2021.
- Cennimo DJ, Bergman SJ, Olsen KM. Coronavirus Disease 2019 (COVID-19): Practice Essentials, Background, Route of Transmission. Medscape. Jun 12, 2023.
- Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: The Berlin definition. JAM: J Am Med Assoc. 2012 Jun 13;307(23):2526–33.
- Sterling G. Ventilation. Br J Clin Pharmacol. 1979;8(6):513–21.
- Ball CM, Wilkinson DJ. History of Airway Management. Hagberg and Benumof’s Airway Management. Elsevier Inc.; 2018:270–86.
- Acosta P, Santisbon E, Varon J. “The Use of Positive End-Expiratory Pressure in Mechanical Ventilation. Crit Care Clin; 2007;23:251–61.
- Marshall R. The physical properties of the lungs in relation to the subdivisions of lung volume. Clin Sci. 1957;16(3):507–15.
- Chaudhry R, Bordoni B. Anatomy, Thorax, Lungs. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023.
[PubMed]
- Brinkman JE, Sharma S. Physiology, Pulmonary. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023.
[PubMed]
- Brinkman JE, Toro F, Sharma S. Physiology, Respiratory Drive. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023.
[PubMed]
- Lutfi MF. The physiological basis and clinical significance of lung volume measurements. Multidiscip Respir Med. 2017;12(3).
[Crossref] [Google Scholar] [PubMed]
- World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes it. Department of Human Service. 2020.
- Cennimo DJ, Bergman SJ, Olsen KM. Coronavirus Disease 2019 (COVID-19): Practice Essentials, Background, Route of Transmission. Medscape. May 18, 2021.
- Coronavirus (COVID-19). NHS. May 18, 2021.
- World Health Organization (WHO). Fact sheet-Information for visitors (produced by WHO/Europe). 2020.
- Gousseff M, Penot P, Gallay L, et al. Clinical recurrences of COVID-19 symptoms after recovery: Viral relapse, reinfection or inflammatory rebound?, J Infect. 2020;81(5):816–46.
[Crossref] [Google Scholar] [PubMed]
- Barlow A, Landolf KM, Barlow B, et al. Review of Emerging Pharmacotherapy for the Treatment of Coronavirus Disease 2019. Pharmacotherapy. 2020;40(5):416-37.
[Crossref] [Google Scholar] [PubMed]
- Feather A, Randall D, Waterhouse M. Kumar and Clark's Clinical Medicine. 10th Edition. Elsevier; 2020.
- Shrestha GS, Khanal S, Sharma S, et al. COVID-19: Current Understanding of Pathophysiology. J Nepal Health Res Counc. 2020;18(3):351–9.
[Crossref] [Google Scholar] [PubMed]
- Huang D, Ma H, Xiao Z, et al. Diagnostic value of cardiopulmonary ultrasound in elderly patients with acute respiratory distress syndrome. BMC Pulm Med. 2018;18(1):136.
[Crossref] [Google Scholar] [PubMed]
- Gajic O, Dabbagh O, Park PK, et al. Early identification of patients at risk of acute lung injury: Evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med. 2011;183(4):462–70.
[Crossref] [Google Scholar] [PubMed]
- Guerin C, Reignier J, Richard JC, et al. Prone Positioning in Severe Acute Respiratory Distress Syndrome. N Engl J Med. 2013;368(23):2159–68.
[Crossref] [Google Scholar] [PubMed]
- Aoyama H, Yamada Y, Fan E. The future of driving pressure: a primary goal for mechanical ventilation? J Intensive Care. 2018;6(1):64.
[Crossref] [Google Scholar] [PubMed]
- Torres A, Motos A, Riera J, et al. The evolution of the ventilatory ratio is a prognostic factor in mechanically ventilated COVID-19 ARDS patients. Crit Care. 2021;25(1):331.
[Crossref] [Google Scholar] [PubMed]
- Bain W, Yang H, Shah FA, et al. COVID-19 versus Non–COVID-19 acute respiratory distress syndrome comparison of demographics, physiologic parameters, inflammatory biomarkers, and clinical outcomes. Ann Am Thorac Soc. 2021;18(7):1202–10.
[Crossref] [Google Scholar] [PubMed]
- Jafari D, Gandomi Sereshki A, Makhnevich A, et al. Trajectories of Hypoxemia and Respiratory System Mechanics of COVID-19 ARDS in the NorthCARDS Dataset. American Thoracic Society. 2021.
- WHO. Living guidance for clinical management of COVID-19. Department of Human Health Service. Updated November 23, 2021.
- Sjoding MW, Admon AJ, Saha AK, et al. Comparing Clinical Features and Outcomes in Mechanically Ventilated Patients with COVID-19 and Acute Respiratory Distress Syndrome. Ann Am Thorac Soc. 2021;18(11):1876–85.
[Crossref] [Google Scholar] [PubMed]