Lymphatic Fistula and Granuloma in Vein Glue VenaSeal«
Received: 20-Oct-2020 Accepted Date: Nov 04, 2020; Published: 11-Nov-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Lymph fistula and granuloma: All catheter-based procedures for the treatment of varicose veins can result in injuries to the lymphatic system when the vessel is punctured and the catheter is inserted. This leads to the development of a lymph fistula in approx. 2-4% of the therapeutic cases.Lymphatic water is pressed through a small opening in the wound to the surface of the skin.Keywords
Lymphatic fistula, Vein glue, Lymphatic fistula
Introduction
We have been using the vein glue VenaSeal® since August 2012. In the last 98 months we have ablated 2836 varicose veins in 1474 patients with the vein glue. In 26 ablated veins (0.9%) we saw a postoperative lymphatic fistula, in 4 cases a granuloma (glue pimple) had to be removed after 10 months-12 months [1-3].
All catheter-based procedures for the treatment of varicose veins can result in injuries to the lymphatic system when the vessel is punctured and the catheter is inserted. This leads to the development of a lymphatic fistula in approx. 2%-4% of the therapeutic cases. Lymphatic water is pressed through a small opening in the wound to the surface of the skin. We also saw lymph fistulas in the vein glue VenaSeal® after puncturing the vessel.
Case Study
These were additionally promoted by glue granulomas residues remaining in the tissue. It is therefore important, particularly when using the vein glue, to ensure that the puncture site is worked properly and that the sealing maneuver is individually defined for the patient (Figure 1).
Lymphatic fistulas and granulomas in vein glue: The lymphatic fistula
The lymphatic fistula mostly occurs as a complication after surgery. The frequency is around 2%-4%. A lymph fistula can form, especially during operations in body regions with many lymphatic vessels. Lymphatic fluid is increasingly secreted via the injured lymphatic system, which can then escape through the wound. Lymphatic fluid emerges from the fistula. The amount of liquid can increase, especially in the warm season. Germs can enter the body through the lymph fistula, causing erysipelas-a bacterial infection of the lymphatic system-to form. Disinfection and sterile covering of the lymph fistula is therefore very important as a first measure. Since protein is also lost through the lymphatic fistula the primary goal is to close the fistula [4-6].
The escaping lymph is difficult to handle for the patient in many cases and is associated with a loss of quality of life. Wound healing is also delayed. The treatment options for a lymph fistula in vein glue and other catheter procedures are versatile. They range from a tight compression bandage to prophylactic adhesive bonding and surgical refurbishment to radiation therapy (especially for lymph fistulas in the groin region). Also, the glue granuloma must be removed in any case, since it is often the cause of the wound healing disorder [7].
Lymphatic fistulas and granulomas in vein glue: The granuloma
Granulomas (‘granules’) are nodular in medicine-or granular accumulation of the phagocytes of the immune system (macrophages). A granuloma can contain other cells: epithelioid cells and multinucleated giant cells are descendants of the macrophages and accompanying immunologically active lymphocytes, granulocytes and fibroblasts can be involved in the formation of granulomas. Some granulomas develop a connective tissue capsule (fibrosis) others have necrosis (dead tissue) in their center. Granulomas develop when the macrophages are unable to break down poison or a foreign substance (e.g. bacteria, parasites or foreign bodies), which causes chronic inflammatory irritation. The purpose of granuloma is to encapsulate the intruder foreign to the body and this prevent it from spreading further. In addition, pathogens or foreign substances can be controlled more effectively by locally concentrating enzymes and bactericidal substances [8].
The clinical picture is characterized by local inflammatory redness and tenderness to pressure. Wounds cannot heal, bloody or lymphatic fluid is secreted. We opened and completely cleared out all 4 granulomas. We had the tissue material examined pathologically and histologically-after 10-14 months no more vein glue residues were found. The vein walls could no longer be identified, remnants of muscle fibers of the vein walls as well as many leukocytes, lymphocytes, granulocytes and macrophages could be made visible (Figure 2).
Results and Discussion
Lymphatic fistula and granuloma in vein glue
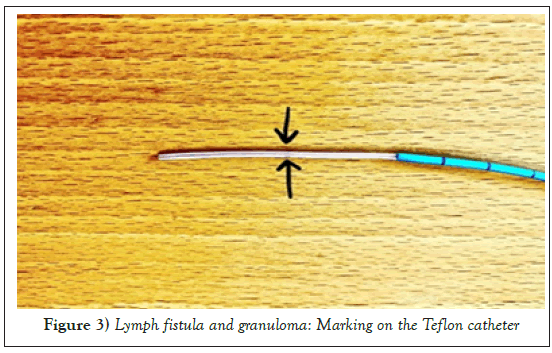
The two described side effects with vein glue are avoidable: As can be clearly seen in the image below of a VenaSeal®-catheter and has also been marked by us, there is a black marking point on the Teflon glue catheter. This is intended to mark the maximum point at which the glue can be dispensed into the container. The only problem is that the distance between skin and vessel is not 2.5 cm for every patient [9].
Particularly strong patients, obese patients and also lymphedema patients often have much greater distances from the skin to the blood vessel. Means: The surgeon has to decide individually for each individual patient up to which catheter length a glue injection is possible. This extensive individualization of the therapy almost certainly prevents the glue from being incorrectly released into the tissue, with the subsequent formation of lymphatic fistula [10-13].
Furthermore, the last dispensing of glue has to be modified in such a way that it waits until the glue has polymerized (approx. 30 sec), and then the catheter is removed vigorously, quickly, and in one go. So, there is no glue thread between the skin ends of the puncture site (Figure 3).
Lymphatic fistula and granuloma in vein glue
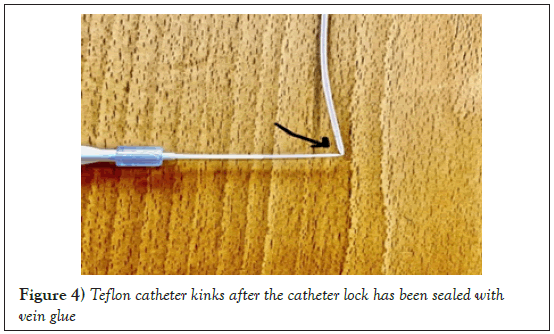
The first point: After removal of the Teflon catheter the tip has vein glue deposits, which should actually remain in the container. Furthermore, it becomes clear that pulling back the Teflon catheter into the vascular lock (blue) on the one hand pushes the vein glue (which remains in the tissue), but on the other hand, glue is also pulled into the lock. The second point, in particular, is extremely important! Pulling the glue into the introducer sheath creates a tight seal on this catheter within 15 seconds. This means that it can no longer be used. The picture below clearly shows that the soft catheter can no longer pass through the lock and there is a kink closure. The result is an unusable sheath and an unusable Teflon catheter (Figure 4).
Conclusion
This means that the surgeon has to open a new catheter for the next vein- another € 1200 is wasted. In addition to the risk of the described side effects of lymphatic fistula and granuloma due to residues of vein glue, there is also a completely unnecessary consumption of a new catheter system. And the change in the technical processes that the manufacturer is considering-the retraction of the catheter into the sheath still in the vein being treated-does not change here. The glue also adheres to the outer skin of the lock and is deposited as lumps when pulled out into the tissue.
You can see this also at youtube-channel of Saphenion®-https://youtu.be/ liXce6pA7BE.
Great thanks to Frau Dr. Lili Marell and Dr. Wolfgang Lahl for the heavy support!
Disclosure
There is no any potential conflict of interests
REFERENCES
- Gibson K, Minjarez R, Gunderson K, et al. Need for adjunctive procedures following cyanoacrylate closure of incompetent great, small and accessory saphenous veins without the use of postprocedure compression: Three-month data from a postmarket evaluation of the VenaSeal System (the WAVES Study). Phlebology. 2019; 34(4):231-7.
- Kolluri R, Chung J, Kim S, et al. Network meta-analysis to compare VenaSeal with other superficial venous therapies for chronic venous insufficiency. J Vasc Surg Venous Lymphat Disord. 2020; 8(3):472-81.e3.
- Morrison N, Gibson K, McEnroe S, et al. Randomized trial comparing cyanoacrylate embolization and radiofrequency ablation for incompetent great saphenous veins (VeClose). J Vasc Surg. 2015; 61(4):985-94.
- Park I. Initial Outcomes of Cyanoacrylate Closure, VenaSeal System, for the Treatment of the Incompetent Great and Small Saphenous Veins. Vasc Endovascular Surg. 2017; 51(8):545-9.
- Park I, Kim D. Correlation Between the Immediate Remnant Stump Length and Vein Diameter After Cyanoacrylate Closure Using the VenaSeal System During Treatment of an Incompetent Great Saphenous Vein. Vasc Endovascular Surg. 2020; 54(1):47-50.
- Gibson KD, Minjarez R, Rinehardt E, et al. Frequency and severity of hypersensitivity reactions in patients after VenaSealTM cyanoacrylate treatment of superficial venous insufficiency. Phlebology. 2019; 35(5):026835551987861
- Lam YL, Maeseneer MD, Lawson J, et al. Expert review on the VenaSeal® system for endovenous cyano-acrylate adhesive ablation of incompetent saphenous trunks in patients with varicose veins. Expert Review of Medical Devices. 2017; 14(10):1378093.
- Christof MS, Christina G, Götz MR. Postoperative therapierefraktäre Lymphfistel mit Wundheilungsstörung. Dtsch Arztebl Int. 2018; 115:376.
- Ohlbauer M, Mildner A, Brenner E, et al. Lymphzysten und Fisteln nach Varizenoperationen. Lymphologie in Forschung und Praxis. 2000; 4:11-14.
- Von Dr. med. Jörg Fuchs. Krampfadern: Behandlungsmethoden im Vergleich. 2014.
- Zierau UT. SaphenionScience-90 months vein glue in 1365 cases. 2020.
- Zierau UT. SaphenionFactCheck-Vein glue for varicose veins/update 8. 2019.
- Zierau UT. SaphenionPatientenInfo: 8 Jahre Venenkleber-Therapie mit Cyanoacrylat-BioKleber. 2020.