Management of inadvertent mesenteric hematoma during total radical colectomy
2 Department of GI and HPB Surgery, Sterling Hospital, Ahmedabad, Gujarat, India
Received: 23-May-2018 Accepted Date: Jul 16, 2018; Published: 23-Jul-2018
Citation: Chavda HJ, Vasoya BC. Management of inadvertent mesenteric hematoma during total radical colectomy. Surg Case Rep. 2018;2(2):26-7.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
BACKGROUND: Any inadvertent bleeding during surgery is difficult to manage despite of availability of many hemostatic instruments like diathermy, ligasure, harmonic scalpel and other vessel sealing devices. Usually it is difficult to identify and control the actively bleeding artery at the route of the mesentery causing expanding hematoma and hemodynamic instability. Angioembolization is a better option over surgical exploration of hematoma in such situations. CASE PRESENTATION: A 76-year-old gentleman had carcinoma of rectum with synchronous growth in ascending and descending colon. He underwent total radical colectomy. Inadvertent bleeding from the middle colic artery causing expanding hematoma at root of mesentery was controlled with angioembolisation. DISCUSSION: Most of the mesenteric hematoma does not require any intervention. Active bleeding with hemodynamic instability warrants urgent intervention like angioembolisation or surgery. CONCLUSION: Exploration of mesenteric hematoma to control the bleeding artery is technically very difficult due to hypotension and hemodynamic instability. Urgent angioembolization to locate and control the bleeding is the safer and better option in such conditions.
Keywords
Mesenteric hematoma; Angioembolisation; Colon; Cancer
Any inadvertent bleeding during surgery is difficult to manage despite of availability of many hemostatic instruments like diathermy, ligasure, harmonic scalpel and other vessel sealing devices1. Usually it is difficult to identify and control the actively bleeding artery at the route of the mesentery causing expanding hematoma and hemodynamic instability. Angioembolization is a better option over surgical exploration of hematoma in such situations [1,2].
Case Presentation
A 76-year-old gentleman had carcinoma of rectum with synchronous growth in ascending and descending colon. He underwent total radical colectomy. Procedure went uneventful. Immediately after extubation abdominal drain accumulated approx. 500 ml of fresh blood which indicated active hemorrhage and urgent re-exploration was done. There was collection of 700 ml blood in peritoneal cavity and an active venous bleeding from superior mesenteric vessels territory. The bleeding was controlled with 5-0 prolene sutures.
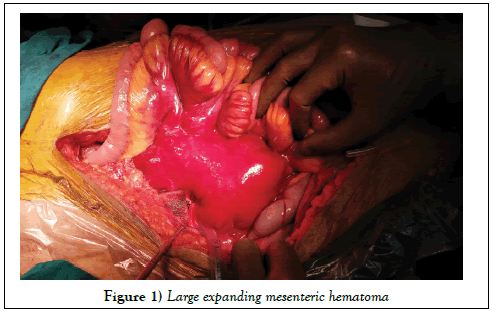
During observation there was a mesenteric hematoma at the suture site of size 5 × 5 cm. It started expanding and reached up to size of 10 × 10 cm within 20 minutes without any identifiable active bleeding due to bulky fat pad and hematoma (Figure 1).
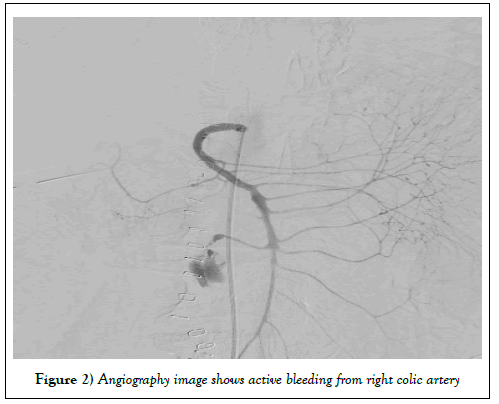
We realized that the arterial knot probably slipped off and the open end of the artery got retracted under the fat pad and was unidentifiable due to the bulky fat pads. Blood products were given as needed and he required inotropic support during this period. After stabilization of patient, he was shifted to cathlab and an urgent angioembolization was planned. During angiography there was an active bleeding from right colic artery branch (Figure 2).
Figure 2: Angiography image shows active bleeding from right colic artery
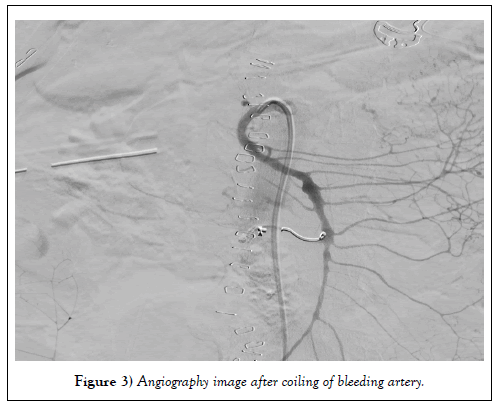
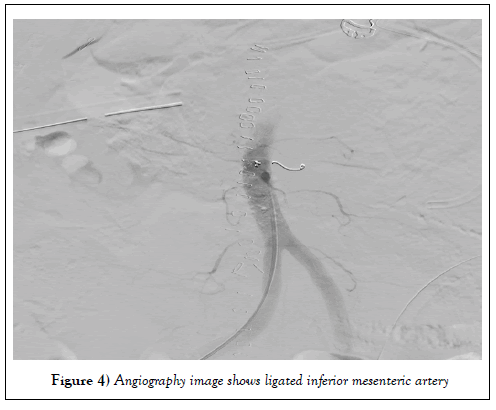
An angioembolization was done with coil and glue. Post embolization angiography shows no active bleeding (Figures 3 and 4).
Figure 3: Angiography image after coiling of bleeding artery.
Figure 4: Angiography image shows ligated inferior mesenteric artery
Patient was kept in intensive care unit for one day and on day two he was shifted to ward. On post-operative day seven he was discharged without any post-operative complications.
Discussion
Mesenteric hematoma is known to occur in blunt abdominal trauma, as a complication of pancreatitis, coagulation disorder or anticoagulant therapy, connective tissue disorder or mesenteric vascular aneurysm [2-5]. Most of the mesenteric hematoma are managed by conservative approach. The route of the mesentery is usually bulky due to fat pads and it is technically difficult to palpate and locate the active arterial bleeding due to the tense hematoma in this region. If the patient becomes hemodynamically unstable due to ongoing active bleeding and expanding hematoma, it may require intervention in form of angioembolisation or open surgery. Angioembolization is a safe option before subjecting patient to open surgery [6]. Most of the mesenteric hematoma does not require any intervention. Active bleeding with hemodynamic instability warrants urgent intervention.
The role of angioembolization in upper gastro intestinal bleeding is well documented, even in failure of endoscopic intervention [7-9]. If there is no other indication of surgery or if there is no intraperitoneal bleeding and the expanding hematoma is recognized during the surgery, the patient should undergo urgent angiography to locate the source of bleeding and subsequent angioembolization to control the bleeding. As in our case it is difficult to find out active bleeding during surgery particularly if the hematoma is expanding rapidly under the fat pad at the route of the mesentery. Angioembolization is a safer option than exploring the hematoma and finding bleeder in mashie surgical field.
Conclusion
There has been a significant advancement in different hemostatic devices and newer hemostatic agents during last two decades [9]. In the described situations it is difficult to locate the bleeding artery due to the expanding hematoma (Figure 1) in mesenteric fat pad. Exploration of mesenteric hematoma to control the bleeding artery is technically very difficult due to hypotension and hemodynamic instability. Urgent angioembolization to locate and control the bleeding is the safer and better option in such conditions.
Conflicts of Interest
All authors disclose financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work.
Funding
No source of funding or sponsors.
REFERENCES
- Gruen RL, Brohi K, Schreiber M, et al. Haemorrhage control in severely injured patients. The Lancet. 2012;380(9847):1099-108.
- DeBrito P, Gomez MA, Besson M, et al. hematoma: unusual complication of a long term oral anticoagulation therapy. Ann Chir. 2006;131(9)529-532.
- Parent BA, Cho SW, Buck DG, et al. Spontaneous rupture of hepatic artery aneurysm associated with polyarteritis nodosa Am Surg. 2010;76 (12)1416-1419.
- Parker SG, Thompson JN. Spontaneous mesenteric haematoma; diagnosis and management BMJ Case Rep. 2012;1-3.
- Toyonaga T, Nagaoka S, Ouchida K, et al. Case of a bleeding pseudoaneurysm of the middle colic artery complicating acute pancreatitis Hepatogastroenterology. 2002;49(46)1141-1143.
- Ghelfi J, Frandon J, Barbois S, et al. Arterial Embolization in the Management of Mesenteric Bleeding Secondary to Blunt Abdominal Trauma Cardiovasc Intervent Radiol. 2016;39: 683.
- Goldman ML, Land WC, Bradley III EL, et al. Transcatheter therapeutic embolization in the management of massive upper gastrointestinal bleeding. Radiology. 1976;120:513-521.
- Aina R, Oliva VL, Therasse É, et al. Arterial embolotherapy for upper gastrointestinal hemorrhage: outcome assessment. J Vasc Interv Radiol. 2001;12:195-200.
- Ljungdahl M, Eriksson LG, Nyman R, et al. embolization in management of massive bleeding from gastric and duodenal ulcers. Eur J Surg. 2002;168:384-390.