May angina and myocardial wall motion disorder be a sign of lung cancer: the rescue role of cardiac PET
Received: 16-Sep-2022, Manuscript No. PULCJ-22-5238; Editor assigned: 19-Sep-2022, Pre QC No. PULCJ-22-5238(PQ); Accepted Date: Sep 29, 2022; Reviewed: 22-Sep-2022 QC No. PULCJ-22-5238(Q); Revised: 25-Sep-2022, Manuscript No. PULCJ-22-5238(R); Published: 30-Sep-2022, DOI: 10.37532/pulcj.22.6(5).61-62
Citation: Cakir B, GOK M, Altay S. May angina and myocardial wall motion disorder may be a sign of lung cancer: The rescue role of cardiac PET. Clin Cardiol J. 2022; 6(5):61-62.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Cardiac nuclear imaging is one of the most commonly used imaging methods today to investigate myocardial ischemia or viable tissue in patients with suspected coronary artery disease. There are many studies on extracardiac finding scans in these images taken as tomographic sections. However, there is no report in the literature regarding the extracardiac findings encountered during 18 Fluoro-2-Deoxyglucose (18F-FDG) cardiac Positron Emission Tmography (PET), which is a metabolic evaluation. In this case report, we discussed a case who presented with chest pain, had myocardial wall motion disorder but did not have significant coronary artery stenosis, and was diagnosed with incidental lung cancer on myocardial 18F-FDG PET imaging taken during cardiac evaluation.
Keywords
Cardiac 18F-FDG PET; Lung cancer; Myocardial viability; Normal coronary arteries; Wall motion disorder
Introduction
The presence of viable tissue in myocardial segments with decreased perfusion observed in imaging methods is an important entity in terms of determining the reperfusion strategy. 18F-FDG PET has recently been used as a gold standard method to detect metabolic activity and viable tissue presence in these regions[1]. Acting as a glucose analog, 18F-FDG is also frequently used in oncological imaging due to increased tumoral metabolic activity [2]. In the case report that clinical details are given below, a patient who presented with chest pain and had apical hypokinesia on Transthoracic Echocardiography (TTE), and observed an incidental metabolic active mass in the lung in 18F-FDG cardiac PET imaging which performed to investigate myocardial viability is presented.
Case Presentation
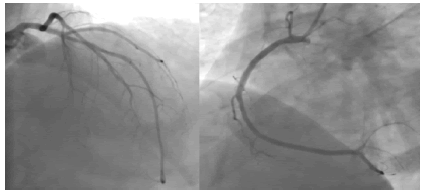
A 58-year-old male patient with a known history of hypertension was admitted to the cardiology outpatient clinic with chest pain triggered by exertion. Two years ago, the patient underwent Coronary Angiography (CAG) because of Left Ventricule (LV) Ejection Fraction (EF) 54% and apical hypokinesia on TTE. CAG showed 40% stenosis in the left anterior descending artery, and a decision was made for medical follow-up. Since then, the patient has frequently been admitted to the emergency room and chest diseases outpatient clinic with complaints of chest pain and cough (Figure 1).
Figure 1: Stenosis in the Left Anterior Descending Artery
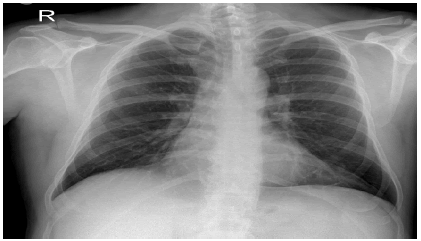
No pathological finding was observed in the chest X-rays taken during these periods (Figure 2). In the control TTE performed at the current admission of the patient, the EF was 38%, and the apex and anterior region were hypokinetic. Myocardial Perfusion Scintigraphy (MPS) was performed to investigate ischemia, and 30% mixed perfusion defect was detected in the anterior area.
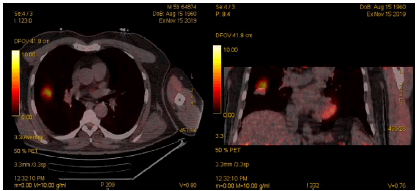
In 18F-FDG PET performed for the evaluation of myocardial viable tissue, 15% viable tissue and 15% non-viable tissue were observed in the area with perfusion defect. At the same time, increased FDG uptake was observed in a 2 cm soft tissue lesion in the lateral part of the right lung middle lobe on PET imaging (Figure 3). Thoracic Computed Tomography (CT) was performed on the patient, who was thought to have a possible lung malignancy, and he was referred to Thoracic Surgery after a mass was observed in the middle lobe of the right lung. With the preliminary diagnosis of lung cancer, the patient underwent left middle lobectomy and mediastinal lymph node dissection. In the pathological examination of the biopsy materials, a diagnosis of lung invasive adenocarcinoma was made. It was evaluated as stage 1c because there was no invasion in the lymph nodes and there was no distant tissue metastasis. Cure was achieved after postoperative carboplatin and paclitaxel treatment and radiotherapy application. In the first year follow-up of the patient, it was observed that EF increased to 48% and anterior hypokinesia persisted in the apical sections in TTE and coronary arteries were normal in coronary CT angiography.
Discussion
Many times so far, extracardiac findings encountered during various cardiac imaging methods have been reported or malignancy screening studies have been performed in these imaging studies. In cardiac PET imaging, extracardiac findings and malignancy screening were generally performed in perfusion imaging. In a study of 1397 patients in 2017, tomographic images were scanned in patients who underwent myocardial perfusion PET/CT, and 10% found extracardiac findings with the potential to be associated with chest pain. In addition, 1.4% of these patients had a newly diagnosed malignant disease, the majority of which was lung cancer. Regarding myocardial 18F-FDG PET imaging for metabolic evaluation, no extracardiac finding has been reported before[3,4].
The most important marker showing that a cell is alive is the continuation of its metabolic activity. There is a perfusion defect in the hibernated myocardial tissue during stress and rest, but myocytes continue their metabolic activities. Based on this, 18FFDG, which acts as a glucose analogue, has been used in nuclear medicine to investigate myocardial viability [1]. It is also used in oncological studies due to the increased metabolic activity of malignant tumors. These two different usage areas have different protocols. In the investigation of myocardial viability, glucose load is applied to the patient to encourage the use of glucose in the myocardium and then images are taken. In oncological imaging, imaging is performed during fasting to promote myocardial fatty acid utilization and thus increase glucose uptake of tumoral regions[2]. Therefore, the case presented is noteworthy because of the detection of malignancy in a metabolic PET performed in the myocardial protocol [5].
Chest pain is seen as a clinical symptom of many diseases. Although sometimes the additional findings observed in the patient lead the clinician to a specific diagnosis, other possible etiologies should definitely be kept in mind. In the presented case, although the patient's chest pain and wall motion disorder in TTE suggest CAD in the preliminary diagnosis, lung cancer is a potential cause of chest pain. In addition, a remarkable feature of the presented case is the absence of an explanatory lesion on coronary angiography or coronary CT angiography despite the presence of regional anterior and apical hypokinesia. No apparent cause was found in the etiology of regional wall motion disorder in this patient. Oncological patients may present with Q-wave myocardial infarction without explanatory lesion on coronary angiography due to increased hypercoagulability [4]. It is possible that the presented patient may have had a silent myocardial infarction due to thrombus during this period or the presence of microvascular disease due to hypercoagulation.
References
- Kobylecka M, Mączewska J, Fronczewska-Wieniawska K, et al. Myocardial viability assessment in 18FDG PET/CT study (18FDG PET myocardial viability assessment). Nucl Med Rev. 2012;15(1):52-60. [Google Scholar] [CrossRef]
- Cook GJ, Wegner EA, Fogelman I. Pitfalls and artifacts in 18FDG PET and PET/CT oncologic imaging. In Semin Nucl Med. 2004;34(2):122-33. [Google Scholar] [CrossRef]
- Kan H, Zant FM, Wondergem M, et al. Incidental extra-cardiac findings on 13N-ammonia myocardial perfusion PET/CT. J Nucl Cardiol. 2017;24(6):1860-68. [Google Scholar] [CrossRef]
- Abid L, Bahloul A, Frikha Z, et al. Myocardial infarction and normal coronary arteries: the experience of the cardiology department of Sfax, Tunisia. Intern Med. 2012;51(15):1959-67. [Google Scholar] [CrossRef]
- Ngozi SC, Ernest NE. Long-term smoking results in haemostatic dysfunction in chronic smokers. Niger Med J: J Niger Med Assoc. 2014;55(2):121. [Google Scholar] [CrossRef]