Meckel’s diverticulum – a case study
Sandhyarani M.Patil1* and Mahadeo Ramchandra Patil2
1Department of Anatomy, Rajarshi Chhatrapati Shahu Maharaj Goverment Medical College,Kolhapur, India.
2Department of Surgery, Dr. D. Y. Patil Medical College,Kolhapur, India.
- *Corresponding Author:
- Dr. Sandhyarani M. Patil, MS
Assistant Professor, Department of Anatomy Rajarshi Chhatrapati Shahu Maharaj Govt. Medical College, Kolhapur, India.
Tel: +91 982 2286190
E-mail: drsandhyapatil.2009@gmail.com
Date of Received: March 27th, 2012
Date of Accepted: October 23rd, 20121
Published Online: April 21st, 2013
© Int J Anat Var (IJAV). 2013; 6: 66–67.
[ft_below_content] =>Keywords
Meckel’s diverticulum,congenital,gastrointestinal tract
Introduction
The Meckel’s diverticulum or diverticulum ilei is the most common unusual congenital condition of gastrointestinal tract. It is present in fetal life as the vitello-intestinal duct, which usually disappears later in seventh week of gestational period.
The incidence of Meckel’s diverticulum in the general population has been estimated to be about 2% [1]. Reports from autopsy and retrospective studies range from 0.14-4.5% [2,3].
Although Meckel’s diverticulum occurs in both sexes, it may cause complications more frequently in males, and therefore is often diagnosed in males [4–6].
Ninety per cent of diverticula are within 90 cm of distance to the ileocaecal valve, although diverticula up to 180 cm from ileocaecal valve have been observed. A person with Meckel’s diverticulum has 4-6% lifetime risk of developing a complication [7]. The major complications are diverticulitis and perforation [6].
Case Report
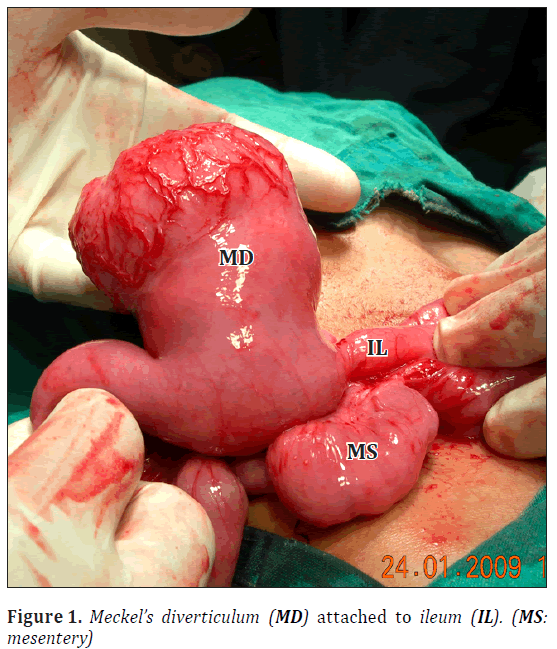
Ten-year-old boy was operated for appendectomy in the Department of Surgery at Chhatrapati Shahu Maharaj Goverment Medical College. On examination of bowel, Meckel’s diverticulum was found. It was removed and the specimen of Meckel’s diverticulum was processed for histological study, where it was stained with hematoxylin and eosin. Following features were noted: the Meckel’s diverticulum was seen at 22 cm proximal to ileocaecal junction; it was 4.3 cm in length with broad tip; it was 3 cm in diameter; it was attached to the antimesentric border of ileum; its tip had no attachment via fibrous band to umbilicus (Figure 1).
Histology
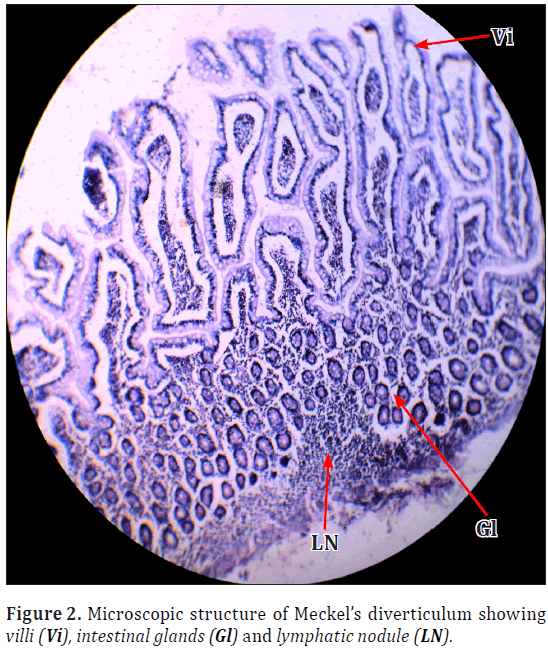
The mucus membrane showed villi. The villi were lined by simple columnar epithelium with goblet cells. The lamina propria showed glands along with isolated lymphatic nodule. Submucosa was present. Muscle layer consisted of inner circular and outer longitudinal layer and outermost serosa (Figure 2).
Discussion
Developmentally the vitelline duct connects the yolk sac and midgut of the embryo at an early stage in fetal life for nutrition [5]. Thus, in the 3 week old embryo the yolk forms the ventral aspect of the gut and communicates through a wide, short vitelline duct, which subsequently becomes absorbed. The blood supply to the vitelline duct comes from paired ventral branches of the abdominal aorta, the vitelline arteries.
If this duct does not involute by 7th week of gestation, various developmental remnants may be left. Failure of most proximal portion of duct to obliterate results in a Meckel’s diverticulum [8]. The yolk sac is continuous with the embryo and contains all layers of the intestinal wall [8].
Meckel’s diverticulum may remain completely asymptomatic, or it may mimic disorders such as Crohn’s disease, appendicitis and peptic ulcer disease. Ectopic tissue found in approximately 50% of cases consists of gastric tissue in 60-65% of cases and pancreatic tissue in 5-16% [9].
Meckel’s diverticulum occurs more commonly in individuals born with other congenital malformations especially exomphalos, esophageal atresia, anorectal atresia and gross malformations of the cardiovascular and central nervous system [9]. Hemingway and Allisan reported an association between angiodysplasia of the caecum and ascending colon with Meckel’s diverticulum in five patients aged between 13 and 21 years [10].
Knowledge of Meckel’s diverticulum is important for surgeons to avoid complications during various abdominal surgeries. It is also important for radiologists while doing ultrasound examination and evaluating radiographs.
References
- Standring S, ed. Gray’s Anatomy. The anatomical basis of clinical practice. 39th Ed., London, Elsevier Churchill Livingstone. 2005; 1167.
- Lüdtke FE, Mende V, Köhler H, Lepsien G. Incidence and frequency of complications and management of Meckels diverticulum. Surg Gynecol Obstet. 1989; 169: 537–542.
- DiGiacomo JC, Cottone FJ. Surgical treatment of Meckel’s diverticulum. South Med J. 1993; 86: 671–675.
- Arnold JF, Pellicane JV. Meckel’s diverticulum: a ten year experience. Am Surg. 1997; 63: 354–355.
- Mackey WC, Dineen P. A fifty year experience with Meckel’s diverticulum. Surg Gynecol Obstet. 1983; 156: 56–64.
- Cullen JJ, Kelly KA, Moir CR, Hodge DO, Zinsmeister AR, Melton LJ 3rd. Surgical management of Meckel’s diverticulum. An epidemiologic, population-based study. Ann Surg. 1994; 220; 564–569.
- Williams RS. Management of Meckel’s diverticulum. Br J Surg. 1981; 68: 477–480.
- Moore KL, Persaud TVN. The Developing Human. 5th Ed., Philadelphia, Saunders. 1993; 255–257.
- Elsayes KM, Menias CO, Harvin HJ, Francis IR. Imaging manifestations of Meckel’s diverticulum. AJR Am J Roentgenol. 2007; 189: 81–88.
- Simms MH, Corkery IJ. Meckel’s diverticulum; a clinical and histological study. Acta Chir Scand. 1959; 248 (Suppl 10): 1.
Sandhyarani M.Patil1* and Mahadeo Ramchandra Patil2
1Department of Anatomy, Rajarshi Chhatrapati Shahu Maharaj Goverment Medical College,Kolhapur, India.
2Department of Surgery, Dr. D. Y. Patil Medical College,Kolhapur, India.
- *Corresponding Author:
- Dr. Sandhyarani M. Patil, MS
Assistant Professor, Department of Anatomy Rajarshi Chhatrapati Shahu Maharaj Govt. Medical College, Kolhapur, India.
Tel: +91 982 2286190
E-mail: drsandhyapatil.2009@gmail.com
Date of Received: March 27th, 2012
Date of Accepted: October 23rd, 20121
Published Online: April 21st, 2013
© Int J Anat Var (IJAV). 2013; 6: 66–67.
Abstract
This paper presents and describes a case of Meckel’s diverticulum. It was found in 10-year-old boy who was operated for appendectomy in surgery department. It was located 24 cm proximal to the ileocaecal junction. It was 4.3 cm in length with broad tip and 3 cm in diameter. It was attached to antimesentric border. The tip was not attached by any fibrous band to umbilicus.
-Keywords
Meckel’s diverticulum,congenital,gastrointestinal tract
Introduction
The Meckel’s diverticulum or diverticulum ilei is the most common unusual congenital condition of gastrointestinal tract. It is present in fetal life as the vitello-intestinal duct, which usually disappears later in seventh week of gestational period.
The incidence of Meckel’s diverticulum in the general population has been estimated to be about 2% [1]. Reports from autopsy and retrospective studies range from 0.14-4.5% [2,3].
Although Meckel’s diverticulum occurs in both sexes, it may cause complications more frequently in males, and therefore is often diagnosed in males [4–6].
Ninety per cent of diverticula are within 90 cm of distance to the ileocaecal valve, although diverticula up to 180 cm from ileocaecal valve have been observed. A person with Meckel’s diverticulum has 4-6% lifetime risk of developing a complication [7]. The major complications are diverticulitis and perforation [6].
Case Report
Ten-year-old boy was operated for appendectomy in the Department of Surgery at Chhatrapati Shahu Maharaj Goverment Medical College. On examination of bowel, Meckel’s diverticulum was found. It was removed and the specimen of Meckel’s diverticulum was processed for histological study, where it was stained with hematoxylin and eosin. Following features were noted: the Meckel’s diverticulum was seen at 22 cm proximal to ileocaecal junction; it was 4.3 cm in length with broad tip; it was 3 cm in diameter; it was attached to the antimesentric border of ileum; its tip had no attachment via fibrous band to umbilicus (Figure 1).
Histology
The mucus membrane showed villi. The villi were lined by simple columnar epithelium with goblet cells. The lamina propria showed glands along with isolated lymphatic nodule. Submucosa was present. Muscle layer consisted of inner circular and outer longitudinal layer and outermost serosa (Figure 2).
Discussion
Developmentally the vitelline duct connects the yolk sac and midgut of the embryo at an early stage in fetal life for nutrition [5]. Thus, in the 3 week old embryo the yolk forms the ventral aspect of the gut and communicates through a wide, short vitelline duct, which subsequently becomes absorbed. The blood supply to the vitelline duct comes from paired ventral branches of the abdominal aorta, the vitelline arteries.
If this duct does not involute by 7th week of gestation, various developmental remnants may be left. Failure of most proximal portion of duct to obliterate results in a Meckel’s diverticulum [8]. The yolk sac is continuous with the embryo and contains all layers of the intestinal wall [8].
Meckel’s diverticulum may remain completely asymptomatic, or it may mimic disorders such as Crohn’s disease, appendicitis and peptic ulcer disease. Ectopic tissue found in approximately 50% of cases consists of gastric tissue in 60-65% of cases and pancreatic tissue in 5-16% [9].
Meckel’s diverticulum occurs more commonly in individuals born with other congenital malformations especially exomphalos, esophageal atresia, anorectal atresia and gross malformations of the cardiovascular and central nervous system [9]. Hemingway and Allisan reported an association between angiodysplasia of the caecum and ascending colon with Meckel’s diverticulum in five patients aged between 13 and 21 years [10].
Knowledge of Meckel’s diverticulum is important for surgeons to avoid complications during various abdominal surgeries. It is also important for radiologists while doing ultrasound examination and evaluating radiographs.
References
- Standring S, ed. Gray’s Anatomy. The anatomical basis of clinical practice. 39th Ed., London, Elsevier Churchill Livingstone. 2005; 1167.
- Lüdtke FE, Mende V, Köhler H, Lepsien G. Incidence and frequency of complications and management of Meckels diverticulum. Surg Gynecol Obstet. 1989; 169: 537–542.
- DiGiacomo JC, Cottone FJ. Surgical treatment of Meckel’s diverticulum. South Med J. 1993; 86: 671–675.
- Arnold JF, Pellicane JV. Meckel’s diverticulum: a ten year experience. Am Surg. 1997; 63: 354–355.
- Mackey WC, Dineen P. A fifty year experience with Meckel’s diverticulum. Surg Gynecol Obstet. 1983; 156: 56–64.
- Cullen JJ, Kelly KA, Moir CR, Hodge DO, Zinsmeister AR, Melton LJ 3rd. Surgical management of Meckel’s diverticulum. An epidemiologic, population-based study. Ann Surg. 1994; 220; 564–569.
- Williams RS. Management of Meckel’s diverticulum. Br J Surg. 1981; 68: 477–480.
- Moore KL, Persaud TVN. The Developing Human. 5th Ed., Philadelphia, Saunders. 1993; 255–257.
- Elsayes KM, Menias CO, Harvin HJ, Francis IR. Imaging manifestations of Meckel’s diverticulum. AJR Am J Roentgenol. 2007; 189: 81–88.
- Simms MH, Corkery IJ. Meckel’s diverticulum; a clinical and histological study. Acta Chir Scand. 1959; 248 (Suppl 10): 1.