Medial plantar artery arising from popliteal artery
Lennox S.B. Francis*
Department of Anatomy, Basic Medical Sciences, University of the West Indies Medical School, Mona, Kingston 7, Jamaica, West Indies
- *Corresponding Author:
- Lennox S.B. Francis, MBBS, FRCS(Ed), FACS
Department of Anatomy Basic Medical Sciences University of the West Indies Medical School, Mona, Kingston 7 Jamaica, West Indies
Tel: +1 (876) 830-4838
E-mail: landkfrancis@gmail.com
Date of Received: December 20th, 2015
Date of Accepted: December 30th, 2016
Published Online: February 3rd, 2017
© Int J Anat Var (IJAV). 2016; 9: 79–81.
[ft_below_content] =>Keywords
variant, medial plantar artery, clinical importance
Introduction
Variations of the branching patterns of arteries have always received considerable attention in anatomical literature and these are more common in the upper extremity compared to the lower extremity [1,2]. When it does occur in the lower limb, branching of the popliteal artery is a common site. Variations of the branching patterns of the popliteal artery [3-5] have clinical implications for many procedures, such as bypass grafting for atherosclerotic occlusion; also to the emergency surgeon dealing with vascular injuries and the orthopedic surgeon performing knee replacements and other procedures.
Another clinical implication of this variation pertains to reconstructive surgery. Over the past thirty years a medial plantar artery based skin flap is being used increasingly to provide cover for skin defects of the sole of the foot [6-10].
Case Report
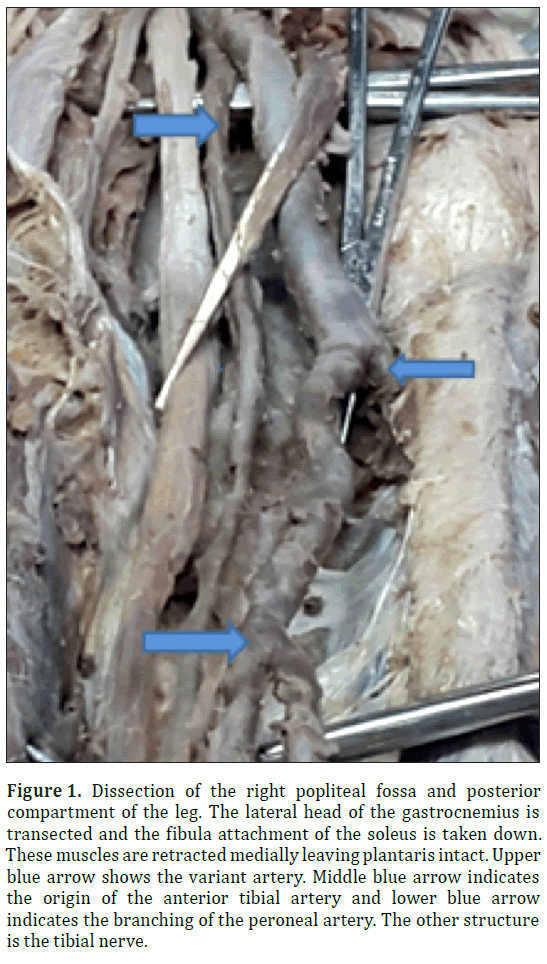
The University of the West Indies Medical School started in 1948 and in our Anatomy Department the teaching of anatomy is based on cadaveric dissection. During routine dissection of the cadaver on an elderly male I noted a variant artery arising from the medial side of the right popliteal artery (Figure 1) and entering the deep compartment with the popliteal artery by passing under the arch of the soleus muscle. After noting this variant, the left popliteal fossa and leg was also dissected (Figure 2) and a similar variant artery was found.
Figure 1: Dissection of the right popliteal fossa and posterior compartment of the leg. The lateral head of the gastrocnemius is transected and the fibula attachment of the soleus is taken down. These muscles are retracted medially leaving plantaris intact. Upper blue arrow shows the variant artery. Middle blue arrow indicates the origin of the anterior tibial artery and lower blue arrow indicates the branching of the peroneal artery. The other structure is the tibial nerve.
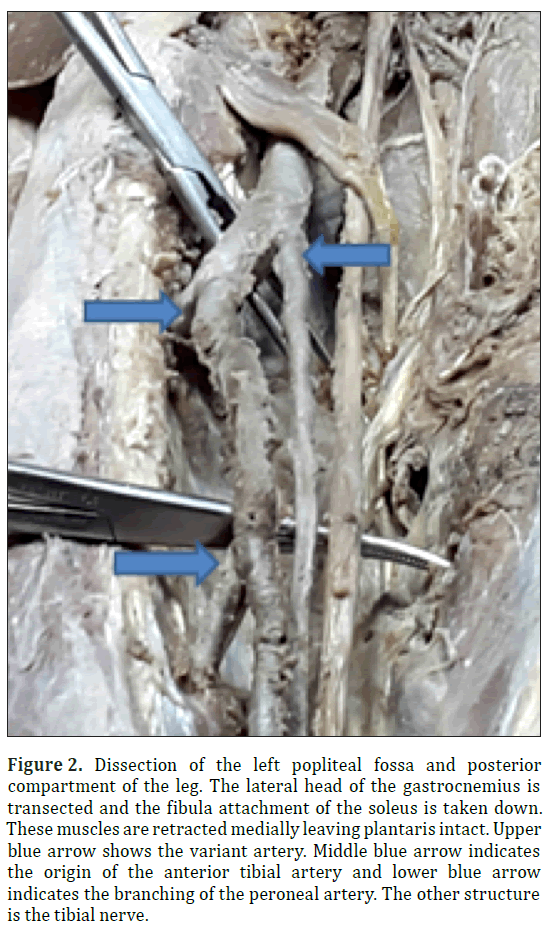
Figure 2: Dissection of the left popliteal fossa and posterior compartment of the leg. The lateral head of the gastrocnemius is transected and the fibula attachment of the soleus is taken down. These muscles are retracted medially leaving plantaris intact. Upper blue arrow shows the variant artery. Middle blue arrow indicates the origin of the anterior tibial artery and lower blue arrow indicates the branching of the peroneal artery. The other structure is the tibial nerve.
The deep posterior compartment of the leg was exposed by transecting the lateral head of the gastrocnemius muscle and taking down the fibula attachment of the soleus. These muscles were retracted medially leaving the plantaris muscle intact. The structures of the deep compartment were further exposed by dividing the transverse intermuscular septum longitudinally and dissecting it off the structures (Figures 1 and 2). The popliteal artery gave off the anterior tibial (AT) artery at the lower border of the popliteus muscle. The tibioperoneal trunk of the posterior tibial (PT) artery was long (7.9 cm on right and 8 cm on left) before giving off the peroneal artery (PA) which ran in a tunnel between the tibialis posterior (TP) muscle and the flexor hallucis longus (FHL). The variant artery ran medial and parallel to the posterior tibial artery, between the tibialis posterior (TP) muscle and the flexor digitorum longus (FDL) muscle throughout the leg.
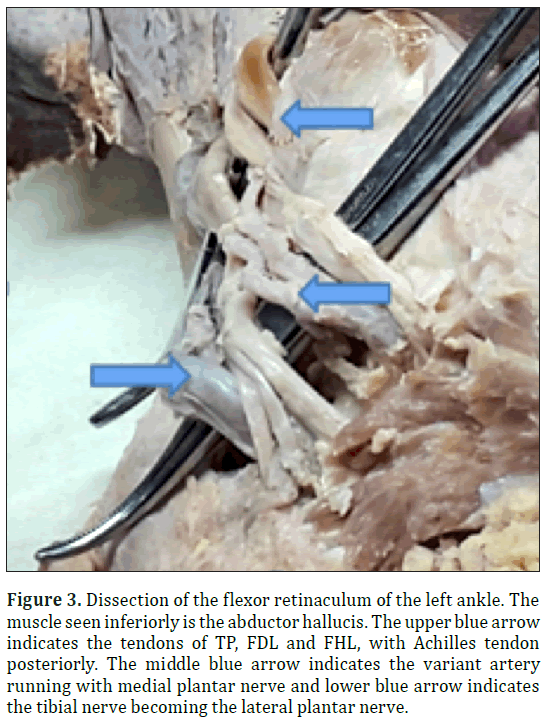
At the flexor retinaculum the variant artery ran in the neurovascular compartment of the flexor retinaculum between the tendons of FDL and FHL. Below the flexor retinaculum (Figure 3) the variant artery accompanied the medial plantar nerve and the posterior tibial artery accompanied the lateral plantar nerve passing laterally and under cover of the abductor hallucis muscle to enter the foot running between the first and second layers of the sole of the foot.
Figure 3: Dissection of the flexor retinaculum of the left ankle. The muscle seen inferiorly is the abductor hallucis. The upper blue arrow indicates the tendons of TP, FDL and FHL, with Achilles tendon posteriorly. The middle blue arrow indicates the variant artery running with medial plantar nerve and lower blue arrow indicates the tibial nerve becoming the lateral plantar nerve.
Dissection of the left leg revealed a similar variant artery. The only difference was that the variant artery arose lower on the medial aspect of the popliteal artery. The variant arteries were 5 mm in diameter.
Discussion
Variations of the branching patterns of arteries, although engendering much interest by anatomists, generally are asymptomatic. They are however very important when procedures are being performed as failure to recognize the aberrant artery may lead to harm for the patient.
Variations of the popliteal artery should be kept in mind when performing procedures such as vascular by-pass grafting for atherosclerotic occlusions, surgical exploration of popliteal artery injuries and orthopaedic procedures on the knee.
A review of the branching patterns of the popliteal artery include: a database review using four studies of anatomical dissections and eleven radiological retrospective series comprising 7671 limbs [3], an angiographic study of 1037 femoral angiograms[4], anatomical studies of lower limbs of 100 cadavers [5]. These studies revealed that on average 90% of branching of the popliteal arteries were normal with anterior tibial (AT) artery branching at inferior border of popliteus, a short tibioperoneal trunk of the posterior tibial (PT) artery before giving off the peroneal artery (PA) artery. Of the 10% with variations, the three common ones were: high origin of AT; trifurcation into AT, PT and PA; and hypoplastic or aplastic PT. There was no mention of another artery branching from the popliteal artery and running down into the leg.
An aberrant medial plantar artery would be of interest to reconstructive surgeons. The use of split skin graft and insensate skin flaps to the weight bearing sole on the heel and ball of the feet over the metatarsal heads gave poor results with skin breakdown and problems with gait [6]. This changed in 1979 when Shanahan and Gingrass [7] introduced the medial plantar artery based sensate skin flap using the skin of the instep to cover skin defects on the heel. This has become the standard for covering heel defects [8]. Using this flap to cover distal skin defects at the ball of the foot was initially challenging but two modifications, a propeller flap based on medial plantar artery perforators [9] and a flap utilizing reverse flow in the medial plantar artery [10] now make this possible.
References
- Lippert H, Pabst R. Arterial variations in man: Classification and frequency. Munich, JF Bergman Verlag. 1985;60-64.
- Adachi B. Das Arteriensystem der Japaner, band 2. Kyoto, Kenkyusha. 1928;198-201.
- Kropman RH, Kiela G, Moll FL, deVries JP. Variations in the anatomy of the popliteal artery and its side branches. Vas Endovascular Surg. 2011;45(6):536-540.
- Day CP, Orme R. Popliteal artery branching patterns -- an angiographic study. Clin Radiol. 2006;61(8):696-699.
- Lappas D, Stavropoulos NA, Noussios G, Sakellariou V, Skandalakis P. Anatomic study of infra-popliteal vessels. Folia Morphol (Warsz). 2012;71(3):164-167.
- Sommerlad BC, McGrouther DA. Resurfacing the sole: Long term follow-up and comparison of techniques. Br J Plast Surg. 1978;31(2):107-116.
- Shanahan RE, Gingrass RP. Medial plantar sensory flap for coverage of heel defects. Plast Reconstr Surg. 1979;64(3):295-298.
- Yang D, Yang JF, Morris SF, Tang M, Nie C. Medial plantar artery perforator flap for soft-tissue reconstruction of the heel. Ann Plast Surg. 2011;67(3):294-298.
- Coriddi M, Carraher AM, Agnese D, Chandawarkar RY. A new propeller flap based upon medial-plantar-artery perforator for reconstruction of the distal weight-bearing foot. JPRAS Open. 2015;4:12-15.
- Schwarz R. Reverse medial plantar artery flap. Lepr Rev. 2006;77(1):69-75.
Lennox S.B. Francis*
Department of Anatomy, Basic Medical Sciences, University of the West Indies Medical School, Mona, Kingston 7, Jamaica, West Indies
- *Corresponding Author:
- Lennox S.B. Francis, MBBS, FRCS(Ed), FACS
Department of Anatomy Basic Medical Sciences University of the West Indies Medical School, Mona, Kingston 7 Jamaica, West Indies
Tel: +1 (876) 830-4838
E-mail: landkfrancis@gmail.com
Date of Received: December 20th, 2015
Date of Accepted: December 30th, 2016
Published Online: February 3rd, 2017
© Int J Anat Var (IJAV). 2016; 9: 79–81.
Abstract
I report a unique case with bilateral aberrant medial plantar arteries observed during cadaveric dissection. A thorough search of the literature did not come up with any other reported cases. The variant arteries arose from the popliteal arteries bilaterally, ran in the deep posterior compartment of the leg, parallel and medial to the posterior tibial artery and maintaining this position entered the neurovascular compartment under the flexor retinaculum. Below the flexor retinaculum the tibial nerve split into the medial and lateral plantar nerves, with the aberrant artery accompanying the medial plantar nerve and the posterior tibial artery becoming the lateral plantar artery. The arteries were marginal to the nerves as they passed laterally and under cover of the abductor hallucis muscle to enter the foot, running between the first and second layers of the muscles of the sole. I will be looking at the clinical importance of this variation.
-Keywords
variant, medial plantar artery, clinical importance
Introduction
Variations of the branching patterns of arteries have always received considerable attention in anatomical literature and these are more common in the upper extremity compared to the lower extremity [1,2]. When it does occur in the lower limb, branching of the popliteal artery is a common site. Variations of the branching patterns of the popliteal artery [3-5] have clinical implications for many procedures, such as bypass grafting for atherosclerotic occlusion; also to the emergency surgeon dealing with vascular injuries and the orthopedic surgeon performing knee replacements and other procedures.
Another clinical implication of this variation pertains to reconstructive surgery. Over the past thirty years a medial plantar artery based skin flap is being used increasingly to provide cover for skin defects of the sole of the foot [6-10].
Case Report
The University of the West Indies Medical School started in 1948 and in our Anatomy Department the teaching of anatomy is based on cadaveric dissection. During routine dissection of the cadaver on an elderly male I noted a variant artery arising from the medial side of the right popliteal artery (Figure 1) and entering the deep compartment with the popliteal artery by passing under the arch of the soleus muscle. After noting this variant, the left popliteal fossa and leg was also dissected (Figure 2) and a similar variant artery was found.
Figure 1: Dissection of the right popliteal fossa and posterior compartment of the leg. The lateral head of the gastrocnemius is transected and the fibula attachment of the soleus is taken down. These muscles are retracted medially leaving plantaris intact. Upper blue arrow shows the variant artery. Middle blue arrow indicates the origin of the anterior tibial artery and lower blue arrow indicates the branching of the peroneal artery. The other structure is the tibial nerve.
Figure 2: Dissection of the left popliteal fossa and posterior compartment of the leg. The lateral head of the gastrocnemius is transected and the fibula attachment of the soleus is taken down. These muscles are retracted medially leaving plantaris intact. Upper blue arrow shows the variant artery. Middle blue arrow indicates the origin of the anterior tibial artery and lower blue arrow indicates the branching of the peroneal artery. The other structure is the tibial nerve.
The deep posterior compartment of the leg was exposed by transecting the lateral head of the gastrocnemius muscle and taking down the fibula attachment of the soleus. These muscles were retracted medially leaving the plantaris muscle intact. The structures of the deep compartment were further exposed by dividing the transverse intermuscular septum longitudinally and dissecting it off the structures (Figures 1 and 2). The popliteal artery gave off the anterior tibial (AT) artery at the lower border of the popliteus muscle. The tibioperoneal trunk of the posterior tibial (PT) artery was long (7.9 cm on right and 8 cm on left) before giving off the peroneal artery (PA) which ran in a tunnel between the tibialis posterior (TP) muscle and the flexor hallucis longus (FHL). The variant artery ran medial and parallel to the posterior tibial artery, between the tibialis posterior (TP) muscle and the flexor digitorum longus (FDL) muscle throughout the leg.
At the flexor retinaculum the variant artery ran in the neurovascular compartment of the flexor retinaculum between the tendons of FDL and FHL. Below the flexor retinaculum (Figure 3) the variant artery accompanied the medial plantar nerve and the posterior tibial artery accompanied the lateral plantar nerve passing laterally and under cover of the abductor hallucis muscle to enter the foot running between the first and second layers of the sole of the foot.
Figure 3: Dissection of the flexor retinaculum of the left ankle. The muscle seen inferiorly is the abductor hallucis. The upper blue arrow indicates the tendons of TP, FDL and FHL, with Achilles tendon posteriorly. The middle blue arrow indicates the variant artery running with medial plantar nerve and lower blue arrow indicates the tibial nerve becoming the lateral plantar nerve.
Dissection of the left leg revealed a similar variant artery. The only difference was that the variant artery arose lower on the medial aspect of the popliteal artery. The variant arteries were 5 mm in diameter.
Discussion
Variations of the branching patterns of arteries, although engendering much interest by anatomists, generally are asymptomatic. They are however very important when procedures are being performed as failure to recognize the aberrant artery may lead to harm for the patient.
Variations of the popliteal artery should be kept in mind when performing procedures such as vascular by-pass grafting for atherosclerotic occlusions, surgical exploration of popliteal artery injuries and orthopaedic procedures on the knee.
A review of the branching patterns of the popliteal artery include: a database review using four studies of anatomical dissections and eleven radiological retrospective series comprising 7671 limbs [3], an angiographic study of 1037 femoral angiograms[4], anatomical studies of lower limbs of 100 cadavers [5]. These studies revealed that on average 90% of branching of the popliteal arteries were normal with anterior tibial (AT) artery branching at inferior border of popliteus, a short tibioperoneal trunk of the posterior tibial (PT) artery before giving off the peroneal artery (PA) artery. Of the 10% with variations, the three common ones were: high origin of AT; trifurcation into AT, PT and PA; and hypoplastic or aplastic PT. There was no mention of another artery branching from the popliteal artery and running down into the leg.
An aberrant medial plantar artery would be of interest to reconstructive surgeons. The use of split skin graft and insensate skin flaps to the weight bearing sole on the heel and ball of the feet over the metatarsal heads gave poor results with skin breakdown and problems with gait [6]. This changed in 1979 when Shanahan and Gingrass [7] introduced the medial plantar artery based sensate skin flap using the skin of the instep to cover skin defects on the heel. This has become the standard for covering heel defects [8]. Using this flap to cover distal skin defects at the ball of the foot was initially challenging but two modifications, a propeller flap based on medial plantar artery perforators [9] and a flap utilizing reverse flow in the medial plantar artery [10] now make this possible.
References
- Lippert H, Pabst R. Arterial variations in man: Classification and frequency. Munich, JF Bergman Verlag. 1985;60-64.
- Adachi B. Das Arteriensystem der Japaner, band 2. Kyoto, Kenkyusha. 1928;198-201.
- Kropman RH, Kiela G, Moll FL, deVries JP. Variations in the anatomy of the popliteal artery and its side branches. Vas Endovascular Surg. 2011;45(6):536-540.
- Day CP, Orme R. Popliteal artery branching patterns -- an angiographic study. Clin Radiol. 2006;61(8):696-699.
- Lappas D, Stavropoulos NA, Noussios G, Sakellariou V, Skandalakis P. Anatomic study of infra-popliteal vessels. Folia Morphol (Warsz). 2012;71(3):164-167.
- Sommerlad BC, McGrouther DA. Resurfacing the sole: Long term follow-up and comparison of techniques. Br J Plast Surg. 1978;31(2):107-116.
- Shanahan RE, Gingrass RP. Medial plantar sensory flap for coverage of heel defects. Plast Reconstr Surg. 1979;64(3):295-298.
- Yang D, Yang JF, Morris SF, Tang M, Nie C. Medial plantar artery perforator flap for soft-tissue reconstruction of the heel. Ann Plast Surg. 2011;67(3):294-298.
- Coriddi M, Carraher AM, Agnese D, Chandawarkar RY. A new propeller flap based upon medial-plantar-artery perforator for reconstruction of the distal weight-bearing foot. JPRAS Open. 2015;4:12-15.
- Schwarz R. Reverse medial plantar artery flap. Lepr Rev. 2006;77(1):69-75.