Median nerve compression and the reversed palmaris longus
Janet M. Cope1*, Erin M. Looney2, Christine A. Craig2, Rebecca Gawron2, Rachel Lampros2 and Ryan Mahoney2
1Department of Physical Therapy, Elon University, Elon, North Carolina, USA
2Department of Physical Therapy & Exercise Science, Springfield College, Springfield, Massachusetts, USA
- *Corresponding Author:
- Dr. Janet M. Cope, PhD, OTR/L
Department of Physical Therapy, Campus Box 2085, Elon University, Elon, North Carolina, 27244, USA
Tel: +1 (336) 278-6355
E-mail: jcope2@elon.edu
Date of Received: May 6th, 2009
Date of Accepted: August 26th, 2009
Published Online: September 7th, 2009
© IJAV. 2009; 2: 102–104.
[ft_below_content] =>Keywords
forearm musculature variation, median nerve compression
Introduction
Although palmaris longus is considered an ancillary forearm muscle its tendon is frequently harvested and used in the surgical repair of other structures. It can be used to repair a ruptured ulnar collateral ligament or replace an osteoarthritic trapezium bone. Additionally, it has been used as a substitute for absent flexor tendons, atrophied intrinsic hand musculature and absent facial musculature in reconstructive procedures [1–3].
Typically, the PL muscle is comprised of three sections: a proximal short muscular attachment to the medial epicondyle, a musculotendinous juncture at the level of the distal segment of pronator teres, and a distal slender, tendinous insertion into the palmar aponeurosis. In a 1944 large scale study of 1600 cadaveric limbs, Reimann and colleagues found that 12.8% were missing PL and an additional 9% had variations in the location and form of the muscle belly, including (proximal, distal, central, digastrics and bifid) distal attachment sites [4]. There are many documented variations in the distal tendinous slips of the PL, including insertions that travel through the carpal tunnel or attachments to the thenar fascia or musculature [4–7].
Carpal tunnel syndrome (CTS) is one of the most common nerve entrapment disorders and is often associated with variations in the anatomy at the wrist [8,9]. Variations of PL with reported distal attachments within and anterior to the carpal tunnel can increase the amount of pressure placed on the median nerve, potentially leading to CTS [6,8,9].
An increasing number of surgeons are reporting patient cases where a reversed PL variation is the cause of median nerve compression in patients performing repetitive work tasks [10–15]. Patients who have a PL variation with median nerve compression and effort-related pain often exhibit false-negatives on classic tests for neuropathy such as the Tinel sign, Phalens test [10,13,16] and electromyographic studies [14,15].
In 2000, Schuurman and van Gils [14] identified four patients, at the University Hospital of Utrecht in the Netherlands, who had a reversed PL muscle, causing activity-related compression of the median nerve. Magnetic resonance imaging (MRI) studies performed on these patients were recorded as negative for CTS by radiologists. Further review of the MRIs by surgeons showed the reversed PL as the source of median nerve compression, instead of an inflamed carpal tunnel as expected. The reversed variation of PL musculature should be considered in the assessment of median nerve neuropathy.
Yildiz and colleagues [15] from Turkey and Natsis and colleagues [17] from Greece each reported on subjects with a rare reversed PL muscle found to have three insertions, as compared with one. Bozkurt and colleagues [18] reported a donor with both an anomalous PL and abductor digiti minimi muscles that had attachments travelling through Guyon’s canal. Reversed PL muscular variations should also be considered with ulnar neuropathy at the wrist.
Case Report
The subject was an eighty year-old, right-handed, female who had worked as a machine operator for 45 years. A pre-mortem self-reported medical history was reviewed and the donor’s daughter was interviewed regarding her mother’s past health, social and occupational history by the primary investigator.
During a routine dissection of this donor’s forearms in the human anatomy laboratory at Springfield College, Springfield, Massachusetts; it was noted that the right PL muscle was variant. The right PL was dissected away from the surrounding structures, exposing its origin at the medial epicondyle of the humerus, the musculotendinous juncture and its distal attachments on the volar aspect of the hand. All attachments, both proximally and distally, were identified. The median and ulnar nerves were assessed for signs of compression or attenuation from the proximal wrist and into the hand. Measurements and photographs were taken throughout the course of the dissection to document all relevant structures for location, size and morphology.
The proximal attachment of the PL arising from the medial epicondyle of the humerus was tendinous and had some fibers that were contiguous with both the pronator teres and flexor digitorum superficialis. Distally the PL was muscular with fibrous connections to the flexor carpi radialis muscle.
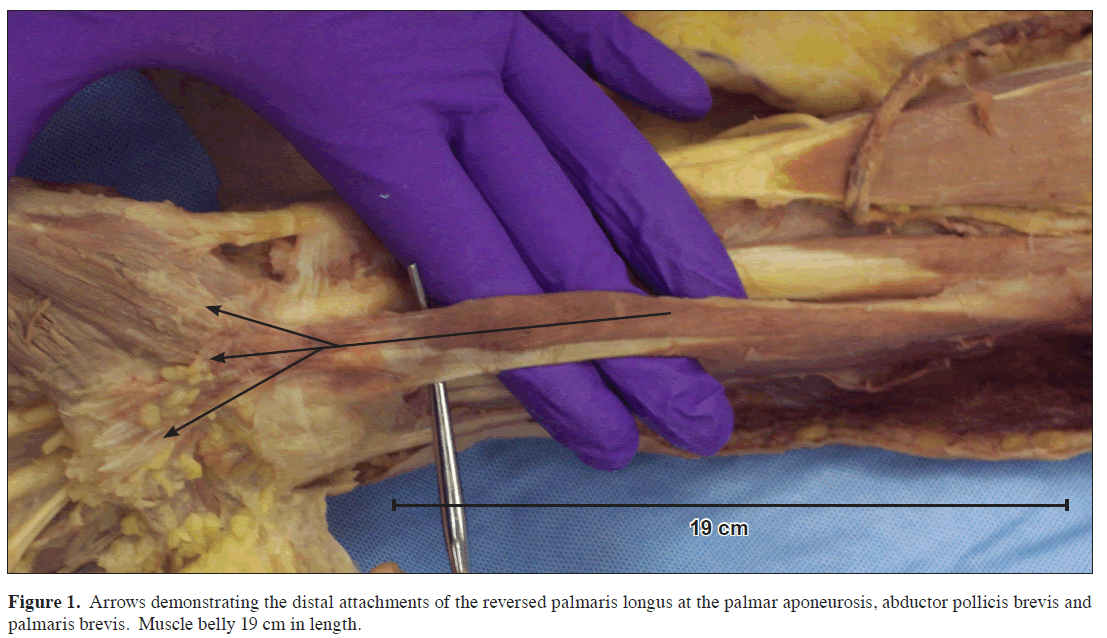
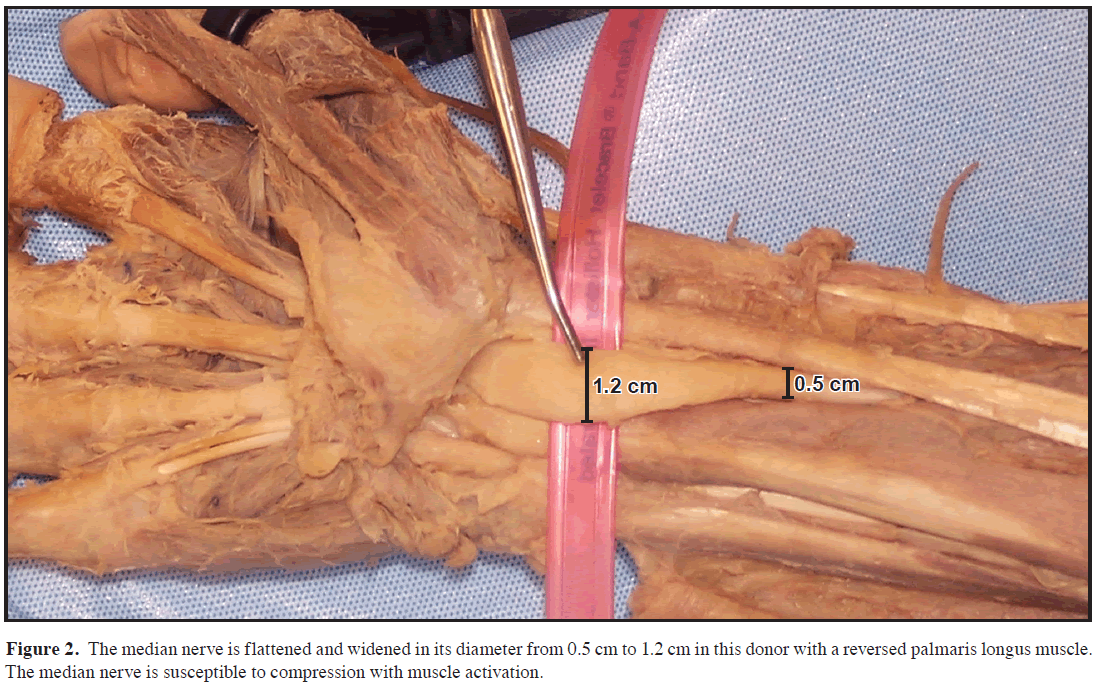
The proximal tendon of PL was 9 cm in length. The distal muscle belly was 19 cm long and traversed the entire length of the forearm to the proximal wrist crease. Here the PL passed superficial to the flexor retinaculum and then attached broadly to the palmar aponeurosis, abductor pollicis brevis and palmaris brevis (Figure 1). Just proximal to the wrist the median nerve was enlarged and flattened as it passed between the muscular segment of PL and the tendons of flexor digitorum superficialis (Figure 2). The donor had a lunar shaped scar at the right palm, consistent with a carpal tunnel release. The ulnar nerve was explored with no abnormalities in course or appearance observed. However, the potential for both median and ulnar nerve compression by this atypical reversed PL musculature warrants further consideration.
Discussion
Although carpal tunnel surgery was not documented in the donor’s self-reported medical history or recalled by the daughter during the interview, there was a lunar shaped palmar scar at the right hand consistent with a carpal tunnel release. The scar was well healed, flat and faded. The median nerve was flattened and more than doubled in medial to lateral dimensions (a change from 0.5 cm to 1.2 cm) just proximal to the flexor retinaculum.
The variation in PL in this donor may have contributed to the compression of the median nerve. The subject worked as a machine operator for 45 years, performing repetitive bimanual tasks, potentially causing hypertrophy of the distal muscle belly of the right PL. At rest the subject may not have been symptomatic. However, following repetitive contractions, the PL may have caused localized pressure on the median nerve compressing and widening it as was observed on this donor.
As the PL can be highly variable, it is important for physicians, radiologists and therapists to be aware of the possibility of variations, especially one that might contribute to median or ulnar nerve compression at the wrist. Patients who complain of wrist pain with a palpable mass at the volar wrist should be examined thoroughly for variations of their PL musculature. Patients who report wrist pain but have negative Tinel and Phalens tests might also be asked to perform a repetitive grasp and release activity to assess for activity induced median nerve symptomatology. Nerve conduction studies are typically conducted on patients at rest. Although nerve conduction studies are appropriate procedures, testing performed with the patient at rest may produce a false negative for patients that are only symptomatic with activity. Ultrasound or MRI studies can be used to assess for PL variations in patients who are to undergo tendon transfer procedures, carpal tunnel or Guyon’s canal releases, or who have had previous failed nerve releases. All who are involved in patient care should be aware of the impact that this particular reversed PL muscle variation can have on the median and ulnar nerves at the wrist.
References
- Hunter J, Mackin E, Callahan A. Rehabilitation of the Hand: Surgery and Therapy. 4 th Ed., St. Louis, Mosby. 1995; 48–49, 497.
- Brand PW, Hollister A. Clinical Mechanics of the Hand. St. Louis, Mosby-Year Book. 1999; 119.
- Chauhan R. Atypical innervation of palmaris longus: A case report. J Anat Soc India. 2003; 52: 171–173.
- Reimann AP, Daseler EH, Anson BJ, Beaton LE. The palmaris longus muscle and tendon: a study of 1600 extremities. Anat Rec. 1944; 89: 495–505.
- Koo CC, Roberts AH. The palmaris longus tendon: Another variation in its anatomy. J Hand Surg Br. 1997; 22: 138–139.
- Mobbs RJ, Chandran KN. Variation of palmaris longus tendon. Aust N Z J Surg. 2000; 70: 538.
- Oommen A, Rajarajeshwari. Palmaris longus: Upside down!!! J Anat Soc India. 2002; 51 (2): 232–233.
- De Smet L. Median and ulnar nerve compression at the wrist caused by anomalous muscles. Acta Orthop Belg. 2002; 68: 431–438.
- Jones DP. Bilateral Palmaris profundus in association with bifid median nerve as a cause of failed carpal tunnel release. J Hand Surg Am. 2006; 31: 741–743.
- Depuydt KH, Schuurman AH, Kon M. Reversed palmaris longus muscle causing effort-related median nerve compression. J Hand Surg Br. 1998; 23: 117–119.
- Guler MM, Celikoz B. Anomalous Palmaris longus muscle causing carpal tunnel-like syndrome. Arch Orthop Trauma Surg. 1998; 117: 296–297.
- Polesuk BS, Helms CA. Hypertrophied palmaris longus muscle, a pseudomass of the forearm: MR appearance--case report and review of the literature. Radiology. 1998; 207: 361–362.
- Bencteux P, Simonet J, el Ayoubi L, Renard M, Attignon I, Dacher JN, Thiebot J. Symptomatic palmaris longus muscle variation with MRI and surgical correlation: report of a single case. Surg Radiol Anat. 2001; 23: 273–275.
- Schuurman AH, van Gils AP. Reversed palmaris longus muscle on MRI: report of four cases. Eur Radiol. 2000; 10: 1242–1244.
- Yildiz M, Sener M, Aynaci O. Three-headed reversed palmaris longus muscle: a case report and review of the literature. Surg Radiol Anat. 2000; 22: 217–219.
- Rubino C, Paolini G, Carlesimo B. Accessory slip of the palmaris longus muscle. Ann Plast Surg. 1995; 35: 657–659.
- Natsis K, Levva S, Totlis T, Anastasopoulos N, Paraskevas G. Three-headed reversed palmaris longus muscle and its clinical significance. Ann Anat. 2007; 189: 97–101.
- Bozkurt MC, Tagil SM, Ersoy M, Tekdemir I. Muscle variations and abnormal branching and course of the ulnar nerve in the forearm and hand. Clin Anat. 2004; 17: 64–66.
Janet M. Cope1*, Erin M. Looney2, Christine A. Craig2, Rebecca Gawron2, Rachel Lampros2 and Ryan Mahoney2
1Department of Physical Therapy, Elon University, Elon, North Carolina, USA
2Department of Physical Therapy & Exercise Science, Springfield College, Springfield, Massachusetts, USA
- *Corresponding Author:
- Dr. Janet M. Cope, PhD, OTR/L
Department of Physical Therapy, Campus Box 2085, Elon University, Elon, North Carolina, 27244, USA
Tel: +1 (336) 278-6355
E-mail: jcope2@elon.edu
Date of Received: May 6th, 2009
Date of Accepted: August 26th, 2009
Published Online: September 7th, 2009
© IJAV. 2009; 2: 102–104.
Abstract
The palmaris longus (PL) muscle is an ancillary wrist flexor that is absent in one or both forearms in ten to fourteen percent of the world’s population. Numerous variations of the PL have been documented throughout the literature. In this case study, a variation of PL was identified during the dissection of an eighty year-old female human donor, who had worked as a machine operator for 45 years. The right PL originated at the medial epicondyle however, the attachment was tendinous rather than muscular in nature. The musculotendinous juncture occurred approximately mid-forearm and distally it inserted into the palmar aponeurosis, abductor pollicis brevis and palmaris brevis via a broad, muscular attachment. Additionally this donor had a flattened and enlarged median nerve at the volar wrist. This particular variation of the PL is rarely reported and has the potential to cause compression of both the median and ulnar nerves.
-Keywords
forearm musculature variation, median nerve compression
Introduction
Although palmaris longus is considered an ancillary forearm muscle its tendon is frequently harvested and used in the surgical repair of other structures. It can be used to repair a ruptured ulnar collateral ligament or replace an osteoarthritic trapezium bone. Additionally, it has been used as a substitute for absent flexor tendons, atrophied intrinsic hand musculature and absent facial musculature in reconstructive procedures [1–3].
Typically, the PL muscle is comprised of three sections: a proximal short muscular attachment to the medial epicondyle, a musculotendinous juncture at the level of the distal segment of pronator teres, and a distal slender, tendinous insertion into the palmar aponeurosis. In a 1944 large scale study of 1600 cadaveric limbs, Reimann and colleagues found that 12.8% were missing PL and an additional 9% had variations in the location and form of the muscle belly, including (proximal, distal, central, digastrics and bifid) distal attachment sites [4]. There are many documented variations in the distal tendinous slips of the PL, including insertions that travel through the carpal tunnel or attachments to the thenar fascia or musculature [4–7].
Carpal tunnel syndrome (CTS) is one of the most common nerve entrapment disorders and is often associated with variations in the anatomy at the wrist [8,9]. Variations of PL with reported distal attachments within and anterior to the carpal tunnel can increase the amount of pressure placed on the median nerve, potentially leading to CTS [6,8,9].
An increasing number of surgeons are reporting patient cases where a reversed PL variation is the cause of median nerve compression in patients performing repetitive work tasks [10–15]. Patients who have a PL variation with median nerve compression and effort-related pain often exhibit false-negatives on classic tests for neuropathy such as the Tinel sign, Phalens test [10,13,16] and electromyographic studies [14,15].
In 2000, Schuurman and van Gils [14] identified four patients, at the University Hospital of Utrecht in the Netherlands, who had a reversed PL muscle, causing activity-related compression of the median nerve. Magnetic resonance imaging (MRI) studies performed on these patients were recorded as negative for CTS by radiologists. Further review of the MRIs by surgeons showed the reversed PL as the source of median nerve compression, instead of an inflamed carpal tunnel as expected. The reversed variation of PL musculature should be considered in the assessment of median nerve neuropathy.
Yildiz and colleagues [15] from Turkey and Natsis and colleagues [17] from Greece each reported on subjects with a rare reversed PL muscle found to have three insertions, as compared with one. Bozkurt and colleagues [18] reported a donor with both an anomalous PL and abductor digiti minimi muscles that had attachments travelling through Guyon’s canal. Reversed PL muscular variations should also be considered with ulnar neuropathy at the wrist.
Case Report
The subject was an eighty year-old, right-handed, female who had worked as a machine operator for 45 years. A pre-mortem self-reported medical history was reviewed and the donor’s daughter was interviewed regarding her mother’s past health, social and occupational history by the primary investigator.
During a routine dissection of this donor’s forearms in the human anatomy laboratory at Springfield College, Springfield, Massachusetts; it was noted that the right PL muscle was variant. The right PL was dissected away from the surrounding structures, exposing its origin at the medial epicondyle of the humerus, the musculotendinous juncture and its distal attachments on the volar aspect of the hand. All attachments, both proximally and distally, were identified. The median and ulnar nerves were assessed for signs of compression or attenuation from the proximal wrist and into the hand. Measurements and photographs were taken throughout the course of the dissection to document all relevant structures for location, size and morphology.
The proximal attachment of the PL arising from the medial epicondyle of the humerus was tendinous and had some fibers that were contiguous with both the pronator teres and flexor digitorum superficialis. Distally the PL was muscular with fibrous connections to the flexor carpi radialis muscle.
The proximal tendon of PL was 9 cm in length. The distal muscle belly was 19 cm long and traversed the entire length of the forearm to the proximal wrist crease. Here the PL passed superficial to the flexor retinaculum and then attached broadly to the palmar aponeurosis, abductor pollicis brevis and palmaris brevis (Figure 1). Just proximal to the wrist the median nerve was enlarged and flattened as it passed between the muscular segment of PL and the tendons of flexor digitorum superficialis (Figure 2). The donor had a lunar shaped scar at the right palm, consistent with a carpal tunnel release. The ulnar nerve was explored with no abnormalities in course or appearance observed. However, the potential for both median and ulnar nerve compression by this atypical reversed PL musculature warrants further consideration.
Discussion
Although carpal tunnel surgery was not documented in the donor’s self-reported medical history or recalled by the daughter during the interview, there was a lunar shaped palmar scar at the right hand consistent with a carpal tunnel release. The scar was well healed, flat and faded. The median nerve was flattened and more than doubled in medial to lateral dimensions (a change from 0.5 cm to 1.2 cm) just proximal to the flexor retinaculum.
The variation in PL in this donor may have contributed to the compression of the median nerve. The subject worked as a machine operator for 45 years, performing repetitive bimanual tasks, potentially causing hypertrophy of the distal muscle belly of the right PL. At rest the subject may not have been symptomatic. However, following repetitive contractions, the PL may have caused localized pressure on the median nerve compressing and widening it as was observed on this donor.
As the PL can be highly variable, it is important for physicians, radiologists and therapists to be aware of the possibility of variations, especially one that might contribute to median or ulnar nerve compression at the wrist. Patients who complain of wrist pain with a palpable mass at the volar wrist should be examined thoroughly for variations of their PL musculature. Patients who report wrist pain but have negative Tinel and Phalens tests might also be asked to perform a repetitive grasp and release activity to assess for activity induced median nerve symptomatology. Nerve conduction studies are typically conducted on patients at rest. Although nerve conduction studies are appropriate procedures, testing performed with the patient at rest may produce a false negative for patients that are only symptomatic with activity. Ultrasound or MRI studies can be used to assess for PL variations in patients who are to undergo tendon transfer procedures, carpal tunnel or Guyon’s canal releases, or who have had previous failed nerve releases. All who are involved in patient care should be aware of the impact that this particular reversed PL muscle variation can have on the median and ulnar nerves at the wrist.
References
- Hunter J, Mackin E, Callahan A. Rehabilitation of the Hand: Surgery and Therapy. 4 th Ed., St. Louis, Mosby. 1995; 48–49, 497.
- Brand PW, Hollister A. Clinical Mechanics of the Hand. St. Louis, Mosby-Year Book. 1999; 119.
- Chauhan R. Atypical innervation of palmaris longus: A case report. J Anat Soc India. 2003; 52: 171–173.
- Reimann AP, Daseler EH, Anson BJ, Beaton LE. The palmaris longus muscle and tendon: a study of 1600 extremities. Anat Rec. 1944; 89: 495–505.
- Koo CC, Roberts AH. The palmaris longus tendon: Another variation in its anatomy. J Hand Surg Br. 1997; 22: 138–139.
- Mobbs RJ, Chandran KN. Variation of palmaris longus tendon. Aust N Z J Surg. 2000; 70: 538.
- Oommen A, Rajarajeshwari. Palmaris longus: Upside down!!! J Anat Soc India. 2002; 51 (2): 232–233.
- De Smet L. Median and ulnar nerve compression at the wrist caused by anomalous muscles. Acta Orthop Belg. 2002; 68: 431–438.
- Jones DP. Bilateral Palmaris profundus in association with bifid median nerve as a cause of failed carpal tunnel release. J Hand Surg Am. 2006; 31: 741–743.
- Depuydt KH, Schuurman AH, Kon M. Reversed palmaris longus muscle causing effort-related median nerve compression. J Hand Surg Br. 1998; 23: 117–119.
- Guler MM, Celikoz B. Anomalous Palmaris longus muscle causing carpal tunnel-like syndrome. Arch Orthop Trauma Surg. 1998; 117: 296–297.
- Polesuk BS, Helms CA. Hypertrophied palmaris longus muscle, a pseudomass of the forearm: MR appearance--case report and review of the literature. Radiology. 1998; 207: 361–362.
- Bencteux P, Simonet J, el Ayoubi L, Renard M, Attignon I, Dacher JN, Thiebot J. Symptomatic palmaris longus muscle variation with MRI and surgical correlation: report of a single case. Surg Radiol Anat. 2001; 23: 273–275.
- Schuurman AH, van Gils AP. Reversed palmaris longus muscle on MRI: report of four cases. Eur Radiol. 2000; 10: 1242–1244.
- Yildiz M, Sener M, Aynaci O. Three-headed reversed palmaris longus muscle: a case report and review of the literature. Surg Radiol Anat. 2000; 22: 217–219.
- Rubino C, Paolini G, Carlesimo B. Accessory slip of the palmaris longus muscle. Ann Plast Surg. 1995; 35: 657–659.
- Natsis K, Levva S, Totlis T, Anastasopoulos N, Paraskevas G. Three-headed reversed palmaris longus muscle and its clinical significance. Ann Anat. 2007; 189: 97–101.
- Bozkurt MC, Tagil SM, Ersoy M, Tekdemir I. Muscle variations and abnormal branching and course of the ulnar nerve in the forearm and hand. Clin Anat. 2004; 17: 64–66.