Medical staff’s attitude and behavior towards prevention of HIV
Received: 01-Mar-2022, Manuscript No. PULIJHAR-22-4710; Editor assigned: 03-Mar-2022, Pre QC No. PULIJHAR-22-4710 (PQ); Accepted Date: Mar 15, 2022; Reviewed: 09-Mar-2022 QC No. PULIJHAR-22-4710 (Q); Revised: 12-Mar-2022, Manuscript No. PULIJHAR-22-4710 (R); Published: 28-Mar-2022, DOI: DOI:10.37532/ pulijhar.22.5(2).13
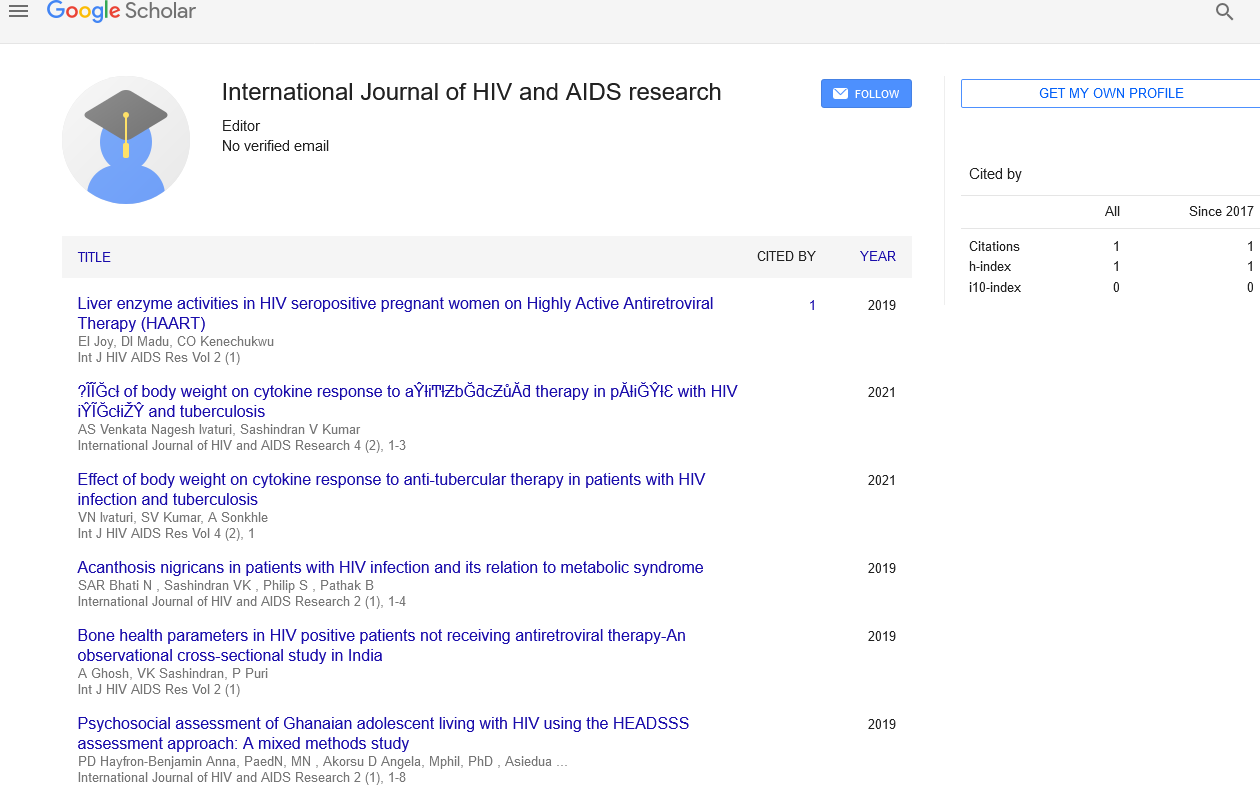
Citation: Anderson M. HIV and alcohol use: Addressing the issues. J HIV AIDS Res. 2022;5(2): 13.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
In Sub-Saharan Africa, the prevalence of the Human Immunodeficiency Virus (HIV) remains high, and there is a tiny but significant risk of surgical workers contracting HIV from infected surgical patients over time. At a tertiary hospital in Malawi, we performed this study to look into the attitudes and behaviors of surgical personnel when it came to preventing Occupational HIV Infection (OHI). This was a cross-sectional qualitative study that used a semistructured questionnaire to investigate the attitudes and practices of surgical staff (surgeons, nurses, and clinical officers) regarding self-protection from OHI. We gathered information on self-protective measures to limit the risk of HIV infection, as well as practices in the event of an accidental HIV infection. In addition, we conducted blind observations of operating room personnel. The data was manually evaluated, with themes drawn and conclusions drawn. Some people thought HIV’s infectiousness from workplace exposure was too low and insignificant. The importance of post-exposure prophylaxis was also overlooked. Due to a lack of resources for personal protection, the majority of employees did not use self-defense materials. There were no formal institutional protocols in place, nor were there any recommendations for staff training on OHI. The views and practice patterns of healthcare professionals in this Malawian institution are often, but not always, in line with scholarly research in the field of OHI prevention. The hospital’s level of information distribution and material support is insufficient.
Key Words
Occupational HIV infection; HIV; Post-exposure prophylaxis
Introduction
At the end of 2019, 38 million persons worldwide were infected with the Human Immunodeficiency Virus (HIV) (World Health Organization, 2020). In Malawi, the national HIV prevalence rate was 10.4 percent in 2016. In contrast to the 11 percent national HIV prevalence (National Statistical Office), a study in 2012 found a statistically significant higher prevalence of HIV infection in patients presenting with surgical problems, at 13 percent. According to the literature, health personnel are at a low but considerable risk of getting HIV from patient bodily fluids when conducting surgical procedures, a condition known as Occupational HIV Infection (OHI).
In order to prevent OHI, the World Health Organization recommends that surgical professionals use extra caution while dealing with all patients. These precautions include taking a detailed medical history and physical examination before performing invasive procedures on surgical patients, wearing double gloves while conducting surgical operations, wearing appropriate surgical garb, including footwear that prevents contact with the patients’ bodily fluids, and using non-touch suturing techniques, in which they do not physically touch sharp objects during operations in or out of the operating room. Unfortunately, due to budget constraints, hospitals in lowincome nations are unable to regularly offer the necessary materials, putting employees at greater risk of OHI.
Human factors such as poor adherence to known proven safe practices, not knowing the HIV status of patients undergoing surgical procedures, lack of familiarity with locally available prevention guidelines, and job relinquishment. A study done with Chinese nurses found a significant rate of injuries, but the victims did not seek Post-Exposure Prophylaxis (PEP) guidance due to a lack of understanding of the PEP programme in the institutions and a reluctance to test for HIV. These issues have not been thoroughly investigated in Africa, to our knowledge. We did this survey to learn more about surgical staff’s views and behaviors when it comes to OHI prevention. This is the first study in Malawi to look into this problem, as far as we know.
Conclusion
The views and practice patterns of healthcare workers in an urban tertiary hospital in Malawi are often, but not always, in agreement with the scientific literature in the field of OHI prevention. The hospital provides them with insufficient information and material help. Positive characteristics were recognition of the significant risk of infection due to Malawi’s high HIV prevalence, readiness to take PEP, and support for an institutional orientation programme on local OHI procedures, among others. Infection can occur as a result of a needle stick injury. Although data show that the probability of HIV transmission through a single percutaneous needle stick or scalpel cut from an HIV infected individual (not on treatment or without viral load suppression) is roughly 0.3 percent, other conditions make the risk much higher. The notion will be institutionalized through training and the provision of personal protective equipment, making the work environment safer for employees.