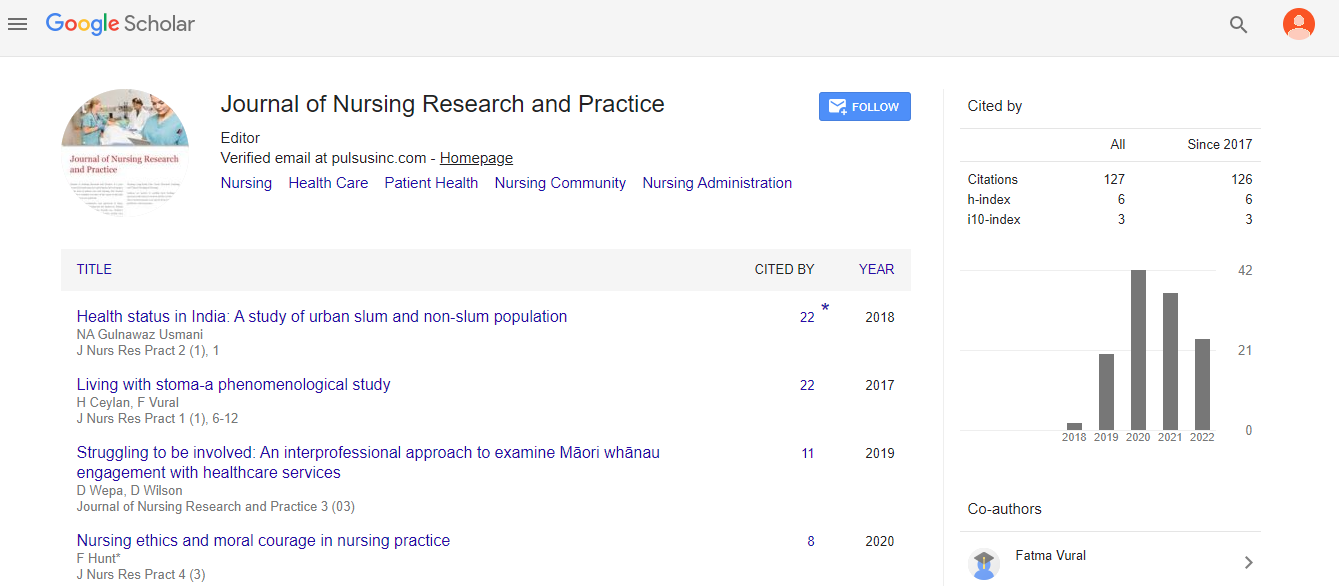
Medication compliance and adherence: a recipe for boosting patient results
Received: 15-Nov-2022, Manuscript No. PULJNRP-22-5627; Editor assigned: 16-Nov-2022, Pre QC No. PULJNRP-22-5627(PQ); Accepted Date: Nov 26, 2022; Reviewed: 20-Nov-2022 QC No. PULJNRP-22-5627(Q); Revised: 25-Nov-2022, Manuscript No. PULJNRP-22-5627(R); Published: 28-Nov-2022, DOI: DOI: 10.37532/ Puljnrp -.22.6(9).155-157
Citation: William D. Medication compliance and adherence: A recipe for boosting patient results. J Nurs Res Pract. 2022; 6(8):155-157
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
In the past, indicators of patient health outcomes included symptom recurrence, emergency department visits, hospitalization and readmission rates, morbidity, and mortality. The promptness of disease diagnosis and management, the expense of therapy, the availability of health insurance, and medication adherence are all factors that providers, who play a large role in the healthcare system, can affect. Beyond the availability and accessibility of healthcare, the capacity of patients to follow doctors' treatment advice greatly contributes to patient outcomes. Unfortunately, there has been a lot of pharmaceutical non-adherence, which has led to poorer health conditions, higher healthcare costs, and higher healthcare spending. This article offers some fresh suggestions and worthwhile factors for promoting drug adherence. Compliance could be improved by raising provider and patient awareness and implementing active and passive communication strategies, including reminders with consent. Adherence might be increased through supporting collaborations between service provider organizations and community and faith-based organizations. It may be possible to promote refills and compliance by adopting an income-based cap on out-of-pocket expenses and modifying the physical characteristics, bioavailability, and dosage schedule of medications to accommodate a variety of patient population preferences. Patient outcomes can be enhanced by maintaining good medication adherence
Key Words:
Patient outcomes, health outcomes; Clinicians' and patients' education; Medication compliance; Non-adherence and communication
INTRODUCTION
The patient's outcome is the ultimate goal, and it comes before the glitz and glamour of medical technological advancements in the 21st century and the mechanics of drug development, informed prescribing, and medicine delivery. Patient’s outcomes include incidents related to illness, disease investigation, and drug use, as well as things like symptom persistence, recurrence, and remission, frequency of ER visits, hospitalization and readmission, timeliness, effectiveness, and safety of care, as well as morbidity and mortality. Cost of therapy, availability of health insurance, timely diagnosis and treatment management, and drug adherence are a few variables that may have an impact on a patient's health results.
Medication compliance and noncompliance:
Medication compliance, also referred to as medication adherence, is the replacement for treatment recommendations. In light of the timing, dosage, and frequency of pharmaceutical use, it might be described as the "act or extent of adhering to a medical recommendation/prescription. It is also known as the ratio of drug doses consumed to doses prescribed during a certain time period. The medication possession ratio, self-report adherence scale, pharmacy refill records and pill counts, micro-electric event monitoring, biological indices drug or metabolite levels in blood or urine, and supervised dosing are all methods for assessing medication compliance. Patients' health results are influenced by how well they take their medications. Therefore, pharmaceutical non-adherence can lead to negative health consequences, such as deteriorating medical conditions, a rise in comorbidities, and even mortality. The increased healthcare needs brought on by drug no adherence frequently result in higher healthcare costs, which inevitably raise overall healthcare spending. Therefore, medication no adherence is a significant problem for world health. Understanding some of the influencing elements, which may be divided into three categories: providers, patients, and pharmaceuticals, is crucial in order to propose answers.
Providers’ factors
Providers, including as doctors, pharmacists, nurse practitioners, and physician assistants, play a part in determining whether or not patients follow prescriptions as one of the stakeholders in patient care. Due to the demands of everyday tasks, healthcare professionals may get too preoccupied with disease dynamics and available treatments to pay attention to patients' acceptance of those treatments, especially when utilizing drugs. As a result, healthcare professionals are unable to effectively inform patients about the preparation, administration, timing, frequency, adverse effects, and cost of the recommended medication.
Patients’ factors
Since patients are the main beneficiaries of healthcare, it is important to take into account their requirements when addressing prescription non-adherence. While admitting that patients are responsible for their own health, it is crucial to keep in mind that certain deviations may be brought on by incomplete knowledge of their diagnosis and available treatments. Medication adherence can be negatively impacted by a number of factors, including illiteracy, polypharmacy taking numerous medications alcohol usage, cultural considerations, religious convictions, and a lack of information regarding the effects of treatment alternatives. Non adherence can also be caused by mental health conditions that people cannot manage, such as depression and cognitive impairment. Patients' socioeconomic status, which is related to whether they are employed or not, determines whether they have access to health insurance and, as a result, whether they can afford their prescription drugs.
Medication or treatment factors
Adherence to drugs can be affected by their properties, such as their pharmaceutical formulation, dosage, amount, frequency of use, and dosage forms such as tablets, capsules, powder, suspension, emulsion, syrup, injection, aerosol, and foam. Potential obstacles to adherence could include cost, time, and side effects. For instance, antiretroviral therapy side effects like headaches, diarrhea, vomiting, and peripheral neuropathy can make people less likely to take what is meant to be a lifelong medication. Poor health outcomes, an increase in viral load, a decrease in CD4 counts, and non-compliance with ARTs are possible outcomes.
Providers’ education
The ability of patients to follow through with recommended therapy or medications might be influenced by the providers' education. Providers must be knowledgeable about the features of the drug alternatives available for the illness being managed in order to act as motivators for medication adherence. The education of healthcare providers can be actively improved by regular hospital grand rounds and ongoing pharmaceutical education. The advantages and downsides of each pharmacological option can be discussed by healthcare professionals as part of a care protocol. The study guide for providers may include topics such as brand-name versus generic drug costs, drug side effects, and the frequency with which patients would take a given medication. The providers are better able to relate to the patients' realities when they are aware of the characteristics of the drugs.
Communication
Strong patient-provider relationships and the capacity of providers to communicate with beneficiaries go beyond what is known to them. Compliance can be increased by having strong interpersonal and communication skills that are infused with empathy and an understanding of the difficulties that patients have when trying to take drugs for both acute and chronic illnesses. Community pharmacists can open a line of contact to patients with dignity, respect, and understanding as fulcrums because of their close proximity to the community. By raising awareness, acting as admirable role models, and sharing any personal testimony they may have, providers play a crucial role in promoting compliance. By implementing agreed-upon reminders via text messages, emails, automated calls, and weekly postal letters, they can promote compliance. This step can lessen the unexpected consequences of amnesia.
Material and Method
Patients’ education
The best way to increase drug adherence is through patient education. Compliance can be encouraged by being aware of the consequences of disobeying the healthcare provider's prescription medicine use recommendations. Compliance can also be improved by being aware of how crucial it is to keep appointments for routine follow-ups and clinic visits. Any of the following methods can be used to deliver these messages
Advocacy
Patients' capacity to finance and follow treatment plans may be hampered by the high expense of healthcare in the US and other countries. Therefore, providers might support legislative initiatives through their various associations or bodies that call for a cap on out-of-pocket expenses for all prescription pharmaceuticals based on the socioeconomic status and income of the patient population served. Providers can inform political authorities about the significance of being at the forefront of improving health outcomes and how to enhance results because the cost of medications that puts fewer burdens on patients' budget can boost refills and adherence. Providers can also press legislators to pass health-related laws with an emphasis on prescription drug costs, accessibility, and availability.
Adaptation of medications
Despite the US's programmes for medication synchronization, packaging, and delivery services making it simple to get medications, a universal implementation of these initiatives could result in better patient outcomes because of the impact of population expansion and global connection. When possible, producers can make sure that every drug has various forms, such as a liquid or solid, to satisfy patients' preferences, taking into account non-adherence caused by the physical qualities of medicines. To facilitate a less frequent administration, manufacturers can modify the potency, bioavailability, and dose regimens of drugs. For instance, using slow-release capsules that patients can take once a week can promote compliance and refills, especially in those who get polypharmacy. Compliance can be improved by giving patients the choice to choose between capsules and tablets. Because everyone's desires, tastes, and wants are different, it is possible to flavor medicines, giving them a pleasing appearance and enhancing users' spirits. Researchers can keep trying to reduce the adverse effects of currently available drugs.
CONCLUSION
The current state and affecting factors of nurses' core competences in burn departments in China are reported in this study, which is the first in its field to do so in China. According to our findings, burn nurses had average core competences, with professional titles, Bicu experience, and time of employment all appearing to have an impact. Future experimental studies must concentrate on how to train burn nurses to perform their many duties as clinical practitioners, educators, researchers, administrators, advisors, and coordinators. In order to improve burn nurse training, we intend to offer additional proof.