Molding with bonded conical transfers: A new technique
Received: 08-Dec-2017 Accepted Date: Jan 02, 2018; Published: 04-Jan-2018
Citation: Elimario R, Geraldo CAP, Simone K, et al. Molding with bonded conical transfers: A new technique. Dentist Case Rep 2018; 2(1):14-17.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
OBJECTIVE: To evaluate the dimensional accuracy of two different molding techniques for multiple prostheses on implants-molding with bonded square transfers using an open individual impression tray, and molding with bonded conical transfers using closed individual impression tray, a variation of the conventional technique.
MATERIALS AND METHODS: A master model was created to simulate the condition of missing teeth and fitted implants, using, thus, three implants out of alignment. A superstructure was used as measurement template and to measure adaptation in the specimens (25 for each molding technique). The transfers were bonded with self-polymerized acrylic resin. Molding procedures were performed using individual impression trays and addition silicone Futura regular fluid. The models were produced in plaster rock type IV Fuji-Rock. Measurements were obtained using Scan Electron Microscopy.
RESULTS: Data relative to disadaptation measurements were analyzed with Student’s t-test for independent samples. The mean disadaptation of the master model was 4.491 µm; the open impression tray molding was 9.546 µm (standard deviation 0.893); and the closed impression tray molding, 8.033 (standard deviation 0.431).
CONCLUSION: The molding technique with closed impression tray and conical transfers showed a significantly higher performance in comparison to the open impression tray technique with bonded square transfers.
Keywords
Prostheses and implants; Dental impression technique; Dental implants
The evolution of implantodontics can be observed on planning, techniques and results. This specialty has become a reality and has reached high rates of success.
In prosthetic rehabilitation on implants, all steps are significant and influence the final result. Transfer molding of implants aims to accurately replicate the location of implants in the mouth onto the model. The most accurate or most adequate technique for each situation is still a subject of debate among professionals. The accuracy of molding can be affected by angle and number of implants, molding material, type of impression tray and of prosthetic connector, as well as by the bonding of transfers [1-4]. Accuracy of this casting influences the prosthetic structure that will be mounted on the implants.
The total passivity of prosthesis on an implant is hard to be obtained due to variables such as implant position and/or angle and is a problem for specialists [5]. The lack of passivity of the infrastructure has been cited as one of the factors leading to biological complications and mechanical flaws of the prosthesis-implant system components. These complications are due to the disadaptation of the implant-prosthesis marginal junction and might cause unfavorable responses both of soft and hard tissue since it favors plaque accumulation [6-10].
Among the most commonly used methods to assess prostheses adaptation are radiographies, probing, screw torque, sensitivity, and the professional’s discretion. However, those are subjective means of assessment and are, thus, more prone to inaccuracies [11].
Some studies have compared the effectiveness of different implant molding techniques [12-15], since the accuracy of the impression will influence the prosthesis adaptiveness [6,9]. One study has showed a 50% rate of prostheses defects related to molding procedures and 50% related to manufacturing procedures on the prostheses laboratory [10].
Given the described context, the assessment of the dimensional accuracy of two molding techniques of multiple prostheses on implant seems relevant. The techniques addressed here are bonded square transfer molding using an open individual impression tray (direct technique) and technique-varying molding with bonded conical transfers using a closed individual impression tray (indirect technique).
Material and Methods
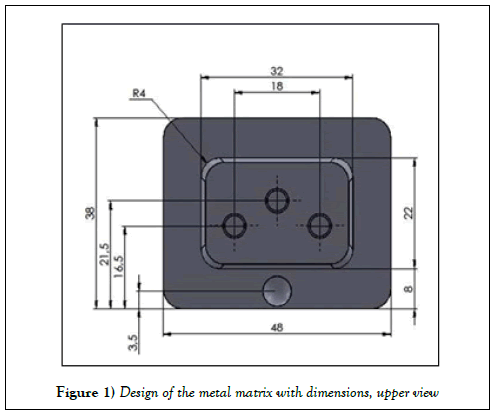
A metal matrix was designed using the image software SOLIDWORKS. Three cavities, designed to hold Micro Unit abutment analogs (A.S. Technology-São José dos Campos - SP-Brazil), were evenly positioned on the top of the matrix, according to Figure 1. A fourth cavity was placed on the master model to standardize the impression tray positioning. The piece was machined in a 5-axis machining center DMU 50 ECO (DMG MORI SEIKI CO., LTDA - Japan).
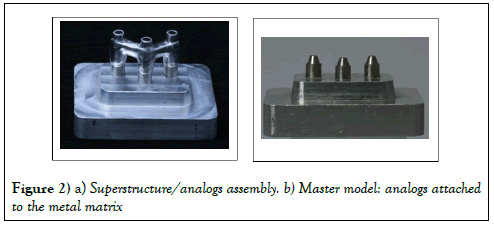
The abutment analogs were temporarily mounted on the cavities for the superstructure framework (Figure 2a), which serves, at this moment, as a template and, later, will be used to measure the specimens adaptation.
The superstructure was casted in cobalt-chrome alloy Star Loy C (DentsplyDeguDentGmbH-Germany) as a weldless monoblock. Following casting and finishing, the analogs mounted on the metal matrix were removed, fitted to the superstructure and attached to the matrix cavities using self-polymerized acrylic resin PatternResin (GC AmericaInc.Ailsip-IL, USA) (Figure 2b) for the master model framework. The interval between fixation and molding was 24 hours.
The analogs were identified from right to left with the numbers 1, 2, 3.
Another matrix was manufactured in removable Teflon with the aim of allowing the visualization of the superstructure/analog connection. This Teflon matrix was replicated in condensation polymerized silicone Clonage Fluido (DFL Indústria e comércio S.A. Rio de Janeiro-RJ. Brazil).
The individual metal impression trays were made in aluminum designed with the design software Solid works and machining software Edge am lathe (5-axis machining center DMU 50 ECO (DMG MORI SEIKI CO., LTD-Japan). Measurements were based on the master model, with an inner relief of 5-mm for thickness uniformity and standard amount of material for molding.
These impression trays have a round projection that functions as a guide during molding, fitting the recession in the master model. In addition to that, they have holes to retain the molding material.
The same impression tray was used in both molding techniques. In the molding with the open impression tray, the upper holes allowed access to the square transfer screw, and in the molding with the closed impression tray, they favored material retention.
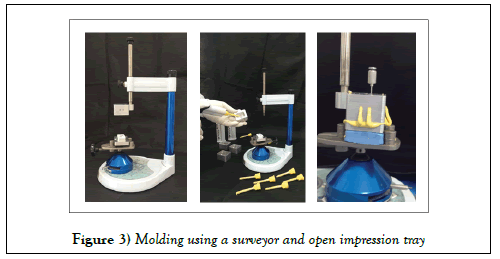
A Bio-Art surveyor B2 (Bio-Art Equipamentos Odontológicos LTDA - São Carlos-SP-Brazil) was used to standardize the metal matrix positioning as well as the insertion and removal axis of the impression tray and molding material assembly. The table was tied to the surveyor using double-sided adhesive tape (Cremer S.A - Blumenau - SC - Brazil) and the metal matrix was tied to the table.
All twenty-five moldings for each transfer technique were fabricated in the same environment, at 23°C. As molding material, we used addition silicone Futura with regular consistency (DFL Indústria e comércio S.A. Rio de Janeiro-RJ - Brazil), which was inserted in the impression tray that was, then attached to the surveyor guide pin (Figure 3).
The same person was responsible for all moldings, obeying the time of eight minutes before handling and polymerizing, as recommended by the manufacturer. Following each molding, the master model was cleaned with alcohol to prepare it for the new molding process.
In the molding using square transfers, the transfers were bonded with dental floss Hillo (Hillo Ind. E Com. Ltda. Aperibe-RJ- Brazil) and selfpolymerized acrylic resin PatternResin (GC AmericaInc.Ailsip-IL, USA), severed and bonded again. We used open individual impression trays and, following polymerization, the excess of molding material was removed on the upper part of the tray, giving access to the transfers screws, which were then loosened. The impression tray, molding material and transfer assembly was removed from the metal matrix. The analogs were attached to the transfers with a torque of 15N using a hand-operated prosthesis torque meter (A.S. Technology - São José dos Campos - SP - Brazil).
In the technique-varying molding, the traditional conical transfers were replaced by titanium copings for microunit abutment (A.S. Technology–São José dos Campos–SP, Brazil). A metal matrix standardized the amount of self-polymerized acrylic resin PatternResin (GC AmericaInc.Ailsip-IL, USA) on the splinting of the transfers, which were applied over the positioned Teflon matrix.
The waiting time before proceeding with the molding with the closed impression tray conventional technique was 17 minutes. After polymerization, the assembly impression tray and molding material was removed from the master model. The bonded titanium copings were removed from the master model, attached to the modeling analogs and inserted in the closed impression tray using molding material, in the same way as in the transference molding, also known as indirect technique.
The Teflon matrix used for the visualization of the connection between suprastructure and abutment was applied to the mold obtained using an intraoral plastic molding syringe JON (Jon Produtos Odontológicos. São Paulo -SP- Brasil). Also, before modeling, an artificial gingiva was applied to the moldings.
An aluminum metal matrix for plaster pouring was manufactured and attached to the outer area of the impression tray. This matrix was designed and machined using the softwares Solidworks and Edgecam, respectively, and lathed (5-axis machining center DMU 50 ECO (DMG MORI SEIKI CO., LTD - Japan). The use of this matrix aimed at standardizing the shape of the models and the amount of modeling material, as well as avoiding the leakage of plaster during pouring.
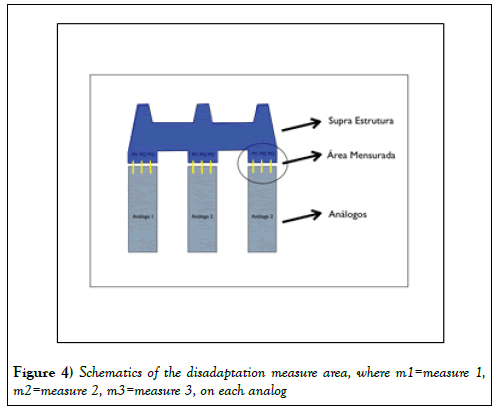
The same modeling procedure was used for both molding techniques. The material used was a Type IV resin plaster stone Fuji-Rock (GC America Inc. Ailsip-IL, USA). Plaster was prepared by a vacuum-mixing machine (AMANNGIRRBACH smartmix-X2- Austria), according to the manufacturer’s recommendations. The waiting time for the complete setting of the plaster was 2 hours for each model. The measurement of adaptation was taken after 120 h, according to 25 ADA Standard. The superstructure was attached to the master model and to the specimens with a 15N torque, standardized with a prosthesis torque meter (A.S. Technology - São José dos Campos - SP - Brazil). The first measurements were taken on the superstructure on the master model. On each analog, the mean disadaptation was measured at three points (Figure 4) that are called primary comparative measures.
The same measurement method was used for all specimens.
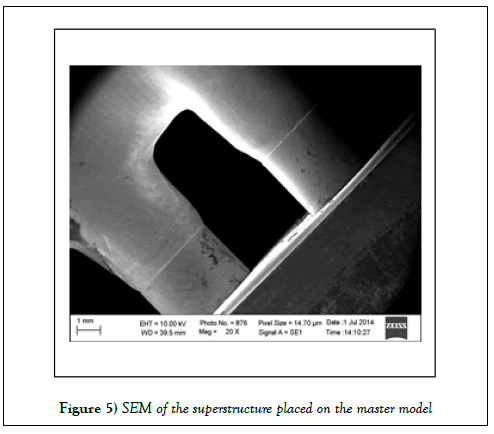
All images and measurements were taken at the research laboratory of the Fundação Oswaldo Cruz (Fiocruz - Rio de Janeiro - RJ – Brazil) and obtained in a scanning electron microscope ZEISS EVO MA 10 (Carl Zeiss - Germany) - Figure 5 and software Smart 100 (ProData Technology LTDA). Data were submitted to statistical analysis.
Results
In order to investigate if the molding technique influenced disadaptation between analogs and the metal superstructure, Student’s t-test for independent samples was applied to the measurements obtained with the open and closed impression trays.
Student’s t-test for one sample was applied to the disadaptation measures between the analogs and the metal superstructure for the molding techniques with open and closed impression trays comparing to the mean values obtained for control, where superstructure disadaptation was measured relative to the master model.
All statistical tests were performed in SPSS 20 (SPSS INC., Chicago, IL, USA), with a significance level of 5%.
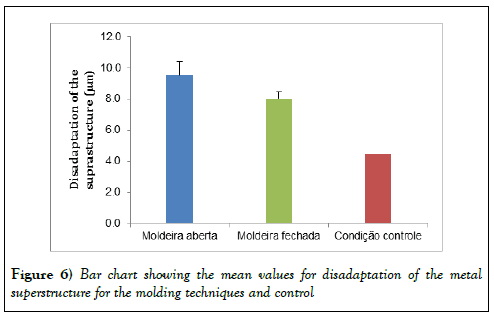
T-test for independent samples shows that the molding technique significantly influenced disadaptation between the analogs and the metal suprastructure (p<0.001), and that the closed impression tray resulted in a significantly lower disadaptation in comparison to the open impression tray (Figure 6).
Student’s t-test for one sample shows a disadaptation between analogs and the metal superstructure resulting from molding with the open impression tray of 9.546 μm and standard deviation of 0.893 μm, which significantly differ (p<0.001) from that found for control, where disadaptation was measured as 4.491 μm relative to the master model. The same result was found using the closed impression tray, with disadaptation measurement of 8.033 μm and standard deviation of 0.431 μm, also significantly larger than the ones found with control (Student’s t-test for one sample: p<0.001), as shown in Figure 6.
Discussion
Complications resulting from the lack of passive adaptation in prosthesis on implants have been object of studies; however, how this lack of adaptation influences mechanical and biological complication factors is still unclear. Among mechanical complication factors, we can mention prosthesis screw loosening, and fracture of screws, prosthesis and implants. The disadaptation of the piece can favor the accumulation of plaque and affect soft and hard tissues surrounding the implant, which might cause peri-implantitis. The acceptable threshold of 15 μm [16] cannot be observed with the conventional methods of clinical evaluation, such as periapical radiography, probing, tactile response to screw torque, and patient’s perception. Faria et al. [11] and Branemark [17] consider that disadaptations of up to 10 μm can be tolerated, being favorable not only to the prosthesis lifespan, but also the whole implanter and peri-implantar systems’ lifespan. Here, we found mean disadaptation measures lower than 10 μm, regardless the molding technique employed (9.546 μm with open impression tray and 8.033 μm with closed impression tray).
The superstructure components used in this study were factory-machined, which reduces the changes in the laboratory processes. Some authors found similar results comparing inner adaptation of burned and machined pieces [18]. Some other works compared the marginal fitting with mad/ cam (manual aided design/computer-assisted manufacturing) and cad/ cam (computer-aided design/computer-assisted manufacturing) of several systems, concluding that the marginal adaptation does not depend solely on the manufacturing system [8].
Torque used to attach the superstructure to the master model and to the specimens is 15 Ncm, following the manufacturer’s recommendations. Some studies use a torque of 10 Ncm [1,3,16-22], or of 30 Ncm [11,21]. Lee and Gallucci [13] report that torque should be maintained within the range of 10 Ncm to 30 Ncm and should obey the manufacturer’s recommendations.
The precise replication of the implants’ positioning on the models is essential for the production of an accurate prosthesis. To achieve this, a reliable molding technique should be chosen. It is, indeed, widely accepted that a good molding is the first step for prosthesis with less disadaptation [6]. Factors such as type of transference, transfer bonding, implants and abutments angle, number of implants, impression material, type of impression tray, and type of prosthesis connection may influence the moldings [1]. Some authors add to this list the pressure exerted by the fingers during the molding process [2]. Here, the implants were evenly distributed, with no angulation, we used a reduced number of analogs and the same molding material in all the groups to reduce the number of variables and assess only molding techniques.
Some studies have evaluated the best molding techniques for prostheses on implants [1,3,4,11]. Some works have shown satisfactory results [6] for all techniques, but a better performance of the direct technique with bonded transfers [11,20]. However, some authors failed to show significant differences between molding techniques [3,4].
Some authors considered the use of materials such as polyether and/or polyvinyl siloxane associated with individual impression trays and transfers as the best option [23,24]. Thus, polyvinyl siloxane was the choice material of this study.
The individual impression tray was used in this work because it has been the choice of the majority of authors [1,11,25]. They allow use a uniform amount of molding material [26,27]. However, some authors compared conventional individual impression trays with modular individual impression trays, and found less distortion with the latter [26].
According to some authors, the bonding of transfers before molding associated with the use of individual impression trays is the technique that produces the best results [11,21,28]. On the other hand, other works have shown similar results when comparing the techniques with and without bonding [19,29]. This study shows variation of a technique using closed impression tray, replacing the conical transfers with titanium copings for Micro Unit abutment. This replacement because the transfers must be splinted, which is not possible with conventional conical transfers, which are manufactured as a single piece and must rotate in insertion and removal of implants. The results were better than those obtained with the open impression tray and bonded transfers. Some authors have shown variation of techniques that produced satisfactory results, showing that the information obtained can be used and adapted to the materials one is more acquainted with, aiming at obtaining more accurate implant transfer moldings [14,20,28].
Conclusion
Based on the results showed here, we conclude that the molding technique using closed impression trays and bonded conical transfer’s shows a better performance if compared with the molding technique using open impression trays and bonded square transfers.
REFERENCES
- Lee YJ, Heo SJ, Koak JY, et al. Accuracy of different impression techniques for internal-connection implants. Int J Oral Maxillofac Implants. 2009;24(5):823-30.
- Uludag B, Cogalan K, Polat S. An alternative impression technique for implant-retained overdentures with locator attachments. J Oral Implantol. 2010;36(6):451-3.
- Alikhasi M, Siadat H, Monzavi A, et al. Three-dimensional accuracy of implant and abutment level impression techniques: effect on marginal discrepancy. J Oral Implantol. 2011;37(6):649-57.
- Chang WG, Vahidi F, Bae KH, et al. Accuracy of three implant impression techniques with different impression materials and stones. Int J Prosthodont. 2012;25(1):44-7.
- Stimmelmayr M, Erdelt K, Güth JF, et al. Evaluation of impression accuracy for a four-implant mandibular model - a digital approach. Clin Oral Investig. 2012;16(4):1137-42.
- Lee H, Ercoli C, Funkenbusch PD, et al. Effect of subgingival depth of implant placement on the dimensional accuracy of the implant impression: an in vitro study. J Prosthet Dent. 2008;99(2):107-13.
- Mombelli A. Etiology, diagnosis, and treatment considerations in peri-implantitis. Curr Opin Periodontol 1997;4:127-136.
- Karatasli O, Kursoglu P, Capa N, et al. Comparison of the marginal fit of different coping materials and designs produced by computer aided manufacturing systems. Dent Mater J. 2011;30(1):97-102.
- Hjalmarsson L, Örtorp A, Smedberg JI, et al. Precision of fit to implants: a comparison of Cresco™ and Procera® implant bridge frameworks. Clin Implant Dent Relat Res. 2010;12(4):271-80.
- Heckmann SM, Karl M, Wichmann MG, et al. Cement fixation and screw retention: parameters of passive fit. An in vitro study of three-unit implant-supported fixed partial dentures. Clin Oral Implants Res. 2004;15(4):466-73.
- Faria JCB, Silva-ConcÃÂlio LR, Neves ACC, et al. Evaluation of the accuracy of different transfer impression techniques for multiple implants. Braz Oral Res. 2011;25(2):163-7.
- Karl M, Graef F, Schubinski P, et al. Effect of intraoral scanning on the passivity of fit of implant-supported fixed dental prostheses. Quintessence Int. 2012;43(7):555-62.
- Lee SJ, Gallucci GO. Digital vs. conventional implant impressions: efficiency outcomes. Clin Oral Implants Res. 2013;24(1):111-5.
- Joda T, Wittneben JG, Brägger U. Digital implant impressions with the "Individualized Scanbody Technique" for emergence profile support. Clin Oral Implants Res. 2014;25(3):395-7.
- Von See C, Wagner ME, Schumann P, et al. Non-radiological method for three-dimensional implant position evaluation using an intraoral scan method. Clin Oral Implants Res. 2014;25(9):1091-3.
- Tiossi R, Rodrigues RC, de Mattos MG, et al. Comparative analysis of the fit of 3-unit implant-supported frameworks cast in nickel-chromium and cobalt-chromium alloys and commercially pure titanium after casting, laser welding, and simulated porcelain firings. Int J Prosthodont. 2008;21(2):121-3.
- Brånemark PI. Osseointegration and its experimental background. J Prosthet Dent. 1983;50(3):399-410.
- Malaguti G, Denti L, Bassoli E, et al. Dimensional tolerances and assembly accuracy of dental implants and machined versus cast-on abutments. Clin Implant Dent Relat Res. 2011;13(2):134-40.
- Philips KM, Nicolls JI, Rubenstein TM. The accuracy of three implant impression techniques: a three-dimensional analysis. Int J Oral Maxilofac Implants. 1994;9(5):533-40.
- Assif D, Marshak B, Schmidt A. Accuracy of implant impression techniques. Int J Oral Maxillofac Implants. 1996;11(2):216-22.
- Paiva J, Givan DA, Broome JC, et al. Comparison of the passivity between cast alloy and laser-welded titanium overdenture bars. J Prosthodont. 2009;18(8):656-62.
- Jaarda MJ, Razzoog ME, Gratton DG. Providing optimum torque to implant prostheses: a pilot study. Implant dent 1993;2(1):50-52.
- Branemark P-I, Zarb GA, Albrektsson T. Tissue-integrated prostheses. Chicago: Quintessence; 1985.352.
- Assunção WG, Gennari Filho H, Zaniquelli O. Evaluation of transfer impressions for osseointegrated implants at various angulations. Implant Dent 2004;13(4):358-366.
- Assunção WG, Cardoso A, Gomes EA, et al. Accuracy of impression techniques for implants. Part 1-Influence of transfer copings surface abrasion. J Prosthodont. 2008;17(8):641-7.
- Simeone P, Valentini PP, Pizzoferrato R, et al. Dimensional accuracy of pickup implant impression: an in vitro comparison of novel modular versus standard custom trays. Int J Oral Maxillofac Implants. 2011;26(3):538-46.
- Alikhasi M, Bassir SH, Naini RB. Effect of multiple use of impression copings on the accuracy of implant transfer. Int J Oral Maxillofac Implants. 2013;28(2):408-14.
- Vigolo P, Majzoub Z, Cordioli G. In vitro comparison of master cast accuracy for single-tooth implant replacement. J Prosthet Dent. 2000;83(5):562-6.
- Carr AB, Sokol J. Accuracy of casts produced by the Nobelpharma impression techniques. J Dent Res. 1991;70:290.