Morphological variation of thoracic splanchnic nerves in selected Ethiopian cadavers, Gondar and Mekelle Ethiopia
2 Department of Anatomy, School of Medicine, College of Medicine and Health Sciences, Addiss Ababa University, Addiss Ababa, Ethiopia
3 Department of Surgery, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Received: 06-Aug-2018 Accepted Date: Aug 21, 2018; Published: 30-Aug-2018
Citation: Gebretsadik MA, Mulu A, Dessie MA, et al. Morphological variation of thoracic splanchnic nerves in selected Ethiopian cadavers, Gondar and Mekelle, Ethiopia. Int J Anat Var. 2018;11(3):93-98.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Patients with chronic pancreatic carcinoma and cancer of the pancreas often experience severe pain. Sympathatictomy and celiac ganglia blockage or distraction has been applied with varying degree of efficacy in the relief of pain. This variability of efficacy may be due to anatomical variation in the location of the celiac ganglia and thoracic splachnic nerves.
Aim: This study aims to describe the location and the variability of thoracic splanchnic nerves in selected Ethiopian cadavers.
Methods: It is an observation based descriptive study on 10 selected Ethiopian cadavers. Both adult and fetal cadavers were dissected after embalming in formalin. This study was from January-June 2011. Purposive sampling technique was used. The thoracic splanchnic nerves were exposed in the left and the right side of the cadavers. The anatomy and the relationships between the thoracic sympathetic ganglia, sympathetic chains, and thoracic splanchnic nerves were inspected on both sides of the posterior thoracic wall.
Result: The three splanchnic nerves were present in all cadavers. The greater splanchnic nerves were formed by nerve branches from the T4–T11 thoracic sympathetic ganglia and the most common type was formed by T7-T10 (35%), followed by T6-T10 (20%). The T11 forms ganglionic array of lesser splanchnic nerves in 45% of cases. The least splanchnic nerves were formed by T12 in 70% of the cadavers.
Conclusion: Significant variations in the formation of the thoracic splanchnic nerves and the communication between them were observed. The pattern of the formation and structure of the TSNs was not only varying from person to person but also between the right and left side.
Keywords
Thoracic; Splanchnic nerves; Splanchnicectomy
Abbreviations
GSN: Greater Splanchnic Nerve; LSN: Lesser Splanchnic Nerves; lSN: Least Splanchnic Nerves; TSN: Thoracic Splanchnic Nerves
Introduction
The sympathetic chains are bilateral ganglionated nerve cords lying on either side of the vertebral column, extending from the cranial base to the coccyx [1]. The splanchnic nerves are the sympathetic nerves for the abdominal and pelvic viscera [1-3]. They include the thoracic splanchnic nerves (greater, lesser and least), lumbar splanchnic nerve, sacral splanchnic nerve and pelvic splanchnic nerve [3]. The thoracic splanchnic nerves (TSN) are medial branches of the thoracic sympathetic trunk [4]. The preganglionic fibers from T5 to T10 form the greater splanchnic nerve (GSN), which ends mainly in corresponding celiac ganglia and partly in the aorticorenal ganglion and suprarenal gland. The preganglionic fibers from T10 to T11 ganglia forming the lesser splanchnic nerves (LSN) end in the aorticorenal ganglion and fibers from T11 to T12 ganglia forming the least splanchnic nerves (lSN) end in the renal plexus [2,5]. These splanchnic nerves contain, predominantly, visceral efferent fibres, as well as pain conducting visceral afferent fibres [6,7]. The TSNs and celiac ganglia have been of anatomical and clinical interest in the fields of pancreatic cancer and pancreatitis for many years, particularly for their role in pain management [8-10].
The management of pancreatic carcinoma and pancreatic cancer has been a challenging for the patient and treating physicians [9]. Splanchnicetomy is a surgical interruption of splanchnic nerves for management of pain caused by chronic pancreatitis, carcinomas of the pancreas, liver, gallbladder, alimentary tract from the stomach to the transverse colon, omentum and mesentery [2,6,11,12]. Nowadays, most surgical splanchnicectomies are performed to control intractable pain from the upper abdominal organs [13]. One of the main problems in the use of thoracoscopic splanchnicectomy for pain relief is the uneven result of the procedure, mainly because of insufficient anatomical information. Most of the anatomy textbooks describe little variations in the anatomy of the TSNs, only adequate for medical students and physicians to explain the mechanism of visceral pain sensation and the disease to their patients. Surgeons and anesthesiologists, however, require more detailed anatomical information. As a result, surgical trials based on such scant information often lead to uneven degrees of symptom relief. Success rates for pain management following splanchnicectomy vary from 60% to 90% between different surgeons [14]. These results are not due to the differing levels of skill among surgeons, but to the lack of established surgical protocol based on well-defined anatomical information [15].
A number of authors in the 1930s-1960s argued that the highest root of the GSN is as high as thoracic spinal cord segments 4 or 5 [16-19]. In recent studies, T3 has been reported as the highest level of origin of GSN [1,5,7].
Edwards and Baker noted the origin of the LSN as high as T7 and Reed found the origin of the LSN to be from the T9 to 12 sympathetic ganglia [7, 8]. Yang et al noted the origin of the LSN from T8 to T12 and lSN from T10 to L1 [20]. Five different categories of lSN have been reported [21]. Jit and Mukerjee found lSN in 37% of cases arising predominantly from a single root [7].
More detailed anatomical information about TSNs will help physicians in their quest for more precise practice. In Ethiopia, there was no study on morphological variations of the TSNs. Thus, the current study attempted to provide a more comprehensive and detailed, but the uncomplicated anatomical description of TSNs that could be useful to medical students and specialists. The benefit of more precise knowledge, thereby obtained would be a basis for more accurate localization and interruption by treating clinicians to potentially improve clinical outcome. The purpose of this study was to investigate the level of origin, the pattern of formation and other morphological variations of TSNs in selected Ethiopian cadavers.
Materials and Methods
An observational, descriptive study was conducted in selected Ethiopian cadavers. The study was conducted on cadavers available at the University of Gondar and Mekelle University in the department of human anatomy dissection room. Both adult and fetal cadavers were used. The cadavers were embalmed according to conventional methods for routine anatomy classes. The study period was from January to June 2011. Purposive sampling technique was used. Those cadavers which did not have any gross birth defect, particularly of the nervous system, were selected for the present study.
Cadavers which had been damaged in their thoracic and posterior abdomen wall, cadavers with congenital deformity of thoracic wall or adherent pleura, and in those cadavers where the TSNs were damaged during dissection were excluded. The anatomy and the relationships between the thoracic paravertebral sympathetic ganglia, sympathetic chains, and TSNs were inspected in 20 sides of the posterior thoracic and abdominal wall. The clavicles were separated from the manubrium of the sternum, the ribs were cut off at the mid-axillary line, and the anterior chest wall was removed. After removal of the lungs and the major contents of the mediastinum, the parietal pleurae were carefully stripped to expose the thoracic paravertebral sympathetic ganglia, sympathetic chains, and TSNs. The majority of the diaphragms were removed except for the portions that were attached to the posterior thoracic wall.
The TSNs were exposed in the left and the right side of the cadavers. After identification of the thoracic sympathetic ganglia, sympathetic chains, and TSNs; the connections between the ganglia and TSNs were traced by naked eye. All of the dissected materials were photographed using a digital camera. After the dissection, the dissected specimens were checked out for the completeness, accuracy, and clarity by the supervisors. The quality checking was done at the end of each dissection and cross-checking was done before analysis.
Thematic approach was applied to compile and analyze findings on TSNs. Observation was recorded and transcribed for analysis purpose using thematic analysis. This procedure contributed a lot in the design and development of the anticipated TSNs. Numerical data on the uppermost ganglion, lowermost ganglion, participation of ganglia, and the number of roots of the GSN, LSN, and lSN were divided by sides for comparison of their distribution in the left and right thoracic walls. Analysis was performed manually using a thematic approach.
Study subjects were prepared for teaching purposes in the department of anatomy. Ethical clearance was obtained from Research and publication office of the University of Gondar and Ayeder referral hospital.
Results and Observation
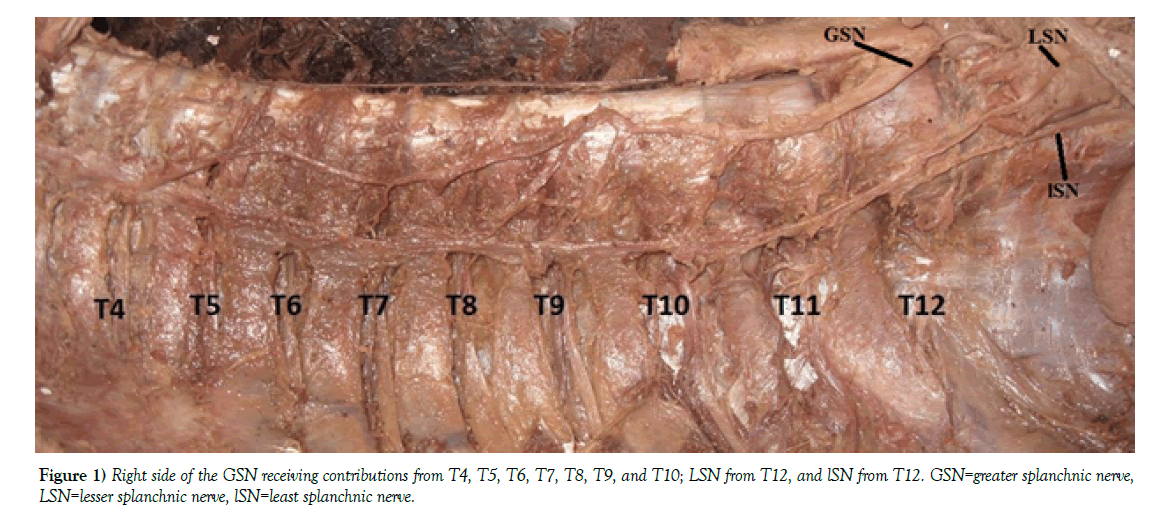
A total of ten cadavers were observed on both sides. Ganglia T4 to T11 levels gave branches to the GSNs. The most frequently seen uppermost thoracic sympathetic ganglion connected to the GSN has been at the T7 level, which accounts 45% (9/20) of the cases. In the right side, the ganglia at the level of T6 contributed to uppermost ganglia of 60% of the cases (Tables 1 and 2). The lowermost ganglion which participates in the formation of the GSN was most frequently at the T10 level observed in 70% (14/20) of cases (Table 3). The ganglion most frequently produces GSN was T8 level produced the root of the GSN in 95% of the cadavers (Figure 1 and Table 4).
Level of cadaver |
Greater Splanchnic nerve | Lesser Splanchnic nerve | Least Splanchnic Nerve | |||
|---|---|---|---|---|---|---|
| Side | Side | Side | ||||
| Left side (n=10) | Right side (n=10) | Left side (n=10) | Right side (n=10) | Left side (n=10) | Right side (n=10) | |
| Cadaver 1 | T7,T8, T9, T10 | T6,T7,T8,T9,T10 | T11 | T11 | T12 | T12 |
| Cadaver 2 | T7,T8 T9 T10 | T6,T7,T8,T9,T10,T11 | T11 | T11, T12 | T12 | T12 |
| Cadaver 3 | T7,T8,T9,T10 | T7,T8,T9,T10,T11 | T11 | T12 | T12 | T12 |
| Cadaver 4 | T5,T6,T7,T8,T9,T10,T11 | T4,T5,T6,T7,T8,T9, T10 | T12 | T12 | T12 | T12 |
| Cadaver 5 | T7, T8 | T8, T9 | T10, T11 | T10,T11, T12 | T11, T12 | T12 |
| Cadaver 6 | T8, T10 | T6, T9, T10 | T11 | T10 | T12 | T11, T12 |
| Cadaver 7 | T7,T8,T9,T10 | T6,T7,T8,T9, T10 | T11 | T10 | T12 | T11, T12 |
| Cadaver 8 | T6,T7,T8,T9,T10 | T6,T7,T8,T9,T10,T11 | T11 | T11, T12 | T11, T12 | T11, T12 |
| Cadaver 9 | T7,T8,T9,T10 | T7,T8,T9,T10 | T11 | T10, T11 | T11, T12 | T12 |
| Cadaver10 | T7,T8,T9,T10 | T6,T7,T8,T9,T10 | T11 | T11, T12 | T12 | T12 |
Table 1: Origin of Thoracic Splanchnic Nerves in 10 selected Ethiopian cadavers
| TSN | Greater Splanchnic Nerves | Lesser Splanchnic Nerves | Least Splanchnic Nerves | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Root | Left (n=10) | Right (n=10) | Total (n=20) | Left (n=10) | Right (n=10) | Total (n=20) | Left (n=10) | Right (n=10) | Total (n=20) |
| T4 | - | 10%(1/10) | 5%((1/20) | - | - | - | - | - | - |
| T5 | 10%(1/10) | - | 5%((1/20) | - | - | - | - | - | - |
| T6 | 10%(1/10) | 60%(6/10) | 35%(7/20) | - | - | - | - | - | - |
| T7 | 70%(7/10) | 20%(2/10) | 45%(9/20) | - | - | - | - | - | - |
| T8 | 10%(1/10) | 10%(1/10) | 10%(2/20) | - | - | - | - | - | - |
| T9 | - | - | - | - | - | - | - | - | - |
| T10 | - | - | - | 10%(1/10) | 40%(4/10) | 25%(5/20) | - | - | - |
| T11 | - | - | - | 80%(8/10) | 40%(4/10) | 60%(12/20) | 30%(3/10) | 30%(3/10) | 30%(6/20) |
| T12 | - | - | - | 10%(1/10) | 20%(2/10) | 15%(3/20) | 70%(7/10) | 70%(7/10) | 70%(14/20) |
Table 2: The Uppermost Ganglia Contributing to the Thoracic Splanchnic Nerves
| Greater splanchnic nerve | Lesser splanchnic nerve | Least splanchnic nerve | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Root | Left (n=10) | Right(n=10) | Total(n=20) | Left(n=10) | Right(n=10) | Total(n=20) | Left(n=10) | Right(n=10) | Total(n=20) |
| T8 | 10%(1/10) | - | 5%(1/20) | - | - | - | - | - | - |
| T9 | - | 10%(1/10) | 5%(1/20) | - | - | - | - | - | - |
| T10 | 80%(8/10) | 60%(6/10) | 70%(14/20) | - | 20%(2/10) | 10%(2/20) | - | - | - |
| T11 | 10%(1/10) | 30%(3/10) | 20%(4/20) | 90%(9/10) | 20%(2/10) | 55%(11/20) | - | - | - |
| T12 | - | - | - | 10%(1/10) | 60%(6/10) | 35%(7/20) | 100% (10/10) | 100% (10/10) | 100% (20/20) |
Table 3: The Lowermost Ganglia Contributing to the Thoracic Splanchnic Nerves
Root |
Greater splanchnic nerve | Lesser splanchnic nerve | Least splanchnic nerve | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Left (n=10) | Right (n=10) | Total (n=20) | Left (n=10) | Right(n=10) | Total(n=20) | Left(n=10) | Right (n=10) | Total (n=20) | |
| T4 | - | 10% (1/10) | 5% (1/20) | - | - | - | - | - | - |
| T5 | 10% (1/10) | 10% (1/10) | 10% (2/20) | - | - | - | - | - | - |
| T6 | 20% (2/10) | 70% (7/10) | 45% (9/20) | - | - | - | - | - | - |
| T7 | 90% (9/10) | 80% (8/10) | 85% (17/20) | - | - | - | - | - | - |
| T8 | 100%(10/10) | 90% (9/10) | 95% (19/20) | - | - | - | - | - | - |
| T9 | 80% (8/10) | 100% (10/10) | 90% (18/20) | - | - | - | - | - | - |
| T10 | 90% (9/10) | 90% (9/10) | 90% (18/20) | 10% (1/10) | 40% (4/10) | 25% (5/20) | - | - | - |
| T11 | 10% (1/10) | 30% (3/10) | 20% (4/20) | 90% (9/20) | 60% (6/10) | 75% (15/20) | 30% (3/10) | 30% (3/10) | 30% (6/20) |
| T12 | - | - | - | 10% (1/10) | 60% (6/10) | 35% (7/20) | 100% (10/10) | 100% (10/10) | 100% (20/20) |
Table 4: The Participation Rate of Thoracic Ganglia in Splanchnic Nerves
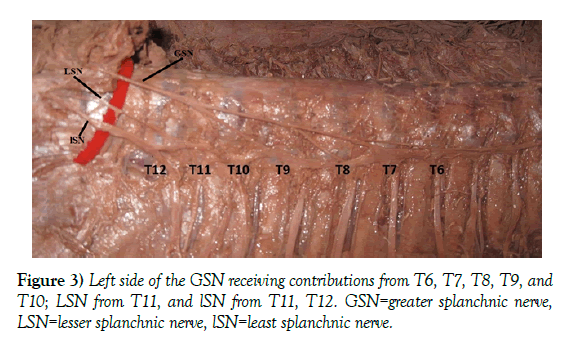
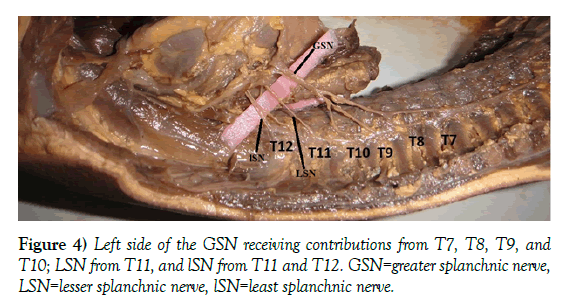
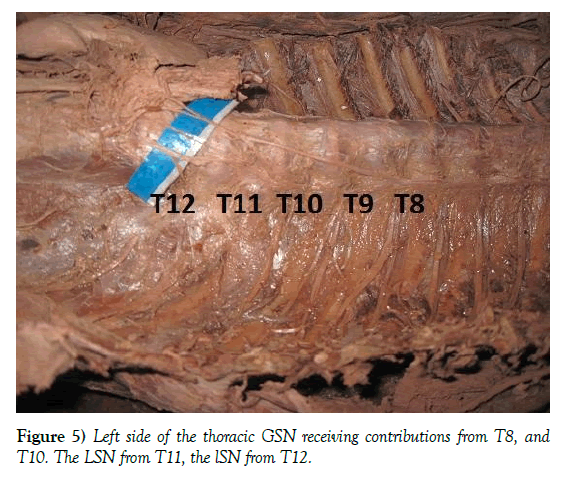
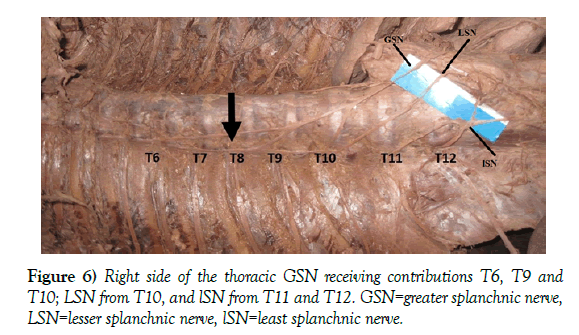
The compositions of ganglionic arrays that contribute to the GSN were arranged from two to seven spinal segments. The most common segments for the contribution of the GSN were 4 segments seen in 7/20 (35%) sides of the cadavers. On the right side, the most common segments for the contribution of the GSN were 5 segments (Table 5). The most common range of the ganglionic array for GSNs was from T7 to T10 (Table 6). In one (10%) of the cadavers symmetric composition of the ganglia was found for the GSN on either side. Almost all roots of the GSN were consecutive, without missing root. Only one cadaver was attributed by inconsecutive ganglia that were right side arise from ganglia T6, T9, T10 and left side from T8, T10 (Figures 2-6). The ganglionic arrays on the right side were longer than those on the left.
| Number of Roots | Greater splanchnic nerve | Lesser splanchnic nerve | Least splanchnic nerve | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Left(n=10) | Right(n=10) | Total(n=20) | Left(n=10) | Right(n=10) | Total(n=20) | Left(n=10) | Right(n=10) | Total(n=20) | |
| 1 | - | - | - | 90%(9/10) | 50%(5/10) | 70%(14/20) | 70%(7/10) | 70%(7/10) | 70%(14/20) |
| 2 | 20%(2/10) | 10%(1/10) | 15%(3/20) | 10%(1/10) | 40%(4/10) | 25%(5/20) | 30%(3/10) | 30%(3/10) | 30%(6/20) |
| 3 | - | 10%(1/10) | 5%(1/20) | - | 10%(1/10) | 5%(1/20) | - | - | - |
| 4 | 60%(6/10) | 10%(1/10) | 35%(7/20) | - | - | - | - | - | |
| 5 | 10%(1/10) | 40%(4/10) | 25%(5/20) | - | - | - | - | - | - |
| 6 | - | 20%(2/10) | 10%(2/20) | - | - | - | - | - | |
| 7 | 10%(1/10) | 10%(1/10) | 10%(2/20) | - | - | - | - | - | - |
Table 5: Number of Ganglionic array connected to the Thoracic Splanchnic Nerves
| Nerve | Composition | Frequency(n=20) |
|---|---|---|
| Greater splanchnic nerve | T4,T5,T6,T7,T8,T9,T10 | 5%(1/20) |
| T5,T6,T7,T8,T9,T10,T11 | 5%(1/20) | |
| T6,T7,T8,T9,T10,T11 | 10%(2/20) | |
| T6,T7,T8,T9,T10 | 20%(4/20) | |
| T6, T9, T10 | 5%(1/20) | |
| T7,T8,T9,T10,T11 | 5%(1/20) | |
| T7,T8,T9,T10 | 35%(7/20) | |
| T7, T8 | 5%(1/20) | |
| T8, T9 | 5%(1/20 | |
| T8, T10 | 5%(1/20) | |
| Lesser splanchnic nerve | T10, T11, T12 | 5%(1/20) |
| T10, T11 | 10%(2/20) | |
| T10 | 10%(2/20) | |
| T11, T12 | 15%(3/20) | |
| T11 | 45%(9/20) | |
| T12 | 15%(3/20) | |
| Least splanchnic nerve | T11, T12 | 30%(6/20) |
| T12 | 70%(14/20) |
Table 6: Composition of Ganglionic Array Connected to the Thoracic Splanchnic Nerves
Ganglia, which were contributing to the formation of the LSN range from T10-T12. The uppermost sympathetic ganglion, which contribute to the formation of LSN were at the level of T11 in 60% (12/20) sides of the cadavers (Table 2). The lowermost ganglion, rooting for the formation of the LSN was T11 in 11/20 (55%) sides of the cadaver (Table 3). The ganglia with the highest participation rate were at the T11 (Figure 6 and Table 4).
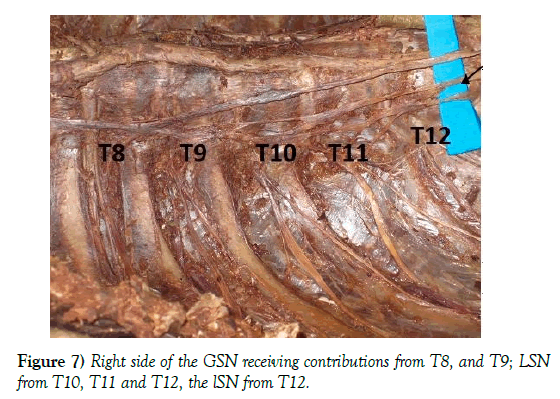
The ganglionic arrays that produced the roots of the LSN were arranged along one to three spinal segment(s). The most common length was by one segment in 14/20 (70%) sides (Figure 7 and Table 5). The most typical LSNs formed by one sympathetic ganglion were at the T11 (Table 6). All roots of the LSN were consecutive, without missing root. The ganglionic arrays on the right were longer than those on the left. Only 2/10 (20%) cadavers with bilateral dissection had symmetric compositions of ganglia to LSNs.
Ganglia at the T11–T12 levels gave branches to the lSNs. In 30% of the total dissected sides, the highest nerve branch to the lSN was from the ganglion at the T11 level (Table 2). The lowest root of the lSN was from the T12 sympathetic ganglion in 14/20 (70%) sides (Table 3). The ganglia at the T12 level contributed to the lSN most frequently (Table 4). The lSN was composed of nerve fibers from one ganglion in 70% of specimens, two ganglia in 30% of specimens (Figure 4 and Table 5). The most typical single form of the lSN had roots from the T12 thoracic sympathetic ganglia in 70% of the specimens (Table 6). About 60% of the cadavers with bilateral dissection had symmetric lSNs. There was no absence of lSNs detected on both sides.
Discussion
Thoracic splanchnicectomy is an important surgical procedure for the relief of pain caused by chronic pancreatitis, cancer of the pancreas or other organs in the region [2,4,22]. Splanchnicectomies and other surgical procedures are dependent on the detailed knowledge of the anatomy of these nerves and their variations [2]. The inconsistent results after the procedure could be due the medial collateral branches which provide alternate pathway to upper sympathetic chain and the anatomical variations found in the TSNs [4].
In most of the previous studies, GSN was found in 100% of the dissections, whereas the incidence of the LSN and lSN variable [2,4,5]. In the current study, the GSN, LSN, and lSN were found in 100% of the cadavers. Naidoo et al. reported 100% presence of GSN, but 92% for LSN and 55% for lSN [7]. Gest also reported the presence of the greater and lesser thoracic splanchnic nerves in all sides [2]. The highest level of origin was seen from T4 and the lowest ganglia contributing to the formation of the GSN was T11. This is similar with other studies in India and Korea [4,20,22,23]. Jacob et al. Dayal et al. and Naidoo et al. reported a higher origin of GSN at T3 level [1,5,7].
The current study found that the compositions of ganglionic arrays that contribute to the GSN were arranged from two to seven spinal segments and this was found similar to the study in Korea [20]. A study in South India re ported that the GSN arise from two to six segments [4]. The most common segments for the contribution of the GSN were 4 segments in 35% of cases. A study on Indian cadavers also showed GSN arose from four roots in 36.36% [5]. A research done in South Africa indicated that the GSN arises from one to four branches, most frequently (73%) from the T6-T9 ganglia [7]. Other research on Korean cadavers confirmed that the GSN was originated most frequently from T5-T9 [20].
A standard text book indicated that the GSN is formed by 5th-9th or 5th-10th thoracic sympathetic ganglia [24,25]. In the current research, the uppermost thoracic sympathetic ganglion connected most frequently to the GSN was at the T7 level followed by T6, and lowermost ganglion most frequently participated in the formation of the GSN was at the T10 level. A research on Indian cadavers showed the highest root of GSN arose frequently from T6 followed by T7 [5]. According to the study of Sakthivel et al. the highest root of origin of GSN was from T6 ganglia in 41.4%, followed by T5 (24.3%), and T7 (21.4%) [4]. A research done in Korea indicated that the uppermost ganglia most frequently participated in the formation of GSN were T5 in 43.5% of the cadavers and lowermost frequent ganglia were T9 in 84.8% [20].
Almost all roots of the GSN were consecutive, without missing root. Only one cadaver was attributed by inconsecutive ganglia that were right side arise from ganglia T6, T9, T10 and left side from T8, T10; having missing ganglia T7 and T8 on the right and T9 on the left side. Similarly, a research done on Korean cadavers indicated that the arrangement of ganglia connected to the GSN is not consecutive in 54.3% of the cadavers [20]. Naidoo et al indicated that in one of their specimen the GSN origin from T7-T8 which has similarity with one of our cadaver [7].
Ganglia, which were contributing to the formation of the LSN range from T10-T12. A study by Thangaraj et al. showed that the roots of the LSN were found to be contributed from T8-T11 ganglion [21]. The uppermost sympathetic ganglion which contributed to the formation of LSN was at the level of T11 in 60% of the cadavers. A study in India indicated that the highest roots of origin of the LSN were at T11 in 34.52% followed by T10 in 25.0% [5]. A research done by Yang et al. indicated the upper most sympathetic ganglion, which contributed to the LSN, was at the T10 level in 58.7% of specimens [20].
The lower most ganglion which gave branches to the LSN was T11 in 55% of the specimens. In a study of Dayal et al. the lowermost root of origin was T12 in all other cases [5]. The ganglionic arrays that produced the roots of the LSN were arranged along one to three spinal segment(s) in current study. The most common length was by one segment. A study in Korea indicated that the ganglionic arrays that produced the roots of the LSN were arranged along one to five spinal segment(s). The most common length was by two segments [20]. The most typical single LSN was formed by sympathetic ganglia at the T11 level. The most typical LSN was formed by two sympathetic ganglia at the T10 and T11 levels according to a study in Korea [20]. In right side of one of the cadavers the LSN origin from T10, T11, T12, while the GSN arise from T8, T9 ganglia. Mitchel in 1935 argued that the splanchnic nerves should be named for their level of origin and not their size, thus removing the greater, lesser and least splanchnic nerves and replace by superior, middle and inferior [26]. This holds some truth when we compare with the above findings and some of the figures.
A study on South African cadavers reported the presence of the lSN in 55% of the cases, with an origin from T11 and T12 [7]. In the present research, lSN was present in all cases with origin range from T11-T12 which was similar to the above literature.
The current research provided the first insight on the anatomical variations of TSNs in Ethiopia. The main limitation of this study was unable to get more specimens. In addition, the relationship of TSNs with each other and their course through the diaphragm was not studied. Further study is recommended for the course of the TSNs through the diaphragm in increased number of subjects and magnifying equipment. Beyond the above limitations, the detailed anatomical information provided in this report will be a baseline for Ethiopian surgeons and anesthesiologist in the successful completion of splanchnicectomies.
Conclusion
The GSN, LSN, and lSN were prevalent in all of the specimens. The most common origin of the GSN was T7, T8, T9, and T10. T11 and T12 were the most ganglionic origin of LSN and lSN respectively. The compositions of ganglionic arrays that contribute to the GSNs were arranged from two to seven spinal segments. The ganglia that participate in the formation of LSNs were arranged from one to three segments, and lSNs were arranged from one to two spinal segments. The pattern of the formation and structure of the TSNs was not only varying from person to person but also between the right and left side.
Acknowledgement
The authors would like to extend their appreciation to Professor Dieter Reissig who has helped authors a lot starting from courage to choose and do with this title and giving additional advice. Also, want to express great thanks to Mekelle university Anatomy department Dr. Hayelom Kebede for his suggestion and allow us to collect data from the Department of Anatomy.
REFERENCES
- Jacob TG, Wadhwa S, Paul S, et al. Variations of thoracic splanchnic nerves and its clinical implications. Int J Morphol. 2005;23:247-51.
- Gest TR, Hildebrandt S. The pattern of the thoracic splanchnic nerves as they pass through the diaphragm. Clinical Anatomy. 2009;22:809-14.
- Haroun HS. Clinical anatomy of the splanchnic nerves. MOJ Anat & Physiol. 2018;5:88-91.
- Sakthivel S, Manjunath K. Variant anatomy of greater splanchnic nerve. National J Basic Med Sci. 2016;7:77-82.
- Dayal SS, Manjunath KY. Variations in the formation of thoracic splanchnic nerves. Eur J Anat. 2014;18:141-51.
- Erdine S. Celiac ganglion block. Agri. 2005;17:14-22.
- Naidoo N, Partab P, Pather N, et al. Thoracic splanchnic nerves: implications for splanchnic denervation. J Anat. 2001;199:585-90.
- Loukas M, Klaassen Z, Merbs W, et al. A review of the thoracic splanchnic nerves and celiac ganglia. Clinical Anatomy. 2010;23:512-22.
- Hajjar Na, Mois E, Graur F, et al. Thoracoscopic splanchnicectomy. Advanced Laparoscopy. 2016.
- Ehrhardt JD, Lopez-Ojeda W. Anatomy, Thorax, Nerves, Greater Splanchnic: StatPearls [Internet]; 2018.
- Khelif K, Scaillon M, Govaerts MJM, et al. Bilateral thoracoscopic splanchnicectomy in chronic intestinal pseudo-obstruction: report of two pediatric cases. Gut. 2006;55:293-4.
- Lang-Lazdunski L, Pimpec-Barthes F, Riquet M. Videothoracoscopic splanchnicectomy for intractable pain from adrenal metastasis. Ann Thorac Surg. 2002;73:1290-2.
- Leksowski K. Thoracoscopic splanchnicectomy for the relief of pain due to chronic pancreatitis. Surg Endosc. 2001;15:592-6.
- Makarewicz W, Stefaniak T, Kossakowska M, et al. Quality of life improvement after videothoracoscopic splanchnicectomy in chronic pancreatitis patients: case control study. World J Surg. 2003;27:906-11.
- Bradley E, Bem J. Nerve blocks and neuroablative surgery for chronic pancreatitis. World J Surg. 2003; 27:1241-8.
- Jit I, Mukerjee R. Observations on the anatomy of the human thoracic sympathetic chain and its branches; with an anatomical assessment of operations for hypertension. J Anat Soc India. 1960;9:55-82.
- Kuntz A. The Autonomic Nervous System. London: Bailliere: Tindall and Cox. 1934.
- Mitchell G. Anatomy of the Autonomic Nervous System. London: Livingstone; 1953.
- Reed A. The origin of the splanchnic nerves. Anat Rec. 1951;109.
- Yang HJ, Gil YC, Lee WJ, et al. Anatomy of thoracic splanchnic nerves for surgical resection. Clin Anat. 2008;21:171-7.
- Thangaraj S, Nagarajan V. Pattern of origin of thoracic splanchnic anatomy section nerves and their clinical implications for sympathectomy and splanchnicectomy-a detailed cadaveric study. Inter J Anat Radiol Sur. 2018;7:14-9.
- Jothi SS, Hemanth K, Kumar UR, et al. Greater splanchnic nerve. Inter J Anat Sci. 2010;1:17-20.
- Kommuru H, Jothi S, Bapuji P, et al. Thoracic part of sympathetic chain and its branching pattern variations in South Indian cadavers. J Clin Diagnostic Res. 2014;8:AC09-AC12.
- Standring S. Gray’s Anatomy. Churchill Livingstone, New York: Elsevier. 2015.
- Moore KL, Dalley A, Agur AM. Clinically Oriented Anatomy. Canada: Lippincott Williams & Wilkins; 2013.
- Makino K, Yamada TK, Kumaki K. Classification of the abdominal splanchnic nerves -a preliminary attempt to re-evaluate their nomenclatures. Folia Anat. 1991;67:443-4.