Multiple variations along the brachial artery distribution
Ozlem Elvan*, Alev Kara, Nail Can Ozturk
Department of Anatomy, Mersin University Faculty of Medicine, Mersin, Turkey.
- *Corresponding Author:
- Ozlem Elvan
Mersin University, Faculty of Medicine, Department of Anatomy, Yenisehir Campus, 33169, Mersin, Turkey.
Tel: +90 532 7274186
E-mail: ofzt@hotmail.com
Date of Received: June 23rd, 2011
Date of Accepted: October 28th, 2011
Published Online: December 31st, 2011
© IJAV. 2011; 4: 211–213.
[ft_below_content] =>Keywords
brachial artery, superficial brachioulnar artery, common interosseous artery, variation
Introduction
The classical pattern of distribution of upper limb arteries exists in many textbooks. Variations in the arterial patterns of the upper limb have been the subject of many anatomical studies due to their high incidence. These variations are encountered in a broad spectrum such as absence, high origin, locational variations or duplication of the arteries [1].
This report describes a different pattern of brachial artery distribution. These variations might cause serious problems in a wide range of clinical situations. Thus, being aware of every pattern of variation has utmost importance in clinical practice.
Case Report
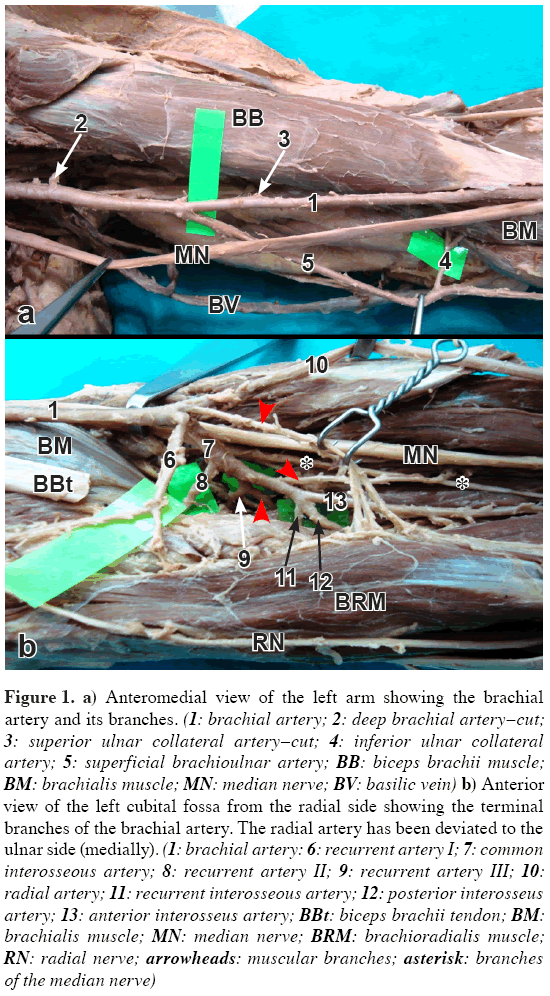
During the dissection of the left upper limb of a 75-year-old male cadaver, some important variations were encountered in the brachial artery (BA) and its branches. The BA gave its deep branch as usual. After running 5.7 cm distally, in the middle of the arm, a superficial brachioulnar artery (SBU) was observed originating from the BA. The BA then gave the superior ulnar collateral branch. The inferior ulnar collateral branch arose from the SBU instead of BA on the origin of the pronator teres which then pierced the brachialis muscle (Figure 1a). This collateral branch divided into two branches after a short course. The SBU passed through the cubital fossa on the origin of the superficial flexors of the forearm and coursed distally on the medial border of the flexor digitorum superficialis. The SBU had no branches at the cubital fossa. It gave two branches at the wrist and terminated by giving its usual branches to complete the superficial and deep palmar arches.
Figure 1: a) Anteromedial view of the left arm showing the brachial artery and its branches. (1: brachial artery; 2: deep brachial artery–cut; 3: superior ulnar collateral artery–cut; 4: inferior ulnar collateral artery; 5: superficial brachioulnar artery; BB: biceps brachii muscle; BM: brachialis muscle; MN: median nerve; BV: basilic vein) b) Anterior view of the left cubital fossa from the radial side showing the terminal branches of the brachial artery. The radial artery has been deviated to the ulnar side (medially). (1: brachial artery: 6: recurrent artery I; 7: common interosseous artery; 8: recurrent artery II; 9: recurrent artery III; 10: radial artery; 11: recurrent interosseous artery; 12: posterior interosseus artery; 13: anterior interosseus artery; BBt: biceps brachii tendon; BM: brachialis muscle; MN: median nerve; BRM: brachioradialis muscle; RN: radial nerve; arrowheads: muscular branches; asterisk: branches of the median nerve)
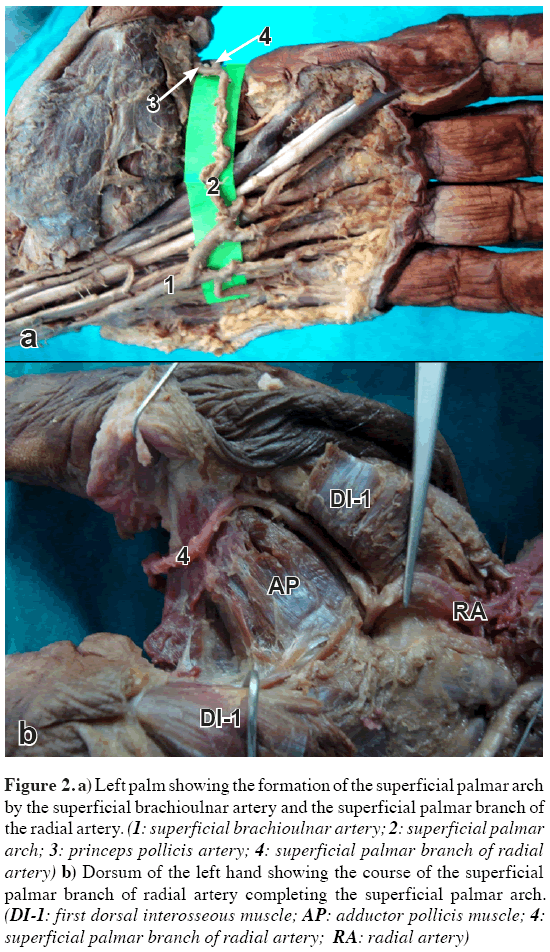
The brachial artery entered the cubital fossa with the median nerve on the brachialis and on the medial margin of the biceps brachii. It then ramified into a radial artery (RA), a common interosseous artery (CIA), a recurrent artery (first recurrent artery –RA1) and a muscular branch at the level of the neck of the radius, at the lateral side of the pronator teres and over the biceps tendon. The RAI arose as a trunk and after a short distance it diverged into an ascending and a descending terminal branch. While the ascending branch supplied the elbow joint, the descending branch supplied the supinator muscle. The RA coursed distally and then diverged into two branches at the point of the basis of the first metacarpal bone on the dorsum of the hand. The superficial palmar branch of the radial artery (SPBRA) joined the superficial palmar arch (SPA) passing through the first web space while the other joined the deep palmar arch (Figure 2a, b). The CIA, during its 3.8 cm course, it gave off a recurrent artery (second recurrent artery – RA2) running to the elbow joint. Two other branches were also observed diverging from the CIA at the cubital fossa. The first one also diverged into two branches; one of which was muscular and the other was another recurrent artery (third recurrent artery – RA3) supplying the elbow joint. The former supplied the superficial flexor digitorum. After giving these muscular branches, the CIA gave off the anterior, posterior and recurrent interosseus arteries (Figure 1b).
Figure 2: a) Left palm showing the formation of the superficial palmar arch by the superficial brachioulnar artery and the superficial palmar branch of the radial artery. (1: superficial brachioulnar artery; 2: superficial palmar arch; 3: princeps pollicis artery; 4: superficial palmar branch of radial artery) b) Dorsum of the left hand showing the course of the superficial palmar branch of radial artery completing the superficial palmar arch. (DI-1: first dorsal interosseous muscle; AP: adductor pollicis muscle; 4: superficial palmar branch of radial artery; RA: radial artery)
Discussion
Arterial variations are common in the upper extremity [1,2]. Superficial brachial, ulnar or radial arteries, superficial brachioulnar or brachioradial arteries, high originating radial or ulnar arteries are some of these variations [1–6]. These branches are observed taking the origin almost 5 times more often from the BA than from the axillary artery and also unilateral variations are more common than bilateral ones [7]. The most frequently reported incidences pertinent to the present case are high origin of the ulnar artery from BA as 1.33% and superficial ulnar artery as 0–9.38% [1,2,8]. Typically when the ulnar artery has a high origin, its course is always superficial to the forearm flexors [5].
A SBU is defined as an ulnar artery originating proximal to the intercondylar line from either the axillary or the BA and coursing over the superficial flexor forearm muscles. Superficial ulnar artery (SUA) with a high origin is a frequently used synonym for this variant, but it is thought not to be an appropriate and clear definition. Rodriguez-Niedenfuhr et al. considered that the term ‘brachio’ is combined with the corresponding region in the forearm (e.g., brachioradial, brachioulnar) for variations that originate in the arm, and the term ‘superficial’ is added depending on whether the latter arteries pursue a normal or superficial course in the forearm [6].
High proximal division into terminal branches is one of the major variations of the BA that mostly occurs in the upper third of the arm and least in the middle third [3,6]. In the study of Rodriguez-Niedenfuhr et al. in 192 cadavers, they reported the incidence of the SBU as 4.2% and they did not find any case where the BA originated from the middle third of the arm [6]. In the present case the SBU originated from the BA in the middle third and lay superficially in its whole course.
Rodriguez-Niedenfuhr et al. reported that when there is a SBU, the BA divides at its normal level into the radial artery and the interosseous trunk, the latter sending off the recurrent ulnar artery [6]. This pattern resembles to the present case. The SBU had no recurrent branches at the cubital region in this case, but three recurrent branches were observed taking origin from the variant arteries which could replace ulnar, radial and interosseous recurrent arteries. While the first of these (RA1) was the branch of BA in the cubital fossa, the second (RA2) and third (RA3) recurrent arteries were the branches of the CIA. In some cases reporting a highly originating SUA, the CIA was diverging from the radial artery [5]. The CIA showed a different pattern of origin in this case by emerging from the BA instead of ulnar. Additional anatomic variations in the upper limb such as persistent median artery or any unusual muscular structures along with these variant arteries as reported by some others did not exist in this case [2].
Two major different forms (complete and incomplete) and their incidences have been reported for the formation of the SPA of the hand in the literature [9]. Bilge et al. found the complete form as 86% and incomplete as 14%. They divided the complete arch into four types. They called type A as a radio-ulnar type in which the arch was formed by the branches of the radial and ulnar arteries and they then divided type A into two subtypes. Subtype I is the classical subtype which was formed by the terminal part of the ulnar artery and SPBRA. This pattern was observed in 17 hands (34%) in their study [4]. The SPA of this study was similar to the subtype I of the above study but differed from it as the SPBRA in this case was from the dorsal branch of the radial artery which was passing through the first web space.
The mechanism of development of arterial variations has been the subject of many studies. According to Rodriguez-Niedenfuhr et al. the upper limb arteries form from an initial capillary plexus that appears from the dorsal aorta and develops at the same rate as the limb. A remodeling process occurs involving the enlargement and differentiation of selected parts. It is thought that variations arise through the persistence, enlargement and differentiation of parts of the initial network which would normally remain as capillaries or even regress [10].
In cases where the SBU replaces the ulnar artery, its accidental injury during surgical procedures can result in serious ischemia of the forearm [2]. It is more vulnerable to trauma but also more accessible for cannulation and carries the risk of potential intra-arterial injection, secondary gangrene and even amputation when it is mistaken for a superficial vein [1,2]. Radiographically, this artery can lead to misinterpretation of incomplete angiographic pictures. Ignorance of this anatomic variation can cause severe impairment of the hand irrigation [1]. As this superficial artery replaced the typical artery and was not an additional vessel it is not convenient to be used for flap. Less critical knowledge of variations of the recurrent elbow arteries might lead to iatrogenic injury during trauma and reconstruction surgery of the elbow.
References
- Jacquemin G, Lemaire V, Medot M, Fissette J. Bilateral case of superficial ulnar artery originating from axillary artery. Surg Radiol Anat. 2001; 23: 139–143.
- Natsis K, Papadopoulou AL, Paraskevas G, Totlis T, Tsikaras P. High origin of a superficial ulnar artery arising from the axillary artery: anatomy, embryology, clinical significance and a review of the literature. Folia Morphol (Warsz). 2006; 65: 400–405.
- Bergman RA, Afifi AK, Miyauchi R. Illustrated Encyclopedia of Human Anatomic Variation: Opus II: Cardiovascular System: Arteries: Upper Limb. http://www.anatomyatlases.org/AnatomicVariants/Cardiovascular/Text/Arteries/Ulnar.shtml (accessed January 5th, 2011)
- Bilge O, Pinar Y, Ozer MA, Govsa F. A morphometric study on the superficial palmar arch of the hand. Surg Radiol Anat. 2006; 28: 343–350.
- Hazlett JW. The superficial ulnar artery with reference to accidental intra-arterial injection. Can Med Assoc J. 1949; 61: 289–293.
- Rodriguez-Niedenfuhr M, Vazquez T, Nearn L, Ferreıra B, Parkin I, Sanudo JR. Variations of the arterial pattern in the upper limb revisited: a morphological and statistical study, with a review of the literature. J Anat. 2001; 199: 547–566.
- Cherukupalli C, Dwivedi A, Dayal R. High bifurcation of brachial artery with acute arterial insufficiency: a case report. Vasc Endovascular Surg. 2007 Dec-2008 Jan; 41: 572–574.
- Nakatani T, Tanaka S, Mizukami S. Superficial ulnar artery originating from the brachial artery and its clinical importance. Surg Radiol Anat. 1998; 20: 383–385.
- Tagil SM, Cicekcibasi AE, Ogun TC, Buyukmumcu M, Salbacak A. Variations and clinical importance of the superficial palmar arch. SDU Tip Fak Derg. 2007; 14: 11–16.
- Rodriguez-Niedenfuhr M, Burton GJ, Deu J, Sanudo JR. Development of the arterial pattern in the upper limb of staged human embryos: normal development and anatomic variations. J Anat. 2001; 199: 407–417.
Ozlem Elvan*, Alev Kara, Nail Can Ozturk
Department of Anatomy, Mersin University Faculty of Medicine, Mersin, Turkey.
- *Corresponding Author:
- Ozlem Elvan
Mersin University, Faculty of Medicine, Department of Anatomy, Yenisehir Campus, 33169, Mersin, Turkey.
Tel: +90 532 7274186
E-mail: ofzt@hotmail.com
Date of Received: June 23rd, 2011
Date of Accepted: October 28th, 2011
Published Online: December 31st, 2011
© IJAV. 2011; 4: 211–213.
Abstract
During the left upper limb dissection of a 75-year-old male cadaver variations were encountered in the brachial artery and its branches. A superficial brachioulnar artery arose from the brachial artery in the middle of the arm. The superior and inferior ulnar collateral branches arose from the brachial and superficial brachioulnar arteries, respectively. Then the brachial artery ramified into a radial, common interosseous, recurrent arteries and a muscular branch at the level of the neck of radius. The common interosseous artery first gave off a recurrent artery and then a trunk which ramified into another recurrent artery and a muscular branch and finally terminated giving anterior, posterior and recurrent interosseous arteries. The superficial palmar branch of the radial artery coursed on dorsum of the hand and by passing through the first web space joined the superficial palmar arch. Additional variations were observed during the courses of the branches of these arteries.
-Keywords
brachial artery, superficial brachioulnar artery, common interosseous artery, variation
Introduction
The classical pattern of distribution of upper limb arteries exists in many textbooks. Variations in the arterial patterns of the upper limb have been the subject of many anatomical studies due to their high incidence. These variations are encountered in a broad spectrum such as absence, high origin, locational variations or duplication of the arteries [1].
This report describes a different pattern of brachial artery distribution. These variations might cause serious problems in a wide range of clinical situations. Thus, being aware of every pattern of variation has utmost importance in clinical practice.
Case Report
During the dissection of the left upper limb of a 75-year-old male cadaver, some important variations were encountered in the brachial artery (BA) and its branches. The BA gave its deep branch as usual. After running 5.7 cm distally, in the middle of the arm, a superficial brachioulnar artery (SBU) was observed originating from the BA. The BA then gave the superior ulnar collateral branch. The inferior ulnar collateral branch arose from the SBU instead of BA on the origin of the pronator teres which then pierced the brachialis muscle (Figure 1a). This collateral branch divided into two branches after a short course. The SBU passed through the cubital fossa on the origin of the superficial flexors of the forearm and coursed distally on the medial border of the flexor digitorum superficialis. The SBU had no branches at the cubital fossa. It gave two branches at the wrist and terminated by giving its usual branches to complete the superficial and deep palmar arches.
Figure 1: a) Anteromedial view of the left arm showing the brachial artery and its branches. (1: brachial artery; 2: deep brachial artery–cut; 3: superior ulnar collateral artery–cut; 4: inferior ulnar collateral artery; 5: superficial brachioulnar artery; BB: biceps brachii muscle; BM: brachialis muscle; MN: median nerve; BV: basilic vein) b) Anterior view of the left cubital fossa from the radial side showing the terminal branches of the brachial artery. The radial artery has been deviated to the ulnar side (medially). (1: brachial artery: 6: recurrent artery I; 7: common interosseous artery; 8: recurrent artery II; 9: recurrent artery III; 10: radial artery; 11: recurrent interosseous artery; 12: posterior interosseus artery; 13: anterior interosseus artery; BBt: biceps brachii tendon; BM: brachialis muscle; MN: median nerve; BRM: brachioradialis muscle; RN: radial nerve; arrowheads: muscular branches; asterisk: branches of the median nerve)
The brachial artery entered the cubital fossa with the median nerve on the brachialis and on the medial margin of the biceps brachii. It then ramified into a radial artery (RA), a common interosseous artery (CIA), a recurrent artery (first recurrent artery –RA1) and a muscular branch at the level of the neck of the radius, at the lateral side of the pronator teres and over the biceps tendon. The RAI arose as a trunk and after a short distance it diverged into an ascending and a descending terminal branch. While the ascending branch supplied the elbow joint, the descending branch supplied the supinator muscle. The RA coursed distally and then diverged into two branches at the point of the basis of the first metacarpal bone on the dorsum of the hand. The superficial palmar branch of the radial artery (SPBRA) joined the superficial palmar arch (SPA) passing through the first web space while the other joined the deep palmar arch (Figure 2a, b). The CIA, during its 3.8 cm course, it gave off a recurrent artery (second recurrent artery – RA2) running to the elbow joint. Two other branches were also observed diverging from the CIA at the cubital fossa. The first one also diverged into two branches; one of which was muscular and the other was another recurrent artery (third recurrent artery – RA3) supplying the elbow joint. The former supplied the superficial flexor digitorum. After giving these muscular branches, the CIA gave off the anterior, posterior and recurrent interosseus arteries (Figure 1b).
Figure 2: a) Left palm showing the formation of the superficial palmar arch by the superficial brachioulnar artery and the superficial palmar branch of the radial artery. (1: superficial brachioulnar artery; 2: superficial palmar arch; 3: princeps pollicis artery; 4: superficial palmar branch of radial artery) b) Dorsum of the left hand showing the course of the superficial palmar branch of radial artery completing the superficial palmar arch. (DI-1: first dorsal interosseous muscle; AP: adductor pollicis muscle; 4: superficial palmar branch of radial artery; RA: radial artery)
Discussion
Arterial variations are common in the upper extremity [1,2]. Superficial brachial, ulnar or radial arteries, superficial brachioulnar or brachioradial arteries, high originating radial or ulnar arteries are some of these variations [1–6]. These branches are observed taking the origin almost 5 times more often from the BA than from the axillary artery and also unilateral variations are more common than bilateral ones [7]. The most frequently reported incidences pertinent to the present case are high origin of the ulnar artery from BA as 1.33% and superficial ulnar artery as 0–9.38% [1,2,8]. Typically when the ulnar artery has a high origin, its course is always superficial to the forearm flexors [5].
A SBU is defined as an ulnar artery originating proximal to the intercondylar line from either the axillary or the BA and coursing over the superficial flexor forearm muscles. Superficial ulnar artery (SUA) with a high origin is a frequently used synonym for this variant, but it is thought not to be an appropriate and clear definition. Rodriguez-Niedenfuhr et al. considered that the term ‘brachio’ is combined with the corresponding region in the forearm (e.g., brachioradial, brachioulnar) for variations that originate in the arm, and the term ‘superficial’ is added depending on whether the latter arteries pursue a normal or superficial course in the forearm [6].
High proximal division into terminal branches is one of the major variations of the BA that mostly occurs in the upper third of the arm and least in the middle third [3,6]. In the study of Rodriguez-Niedenfuhr et al. in 192 cadavers, they reported the incidence of the SBU as 4.2% and they did not find any case where the BA originated from the middle third of the arm [6]. In the present case the SBU originated from the BA in the middle third and lay superficially in its whole course.
Rodriguez-Niedenfuhr et al. reported that when there is a SBU, the BA divides at its normal level into the radial artery and the interosseous trunk, the latter sending off the recurrent ulnar artery [6]. This pattern resembles to the present case. The SBU had no recurrent branches at the cubital region in this case, but three recurrent branches were observed taking origin from the variant arteries which could replace ulnar, radial and interosseous recurrent arteries. While the first of these (RA1) was the branch of BA in the cubital fossa, the second (RA2) and third (RA3) recurrent arteries were the branches of the CIA. In some cases reporting a highly originating SUA, the CIA was diverging from the radial artery [5]. The CIA showed a different pattern of origin in this case by emerging from the BA instead of ulnar. Additional anatomic variations in the upper limb such as persistent median artery or any unusual muscular structures along with these variant arteries as reported by some others did not exist in this case [2].
Two major different forms (complete and incomplete) and their incidences have been reported for the formation of the SPA of the hand in the literature [9]. Bilge et al. found the complete form as 86% and incomplete as 14%. They divided the complete arch into four types. They called type A as a radio-ulnar type in which the arch was formed by the branches of the radial and ulnar arteries and they then divided type A into two subtypes. Subtype I is the classical subtype which was formed by the terminal part of the ulnar artery and SPBRA. This pattern was observed in 17 hands (34%) in their study [4]. The SPA of this study was similar to the subtype I of the above study but differed from it as the SPBRA in this case was from the dorsal branch of the radial artery which was passing through the first web space.
The mechanism of development of arterial variations has been the subject of many studies. According to Rodriguez-Niedenfuhr et al. the upper limb arteries form from an initial capillary plexus that appears from the dorsal aorta and develops at the same rate as the limb. A remodeling process occurs involving the enlargement and differentiation of selected parts. It is thought that variations arise through the persistence, enlargement and differentiation of parts of the initial network which would normally remain as capillaries or even regress [10].
In cases where the SBU replaces the ulnar artery, its accidental injury during surgical procedures can result in serious ischemia of the forearm [2]. It is more vulnerable to trauma but also more accessible for cannulation and carries the risk of potential intra-arterial injection, secondary gangrene and even amputation when it is mistaken for a superficial vein [1,2]. Radiographically, this artery can lead to misinterpretation of incomplete angiographic pictures. Ignorance of this anatomic variation can cause severe impairment of the hand irrigation [1]. As this superficial artery replaced the typical artery and was not an additional vessel it is not convenient to be used for flap. Less critical knowledge of variations of the recurrent elbow arteries might lead to iatrogenic injury during trauma and reconstruction surgery of the elbow.
References
- Jacquemin G, Lemaire V, Medot M, Fissette J. Bilateral case of superficial ulnar artery originating from axillary artery. Surg Radiol Anat. 2001; 23: 139–143.
- Natsis K, Papadopoulou AL, Paraskevas G, Totlis T, Tsikaras P. High origin of a superficial ulnar artery arising from the axillary artery: anatomy, embryology, clinical significance and a review of the literature. Folia Morphol (Warsz). 2006; 65: 400–405.
- Bergman RA, Afifi AK, Miyauchi R. Illustrated Encyclopedia of Human Anatomic Variation: Opus II: Cardiovascular System: Arteries: Upper Limb. http://www.anatomyatlases.org/AnatomicVariants/Cardiovascular/Text/Arteries/Ulnar.shtml (accessed January 5th, 2011)
- Bilge O, Pinar Y, Ozer MA, Govsa F. A morphometric study on the superficial palmar arch of the hand. Surg Radiol Anat. 2006; 28: 343–350.
- Hazlett JW. The superficial ulnar artery with reference to accidental intra-arterial injection. Can Med Assoc J. 1949; 61: 289–293.
- Rodriguez-Niedenfuhr M, Vazquez T, Nearn L, Ferreıra B, Parkin I, Sanudo JR. Variations of the arterial pattern in the upper limb revisited: a morphological and statistical study, with a review of the literature. J Anat. 2001; 199: 547–566.
- Cherukupalli C, Dwivedi A, Dayal R. High bifurcation of brachial artery with acute arterial insufficiency: a case report. Vasc Endovascular Surg. 2007 Dec-2008 Jan; 41: 572–574.
- Nakatani T, Tanaka S, Mizukami S. Superficial ulnar artery originating from the brachial artery and its clinical importance. Surg Radiol Anat. 1998; 20: 383–385.
- Tagil SM, Cicekcibasi AE, Ogun TC, Buyukmumcu M, Salbacak A. Variations and clinical importance of the superficial palmar arch. SDU Tip Fak Derg. 2007; 14: 11–16.
- Rodriguez-Niedenfuhr M, Burton GJ, Deu J, Sanudo JR. Development of the arterial pattern in the upper limb of staged human embryos: normal development and anatomic variations. J Anat. 2001; 199: 407–417.