Myelolipoma of the adrenal gland: A review and update of the literature
Received: 10-Sep-2018 Accepted Date: Oct 01, 2018; Published: 15-Oct-2018
Citation: Anthony Kodzo-Grey Venyo. Myelolipoma of the adrenal gland: A review and update of the literature. Pulsus J Surg Res. 2018;2(2):50-63.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Myelolipomas of the Adrenal Gland (MLOAs) are un-common benign tumors that tend to be found in the adrenal gland but occasionally foci of MLOAs could be found in other extra-adrenal sites. MLOAs consist of mature adipocytes and normal haematopoietic tissue and may contain precursors of red blood and white blood cells including megakaryocytes. MLOAs were previously most commonly diagnosed at autopsy and as incidentalomas at laparotomies for other conditions. MLOAS tend to be more common in the right adrenal gland. MLOAs may be asymptomatic, or in some cases they may present with loin pain, abdominal pain, nausea and vomiting which are non-specific and larger MLOAs may be associated with sudden hemorrhage requiring emergency admission. Radiological imaging with ultrasound scan, CT scan and MRI scan of abdomen are means by which MLOAs con be identified. The adrenal lesions may be hypo-echogenic, mixed-echogenic or hyper-echogenic and at times with foci of calcification. CT scan evidence of fat density component of the adrenal lesion tends to be diagnostic of MLOA but diagnosis can be confirmed by histopathological examination of radiological imaging of mature adipocytes admixed with myeloid/haematopoietic elements. Even though MLOAs tend to be non-functional by themselves; nevertheless, they tend on 10% of occasions to be associated with endocrine disorders some of which include Cushing syndrome, congenital adrenal hyperplasia, primary hyperaldosteronism (Coon syndrome). And for this reason serum cortisol, metanephrine, normetanephrine and vanillylmandelic levels form part of the routine investigation. Treatment options for MLOAS include: conservative/expectant management foe small lesions. Active/surgical treatment for (a) small MLOAs that are increasing in siz on subsequent radiological imaging, (b) Symptomatic MLOAs, MLOAs that are 6 cm or larger, (d) MLOAs associated with hemorrhage, (e) in situations when malignancy cannot be excluded. Various types of active treatment available include: Laparoscopic adrenalectomy (excision of the whole adrenal gland); Laparoscopic excision oftumor(partial-adrenalectomy), leaving intact the normal looking adrenal gland; Laparotomy and open adrenalectomy (excision of the whole adrenal gland); Laparotomy and open excision oftumor(partial-adrenalectomy), leaving intact the normal looking adrenal gland; Selective angiography and super-selective embolization of feeding artery to the MLOA. Considering the fact that MLOAs tend to be benign generally they should be managed in such a way as to minimize morbidity and if the diagnosis is established radiologically and the options of management should include: conservative approach; partial adrenalectomy, or selective angiography and super-selective embolization of the MLOA. The outcome of MLOAs following all the treatment options tends to be good. Total adrenalectomy could be undertaken in cases when malignancy cannot be excluded. The differential diagnosis include: retroperitoneal liposarcoma, fat-containing adreno-cortical carcinoma, teratoma of the adrenal gland, and angiomyolipoma of the kidney.
Keywords
Adrenal myelolipoma; adipocytes; haematopoietic elements; partial adrenalectomy; adrenalectomy; embolization; conservative treatment; metanephrine; normetanephrine; cortisol; hemorrhage
Introduction
Myelolipoma of the adrenal (MLOA) gland is a rare benigntumorof the adrenal gland that contains fat (mature adipocytes) and myeloid elements. Most often myelolipomas of the adrenal (MLOAs) gland tend to be asymptomatic and they tend to be diagnosed incidentally but on rare occasions (MLOA) may be associated with non-specific symptoms. In view of the rarity of MLOA many clinicians could be unfamiliar with regards to its presentation and management. However, as a result of the common use of ultrasound scan abdomen, Computed-Tomography (CT) scan and Magnetic Resonance Imaging (MRI) scan of abdomen in the investigation of various conditions and symptoms, cases of MLOA are being diagnosed more frequently these days in comparison with earlier days when most often MLOAS were being diagnosed incidentally during autopsy or laparotomy procedures undertaken for various reasons. Adrenal lesions could either be benign or malignant. It may not always be easy or straightforward to confidently diagnose myelolipoma of the adrenal gland based upon the radiological imaging features of the lesion. Because generally myelolipomas of the adrenal gland tend to be diagnosed sporadically, perhaps many clinicians may be unfamiliar with the diagnostic features as well as the biological behaviour of the lesion. Furthermore documentations of myelolipoma of the adrenal gland tend to involve case reports. The ensuing extensive paper which has reviewed the literature on MLOA is divided into two parts: (A) Overview and (B) Miscellaneous narrations and discussions from a number of reported cases of MLOA.
Results
Overview
Definition and general comments
• MLOA is a benigntumorof the adrenal gland which most commonly tends to be a unilateral adrenaltumorwhich is comprised of haematopoietic precursor cells as well as mature fat [1]
• MLOAs most commonly tend to be diagnosed incidentally following autopsy examinations as well as following computed tomography (CT) scans and or magnetic resonance imaging (MRI) scans undertaken in the investigation of non-related conditions [1]
• MLOAs tend not to be functional and they tend not to be associated with haematological dis-orders [1]
Epidemiology
• It has been stated that MLOAs tend to be diagnosed in people who have been within the 5th and 7th decades of their lives and also that MLOAs does not tend to have predilection for any of the sexes [1]
• MLOAs are rare tumors of the adrenal gland that have an autopsy prevalence of 0.1% to 0.2% which tend to be identified in adults as incidental findings or following presentation with hemorrhage [2]
Aetiology: It had been postulated that MLOA could be a result of metaplastic change within the reticuloendothelial cells as a response to stimulation from necrosis, infection or stress [1,3].
Presentation: MLOA was first described by Gierke [4] but Oberling in 1927 coined the name Myelolipoma for the lesion [5]. And since then a number of cases have been reported that had been diagnosed pursuant to a variety of presentations.
Some of the summations relating to the presentation of cases of MLOA include the ensuing:
• Majority of cases of MLOA tend to be asymptomatic [2,4,6] and the findings are made when the affected individuals have undergone radiological imaging for unrelated reasons which would indicate that majority of the lesions would tend to be incidentalomas but larger MLOAs with particular mention of myelolipomas larger than 4 cm can manifest with retroperitoneal hemorrhage of acute onset and furthermore other individuals with particular mention of individuals who have very large myelolipoma lesions tend to manifest with vague mass related symptoms [2,6]
• With regard to site of involvement, it had been stated that MLOA would tend to have a predilection to involve the right adrenal gland [2,7]
• It had been stated that on the whole, MLOA most commonly tends to be non-functional; nevertheless, 10% of MLOAs have been associated with some endocrine disorders including Cushing Syndrome; Congenital adrenal hypoplasia with 21-hydroxylase deficiency, Conn syndrome due to primary aldosteronism and hence individuals who have myelolipomas associated with any of the aforementioned disorders could present with symptoms related to the disorder [2,6]
Clinical examination findings: Generally general and clinical examination of patients with may not reveal any findings that would be diagnostic of MLOA.
Laboratory investigations: On the whole there are no specific laboratory tests including haematology and biochemistry and microbiology tests that would be diagnostic of MLOA but in few cases of MLOAs that may be associated with any endocrine disorder, there could be laboratory test results that may be indicative of the specific endocrine disorder but these would not be diagnostic of MLOA.
Radiological investigation findings, Ultrasound scan: Ultrasound scan of abdomen undertaken for asymptomatic or symptomatic patients may reveal variable findings in the adrenal gland of an individual who has MLOA but these tend to be non-specific but the ultrasound scan feature of a specific myelolipoma tends to depend upon the individual components of the lesion [8]. But on the whole MLOA on ultrasound scanning tends to be seen as heterogeneous adrenal mass of mixed hyper-echogenic and hypo-echogenic components with the hyper-echogenic component resulting mainly from the fatty component of the adrenal lesion [2].
The ultrasound scan findings in MLOA tend to be variable depending upon the individual components of the tumor. The masses tend to be well circumscribed; nevertheless, they generally tend to be seen as heterogeneous masses or mixed hyper-echoic and hypo-echoic components with the hyper-echoic component resulting from the fatty parts of the tumor [2]. It had also been said that ultrasound-scan in cases of MLOA may show a hypo-echoic well encapsulated mass within the adrenal gland [9] or the scan could show lesions with other types of echogenicity like mixed-echogenic areas in the adrenal gland [10].
Ultrasound guided biopsy/aspiration cytology: Ultrasound scan can be used as a guide for the localization of the adrenal lesion which could be biopsied / aspirated for histopathological examination to establish the diagnosis of MLOA.
Computed tomography (CT) scan: Documented summations related to the computed tomography scan findings of MLOA:
• An adrenal mass which has fat components; the mass tends to be relatively well circumscribed, nevertheless, it has been pointed out that adrenal masses which mostly contain fat could prove difficult to separate from the retroperitoneal fat [2]
• The composition of the fat component of MLOA has tended to vary between only a few small regions within an otherwise soft tissue density mass of 10% to adrenal masses that comprise of about equal densities of fat and soft tissue components of about 50% each, or almost completely comprising of fat (40%) [2,6]. In some situations, the soft tissue component and the fat component of the MLOA could be sufficiently mixed such that they render the mass a density that is similar to fluid [2]
• In 25% to 30% of cases of MLOA CT-scan may show punctate calcifications within the adrenal lesions [2,6,11]
• In cases of MLOA in which there are hemorrhages present within the lesions, regions of higher attenuation tend to be seen in the adrenal lesions on CT scanning and this tends to be more frequently seen in large MLOAs greater than 10 cm [12]
CT-guided aspiration/biopsy of adrenal lesion: CT-scan can be used to localize the adrenal lesion in order to obtain aspiration / biopsy specimen for histological examination that could establish a diagnosis of MLOA.
Magnetic Resonance Imaging (MRI) Scans: Summations relating to the MRI- scan findings in MLOAs include:
• T1: hypodense lesions tend to be found within the adrenal gland in view of the fat contents [2]
• T1FS: This typically tends to exhibit fat suppression [2]
• T2: T2 weighted images tend to show generally intermediate to hyperintense lesions within the adrenal gland; nevertheless, this could at times be variable depending upon the contents especially blood products [2]
• T1 C+ Gadolinium (Gd) tend to show striking enhancement [2,8]
• In and out of phase images: With regard to masses with mixed components, out of phase imaging could show signal loss as the microscopic fat cells usually tend to have little intra-cellular water [2,6,13]
MRI scan guided aspiration / biopsy of adrenal lesion to establish diagnosis: MRI scan can be used to localize the adrenal lesion in order to obtain aspiration/biopsy specimen for histological examination that could establish a diagnosis of MLOA.
Differential diagnosis: Differential diagnosis of MLOA include:
• Retroperitoneal liposarcoma [2]
• Fat containing adrenocortical carcinoma [2]
• Adrenal teratoma which is very rare [1,2]
• Angiomyolipoma of the kidney [1,2]
• Liposarcoma [1]
• Myxofibrosarcoma [1]
• Extramedullary haematopoietic tumors [1]
Macroscopic examination Findings: MLOAs tend to be non-encapsulated adrenal lesions consisting of bright yellow adipose-like tissue which may have haemorrhagic foci that contain marrow-tissue [1].
• The adrenal lesions could be up to 5 kg in weight [1]
Microscopic examination findings: Microscopic examination of specimens of MLOAs, tends to show:
• Islands of haematopoietic cells as well as mature fat [1]
• Microscopic examination of the lesions, tend to reveal normal trilineage haematopoiesis nevertheless, quite often there tends to be evidence of markedly increased megakaryocytes [1]
• Within larger MLOAs, there may be hemorrhage, necrosis, calcifications as well as cysts [1]
• On rare occasions, there may be areas of fibromyxoid degeneration that mimic low-grade fibromyxoid sarcoma [1]
Treatment: Considering the fact that MLOA is a benign condition of the diagnosis is established and the lesion is small and the individual who has myelolipoma is asymptomatic then no treatment would be required.
• If a definite diagnosis cannot be made based upon radiological imaging then radiological imaging guided percutaneous biopsy of the lesion can be undertaken for histological examination to confirm the diagnosis. With regard to large MLOAs or in cases where there has been hemorrhage in the lesion then surgical excision would be undertaken and this tends to be curative
Outcome: The prognosis of MLOA would be considered to be good because it is a benign lesion. Miscellaneous Narrations and Discussions from some reported cases.
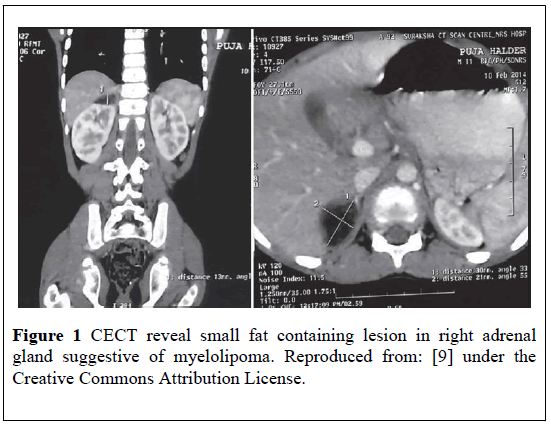
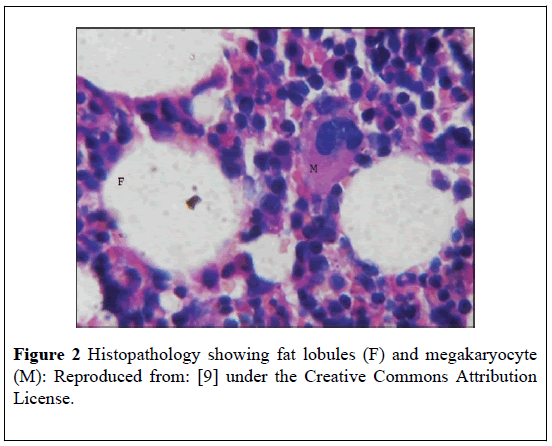
Barman et al. [9] reported an 11-year-old girl who presented with abdominal pain. She had ultrasound-scan and Contrast-Enhanced Computed Tomography (CECT)-scan of the abdomen which showed a well-encapsulated and hypo-echoic lesion within the region of the right adrenal gland that measured (2.71 × 2.43) cm (ultrasound scan finding) which was arising from the right adrenal gland with fat density and that the mass which had calcification in its peripheral part had measured (1.8 × 2.3) cm (Figure 1). The CECT scan also showed that the adrenal gland and the kidney on the left side were normal. She underwent surgical excision of the adrenal mass that measured (2 × 3 × 1) cm. Gross examination of the specimen showed a friable, reddish yellow coloured mass which was soft in consistency. Microscopic examination of the specimen showed islands of haematopoietic scattered among fat cells (Figure 2). It would be argued that fine needle aspiration of the adrenal lesion could have been undertaken for histology confirmation of the diagnosis but fine needle aspiration would not take away the pain of the patient. Excision of the adrenal mass achieved symptomatic relief in the patient.
Figure 1: CECT reveal small fat containing lesion in right adrenal gland suggestive of myelolipoma. Reproduced from: [9] under the Creative Commons Attribution License.
Figure 2: Histopathology showing fat lobules (F) and megakaryocyte (M): Reproduced from: [9] under the Creative Commons Attribution License.
Merchant et al. [14] reported a 20-year-old woman with hypertension and diabetes, who had presented with nausea and flank pain. Her routine haematological and biochemistry tests, urinalysis, urinary vanillylmandelic acid and cathecolamines were normal. She had a CTscan of abdomen which showed a solid left adrenal mass. She underwent open excision of a large left adrenal mass. She was well with no recurrent 9 months later. The tumor was solid, well-circumscribed and had expanded the medulla of the adrenal gland. There was residual adrenal gland at one pole of the tumor as a thin rim which was compressed by the periphery of the tumor.
The surface of the tumors was grey-white, firm and had a 1.5 cm, redbrown soft area at one edge. Microscopic examination of the specimen showed that the tumor had been sharply circumscribed, and it had consisted of interlacing bundles of neurofibromatous tissue which had mature ganglion cells scattered throughout. Within the tumor a number of foci which on gross examination was the red-brown area on microscopic examination were observed to comprise of mature adipose tissue which had been admixed with hematopoietic tissue. These foci were located within the peripheral portions of the tumor. Strands of adrenal cortical cells, mostly of the reticularis type, were identified mingled with the neuro-fibromatous tissue and some of these were observed to be in close proximity to the myelolipomatous foci. This case does show the following:
• That myelolipoma of the adrenal gland could occur in a young female and it could present with flank pain and nausea which are non-specific
• The results of haematology and biochemistry tests could be normal in myelolipoma of the adrenal gland
• Radiology imaging using CT scan of abdomen does show a mass in the adrenal gland but histology examination of the adrenal mass is the best way to confirm diagnosis of myelolipoma of the adrenal gland
Mathews et al. [15] reported a 66-year-old woman who presented with abdominal fullness. She had a CT scan which showed a well-demarcated, low-density, non-enhancing mass with focal calcification within her left adrenal gland. Her serum metanephrine and nor-metanephrine were normal. She underwent left adrenalectomy. The adrenal tumor macroscopically was an encapsulated, bosselatedtumorand had a thin, yellow-transparent and glistening capsule covering it and which was not disrupted by the underlying tissue. Upon sectioning of the tumor, the lesion was observed to be a heterogeneoustumorwhich comprised of a prominent rim of yellow-golden adrenocortical tissue that had surrounded red-brown haemorrhagic areas and white-tan necrotic looking areas. The yellow-golden tissue had also extended into and percolated through all areas of the mass. Histological examination of the adrenal nodule demonstrated a predominantly mature adipose tissue without any evidence of lipoblast, or foetal fat formation. The histopathological features of the tumor, was consistent with MLOA. There was no long-term follow-up detail documented in the case report. This case does illustrate that myelolipoma of the adrenal gland could manifest with abdominal fullness only and its diagnosis could be suspected by undertaking radiology imaging including CT scan but definite diagnosis tends to be made through histology examination of the adrenal lesion. Adrenalectomy with excision of the myelolipoma could help in reducing or eradicating the symptoms of the patient.
Ishikawa et al. [16] reported a case of MLOA which had produced retroperitoneal haematoma. A CT-scan of the abdomen undertaken showed a mass within the right adrenal gland with a fat density and irregular vessels on arteriogram. The patient was at the time of the report of their case the youngest patient to be reported among those who had undergone surgical removal of MLOA and thetumordid not have an endocrine activity. This case does illustrate that even though MLOA is rare, it does represent one of the differential diagnoses of retroperitoneal haematoma.
Tulcinsky et al. [17] reported a 53-year old man who during investigation for painless visible haematuria was found to have an adrenal mass. He had selective angiography which revealed vascular malformations associated with the adrenal mass. He underwent successful removal of the adrenal mass which was the 5th case of successful removal of MLOA to be reported. It could be argued that painless visible haematuria is not a usual presentation of adrenal masses and that the finding of an adrenal lesion in this case was an incidental finding which would indicate that MLOAs could be diagnosed incidentally upon radiology imaging as part of the investigation of some unrelated symptom.
Pagana et al. [18] reported the 14th case of MLOA and they stated that the most consistent complaint that is made by individuals who have MLOA is abdominal pain due to hemorrhage within the tumor. Nevertheless, they had identified an association of MLOA with obesity and hypertension. Pagana et al. [18] further more stated the following:
• The use of ultrasound scan CT-scan of the abdomen is useful in the diagnosis of MLOA
• With expanded use of ultras-sound scan and CT scan of abdomen MLOAs would be recognized more frequently
• Definitive diagnosis and treatment are achieved by means of simple excision of the BBMLOA and radical surgery would not be necessary
Based upon this report, clinicians would need to be reminded that MLOA should be considered as a rare possible finding in the investigation of obesity and hypertension.
Ramirez and Misra [19] reported a 28-year-old woman who presented with left loin pain. She had two years earlier presented with left loin pain when she had a CT-scan which showed a non-obstructing calculus in the left kidney and an incidental well circumscribed adenoma in her left adrenal gland that measured (4.70 × 3.77) cm. She did have another CTscan of abdomen 6 months later which showed that the adrenal adenoma had increased in size and also that there was loss of fat plane between the adrenal adenoma, the spleen, and the pancreas. She had a high BMI, Cushingoid features, with moon facies, truncal obesity, striae on her abdominal wall. Additional to routine haematological and biochemistry blood tests she had investigations to exclude phaeochromocytoma which included Serum Normetanephrine, Serum Metanephrine, 24 hour urine Vinyl Mandelic Acid, acid Vinyl mandelic acid/creatinine ratio which were all normal. She had laparotomy and separation of the adrenal mass from the perinephric fat, and the tumor, the adrenal gland, spleen and the tail of the pancreas were excised en bloc. At her two-week follow-up she had recovered from her operation and indicated that her left upper quadrant abdominal pain and flank pain had subsided. Microscopic examination showed that the adrenal mass contained myelolipoma which had comprised of mature fat cells, admixed with haematopoietic elements. Ramirez and Misra [19] stated the following:
• MLOAs have been treated conservatively; nevertheless; however, surgical intervention for symptomatic tumors, growing tumors, or tumors larger than 6 cm should be undertaken in order to minimise the risk of the development of abdominal pain, or life threatening rupture of the MLOA, and hemorrhage. Pursuant to excision of MLOAs, recurrence of MLOA does not tend to occur and recurrence-free, survival rates of up to 12 years have been reported [20]
• Laparoscopic excision of MLOA has been gaining ground; however, laparoscopy approach would not be indicated in the presence of adhesions or in situations when the lesion has been shown to be infiltrating the surrounding structures [21]
• Although the tumor is considered to be benign, surgery plays an important role in the management of symptomatic cases and in lesions that cannot be reliably differentiated or diagnosed and that the management of MLOA should be undertaken on case to case basis [22]
This reported case does show that apart from conservative treatment and laparoscopic surgery for MLOAs which would tend to be associated with less morbidity, open open adrenalectomy or open excision of an MLOA could be indicated as an alternative treatment option under certain circumstances as stated above.
Al Harthi et al. [23] reported two cases of MLOA which had been managed by laparoscopic surgery as follows:
Case 1
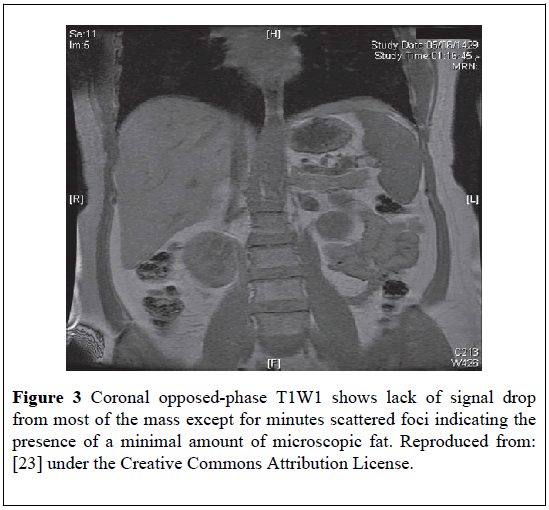
A 53-year-old woman presented with abdominal pain. She had a CT-scan of abdomen which showed a right adrenal mass. The mas contained fat and this raised the possibility of the following: lipoma, fat-rich adrenal adenoma, and liposarcoma. She had multi-planar multi-sequential magnetic resonance imaging (MRI) scan of the adrenal glands and preand post-gadolinum injections. The findings were reported to be consistent with MLOA (Figure 3).
Figure 3: Coronal opposed-phase T1W1 shows lack of signal drop from most of the mass except for minutes scattered foci indicating the presence of a minimal amount of microscopic fat. Reproduced from: [23] under the Creative Commons Attribution License.
Her urinary adrenaline, noradrenaline, dopamine, serum adrenaline, noradrenaline and dopamine, free cortisol, metanephrine and normetanephrine, urinary Vanillyl mandelic acid (VMA) were normal. She had CT-guided aspiration cytology which established the diagnosis of MLOA. She underwent laparoscopic right adrenalectomy and histological confirmed the diagnosis of MLOA. She recovered very well from her operation. This case has confirmed the usefulness of CT scan and MRI scan in the diagnosis of MLOA and the case also has illustrated the usefulness of radiological image-guided aspiration cytology in the confirmation of MLOA.
Case 2
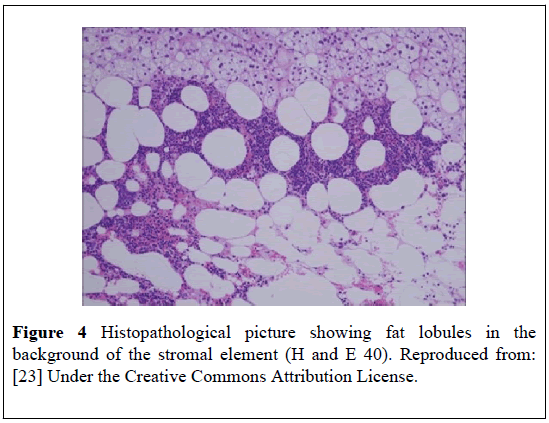
A 43-years-old woman who had hypertension, presented with: right loin pain, palpitation, and increased flushing. She had ultrasound scan of her abdomen which showed a right adrenal mass. Her blood and urine test results showed that she had a non-functioning adrenal mass. She had a Contrast-Enhanced Computed Tomography (CECT) scan of abdomen and MRI-scan with godalinium injection of abdomen which showed a noncontrast enhancing mass in the lateral limb of the right adrenal gland that was consistent with fat. She had CT-guided fine-needle aspiration of the mass and cytology of the specimens showed features of MLOA. She underwent laparoscopic right adrenalectotomyl. Histology of the specimen confirmed MLOA with hematopoiesis (Figure 4).
Figure 4: Histopathological picture showing fat lobules in the background of the stromal element (H and E 40). Reproduced from: [23] Under the Creative Commons Attribution License.
This case has illustrated an association of hypertension and loin pain as well as non-specific symptoms with MLOA. The case has also illustrated the usefulness of ultrasound scan, CT scan and MRI scan as well as FNA in the diagnosis of MLOA. Furthermore, the case has re-affirmed the usefulness of laparoscopic surgery in the excision of MLOA.
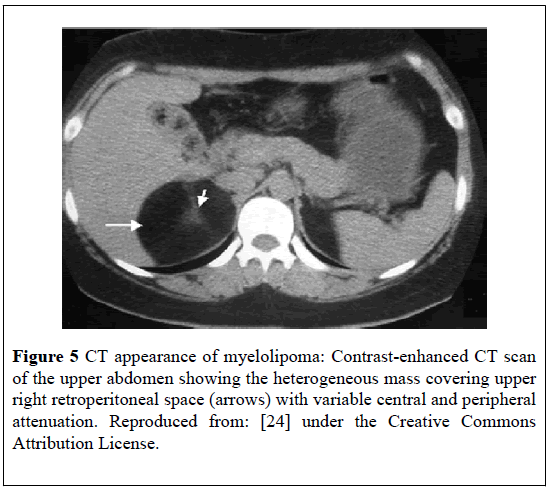
Nabi et al. [24] reported a 63-year-old man who presented with right upper abdominal pain. He had ultrasound scan of the abdomen which showed a hyper-echoic mass in the right adrenal gland which lacked welldefined boundaries and measured (5.9 × 4.5) cm. He had CECT- scan which showed a well-defined, round lesion with central soft tissue attenuation of 38 to 42 HU and with a peripheral attenuation of 52 HU to 65 HU that measured (6.1 × 4.0) cm within the right adrenal gland (Figure 5). The location and attenuation of the mass was consistent with MLOA.
Figure 5: CT appearance of myelolipoma: Contrast-enhanced CT scan of the upper abdomen showing the heterogeneous mass covering upper right retroperitoneal space (arrows) with variable central and peripheral attenuation. Reproduced from: [24] under the Creative Commons Attribution License.
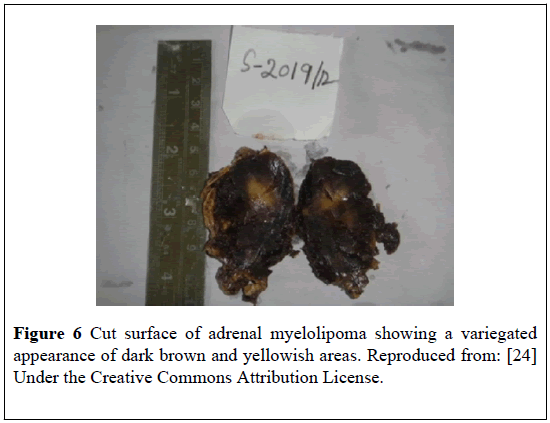
He underwent an open right adrenalectomy. Macroscopic examination of the specimen revealed a large, rounded, and encapsulated mass with smooth external surface that measured (6.5 × 3.5 × 2.6) cm. The cut surface of the specimen showed a solidtumorwith variegated appearance of dark brown and yellowish areas (Figure 6).
Figure 6: Cut surface of adrenal myelolipoma showing a variegated appearance of dark brown and yellowish areas. Reproduced from: [24] Under the Creative Commons Attribution License.
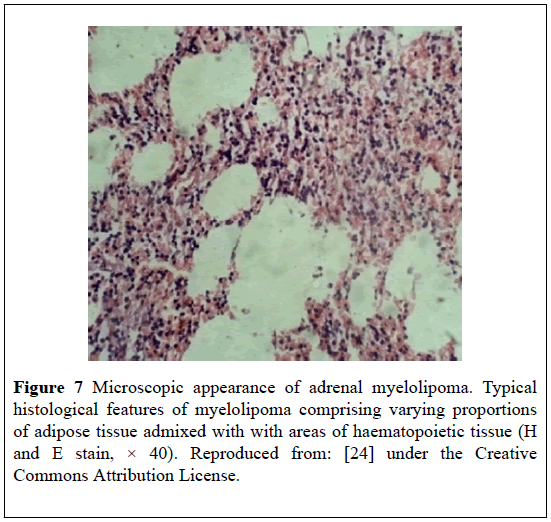
Microscopic examination of the specimen showed characteristic mixture of mature adipose tissue together with haematopoietic elements (Figure 7) lacking signs of atypia, which confirmed the original diagnosis of MLOA.
Figure 7: Microscopic appearance of adrenal myelolipoma. Typical histological features of myelolipoma comprising varying proportions of adipose tissue admixed with with areas of haematopoietic tissue (H and E stain, × 40). Reproduced from: [24] under the Creative Commons Attribution License.
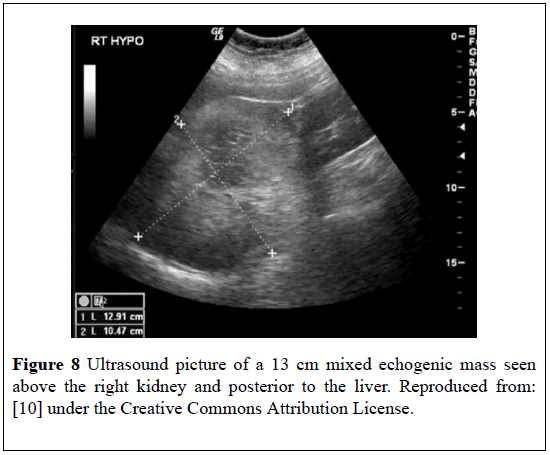
At his 3-months follow-up he was asymptomatic and ultrasound scan of his abdomen did not reveal any recurrence. This case has re-affirmed the usefulness of radiology imaging in the diagnosis and follow-up of MLOA. Doddi et al. [10] reported a 72-year-old woman who presented with dysuria. She had previously undergone complete resection of a moderately dysplastic tubullo-villous adenoma from her colon. She was treated with appropriate antibiotics for Escherichia Coli urinary tract infection. She had ultra-sound scan which showed a mixed echogenic mass that measured 13 cm above the right kidney but posterior to the liver. The mass was welldefined and showed central necrotic changes (Figure 8).
Figure 8: Ultrasound picture of a 13 cm mixed echogenic mass seen above the right kidney and posterior to the liver. Reproduced from: [10] under the Creative Commons Attribution License.
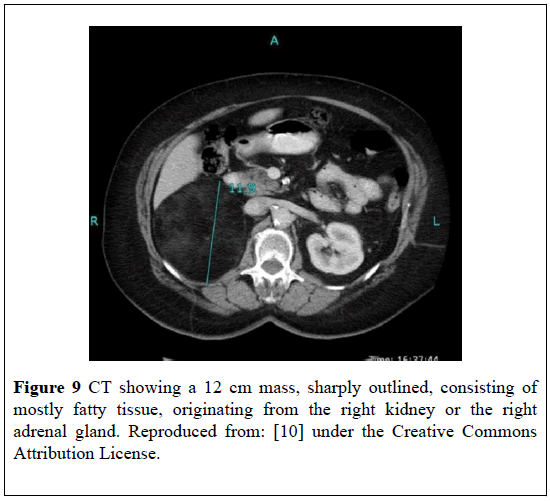
She next had a CT-scan which showed a lesion that measured 12 cm in diameter, was sharply outlined, and mostly comprised of fatty tissue which had originated from the right kidney or right adrenal gland (Figure 9).
Figure 9: CT showing a 12 cm mass, sharply outlined, consisting of mostly fatty tissue, originating from the right kidney or the right adrenal gland. Reproduced from: [10] under the Creative Commons Attribution License.
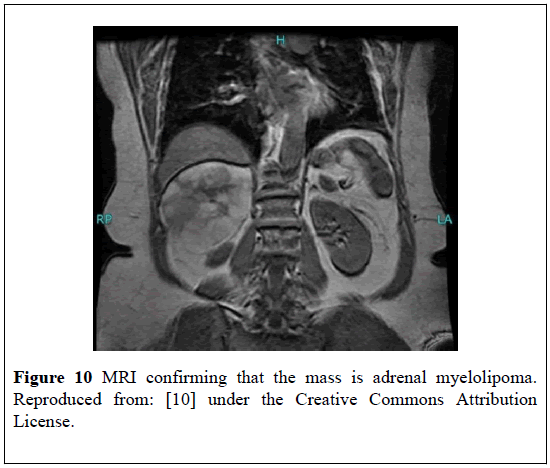
She had MRI- scan which showed the mass was MLOA that measured 11.0 cm in diameter. The mass had a high signal on both T1 and T2 weighted images and there appeared to be necrotic areas within the lesion. There was loss of signal in the T1 fat suppressed images which confirmed its fat nature. The mass was not contrast-enhancing (Figure 10).
Figure 10: MRI confirming that the mass is adrenal myelolipoma. Reproduced from: [10] under the Creative Commons Attribution License.
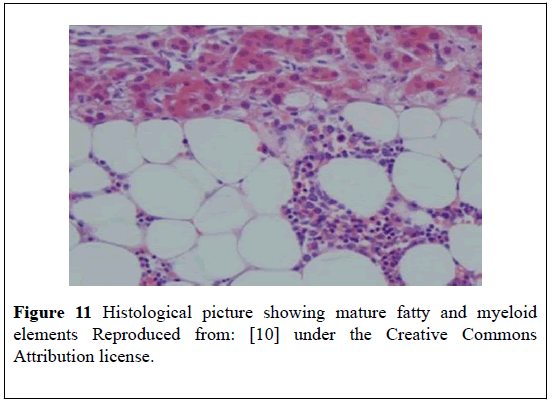
Her routine hematology, blood biochemistry tests, “24- hour urine for cortisol”, noradrenaline, adrenaline and dopamine were normal. She subsequently had a repeat MRI-scan which demonstrated that the adrenal mass had increased in size and that the mass had become more heterogeneous. A malignancy could not be excluded. She underwent an open right adrenalectomy with removal of a 573 grams adrenal mass which had a maximum dimension of 14.5 cm (Figure 11). Histological examination of the specimen showed the lesion was MLOA without any evidence of malignancy.
Figure 11: Histological picture showing mature fatty and myeloid elements Reproduced from: [10] under the Creative Commons Attribution license.
Doddi et al. [10] stated following:
• There has been an increase in the detection of MLOAs incidentally due to the increasing use of CT-scans and MRI- scans
• Occasionally MLOAs have been associated with endocrine dysfunction and by 2004 25 cases of MLOAs associated with endocrine dysfunction had been reported [25]
• Surgical treatment becomes necessitated when the MLOAs are functional, increase in size or become symptomatic [26]
• MLOAs tended to be found incidentally during autopsy, surgery, or as incidentalomas on radiological imaging for other reasons [25], rarely, patients may present with abdominal pain emanating from (a) hemorrhage which tends to be more likely when the myelolipoma is composed of myeloid tissue, (b) tumor necrosis, (c) or mechanical compression from the bulky tumor. Also rarely MLOAs may present as hematuria or abdominal mass [27].
• Four distinct patterns of MLOAs have been described: isolated MLOA; MLOA with hemorrhage; extra-adrenal myelolipoma; MLOA associated with other adrenal diseases including nonfunctional adenomas of the adrenal gland, or endocrine disorders. MLOA which has been associated with Cushing’s syndrome, Conn’s syndrome, and congenital adrenal hyperplasia which has been due to 21 alpha-hydroxylase or 17 alpha-hydroxylase deficiencies had been reported [28]
• The size of MLOA has varied from a few millimetres to greater than 30 cm; nevertheless, the size of MLOA is rarely more than 5 cm. MLOAs tend to be unilateral majority of times without undergoing malignant transformation [29]. Bi lateral MLOAs do occur in about 10% of cases [30]
This case has illustrated the role of radiology imaging in the follow-up of an initially diagnosed MLOA and if there is evidence of increase in size of the adrenal lesion then operative surgery would be indicated.
Wani et al. [31] reported two cases of MLOA as follows:
Case 1
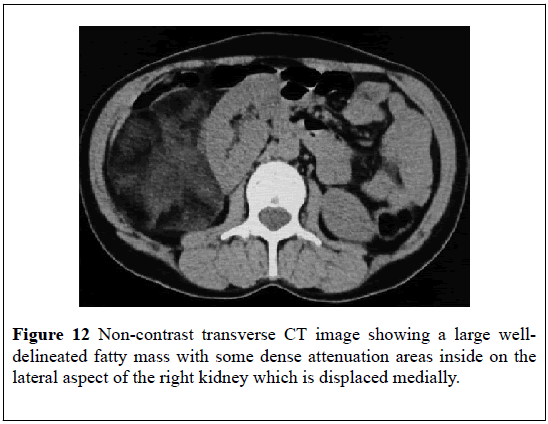
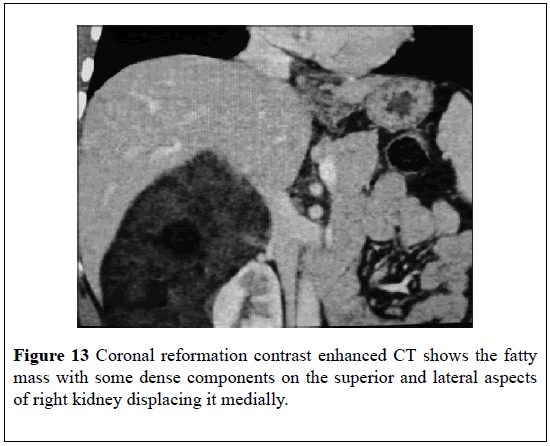
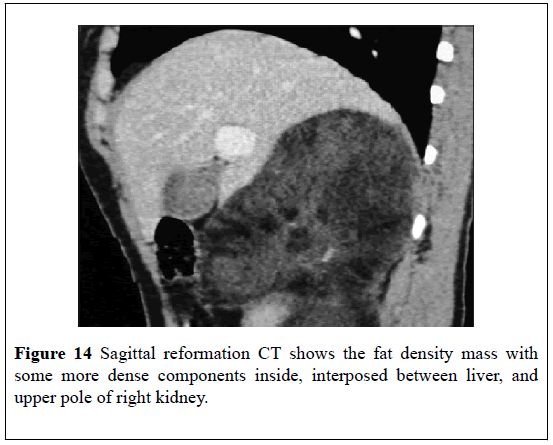
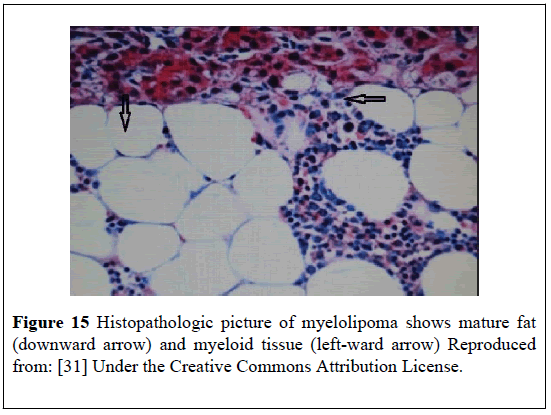
A 52-year-old man with hypertension presented with: right upper abdominal pain, a palpable right loin mass. He had ultra-sound scan which showed a hyper-echoic mass that measured 15 cm on the lateral aspect of the right kidney and which had displaced the kidney medially. He had an MDCT scan which showed a large (16 × 12) cm mass in the retroperitoneum on the superior and lateral aspect of the right kidney and which had displaced the right kidney inferiorly and medially (Figures 12-14)The mass appeared largely fatty but it also had areas of attenuation higher inside. The density of the mass on CT- scan varied between 90 Hounsfield Units (HU) in the peripheral aspect to 30 Hounsfield Units (HU) within the centre (Figures 12-14). Punctate foci of calcification were also observed within the adrenal mass. The CT scan features of the lesion were consistent with MLOA. Open right adrenalectomy was undertaken. Macroscopic examination of the specimen showed a giant mass which measured (16 × 12 × 10) cm which was surrounded by a thin capsule. Histological examination of the lesion revealed features consistent with MLOA (Figure 15). At his 3-month follow-up, he was asymptomatic and he had a CT-scan which showed no recurrence.
Figure 15: Histopathologic picture of myelolipoma shows mature fat (downward arrow) and myeloid tissue (left-ward arrow) Reproduced from: [31] Under the Creative Commons Attribution License.
This case had also indicated a link between hypertension, upper abdominal and a palpable loin mass with MLOA as well as the usefulness of radiology imaging in the diagnosis of MLOA.
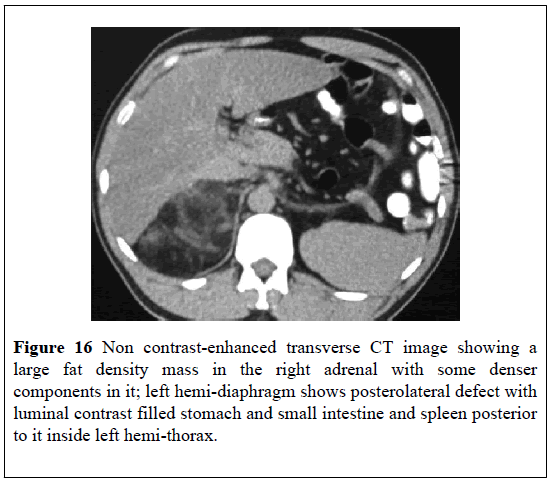
Case 2
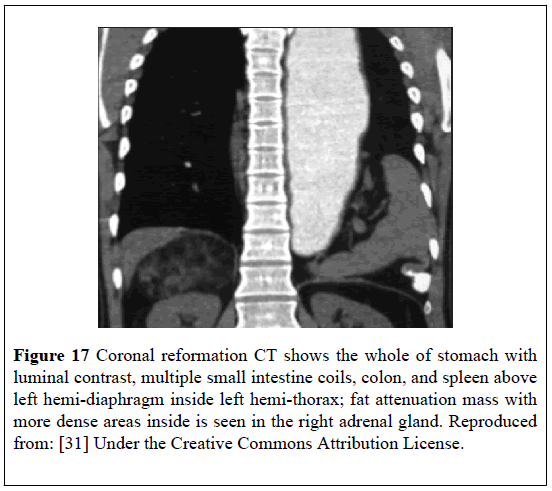
A 48-year-old man had a chest X-ray as part of assessment for his hypertension which showed stomach bubbles within his left chest. He had a CT-scan looking for a diaphragmatic hernia. The MDCT-scan demonstrated a large defect within the posterolateral left hemi-diaphragm which contained: stomach, small intestine, spleen, and colon within the left hemi-thorax (Figures 16 and 17). A well-defined fat attenuation mass which measured (10 × 8) cm was observed in the right adrenal region between the liver and the kidney with evidence of higher attenuation areas inside which indicated a diagnosis of MLOA (Figures 16 and 17). It was planned that the patient should undergo in the first instance repair of his Bochdaleck hernia before undergoing excision of the right adrenal mass. This case has re-affirmed that MLOAs could be diagnosed incidentally in the investigation of a different condition.
Figure 17: Coronal reformation CT shows the whole of stomach with luminal contrast, multiple small intestine coils, colon, and spleen above left hemi-diaphragm inside left hemi-thorax; fat attenuation mass with more dense areas inside is seen in the right adrenal gland. Reproduced from: [31] Under the Creative Commons Attribution License.
Chung et al. [32] reported a 32-year-old woman who presented with rightsided loin pain and a palpable mass in the right upper abdomen. She was anemic. Her serum adrenocorticotrophic hormone, plasma renin activity, serum aldosterone, and 24 hour urine vanillylmandelic acid levels were normal. She had CT scan of abdomen which showed retroperitoneal hemorrhage of a largetumorwith fat density in the region of the right adrenal gland. She underwent open excision of the mass of which histological examination showed a proliferation of adipocytes and myeloid tissues which was consistent with MLOA. She was well at her 6- month follow-up. This case has demonstrated a link between anemia, loin pain and a palpable abdominal mass as some of the presentations of MLOA and also has demonstrated the usefulness of CT scan of the abdomen and pelvis in demonstrating an adrenal lesion.
HSU et al. [22] reported 3 men and 3 women who had undergone surgical treatment for MLOAs. Hsu et al. [22] reported that 3 patients were diagnosed incidentally and 3 patients were symptomatic. Hsu et al. [22] stated that all the six patients did undergo surgery, including laparoscopic adrenalectomy. With regard to the outcome there was no recurrence of the lesion in any of the six patients. Hsu et al. [22] made the ensuing summations:
• Right adrenal gland was more dominant with regard to myelolipoma
• The prevalent age was from the 4th to the 6th decade
• The commonest symptoms were abdominal pain and flank pain
• MLOA is uncommon and can be confused with malignancy when the lesion is large in size (> or=6 cm)
Surgery could be reserved for: symptomatic cases, those cases which cannot be reliably diagnosed, and. large tumors that measure 6 cm or greater than 6 cm could be excised surgically or laparoscopically.
This case series would indicate that when MLOAs are adequately excised there would tend to be no recurrence of the lesion which is benign.
Matsumoto et al. [33] reported a 65-year-old man who presented with: right sided flank pain, a tender mass in the right upper abdomen. His serum biochemistry results were normal. He was slightly anemic, his white blood cell count, “C-reactive-protein,” levels, were raised. He had ultrasound- and non-contrast CT- scan of abdomen which showed a large mass between the right lobe of the liver and the right kidney then initially diagnosed as ruptured angiomyolipoma. He had renal arteriography which demonstrated that the inferior adrenal branch of the right renal artery had been compressed by tumor; nevertheless, pooled contrast fluid tumor feeding vessels had not been identified. There was no as certainable tumor feeding vessels that could be super-selectively identified for embolization. Pursuant to having the renal arteriography, he had contrast-enhanced CT scan of abdomen which demonstrated that the mass had a fatty component and the hematoma was situated within the peri-tumoral and the perirenal space. He had MRI-scan which demonstrated a heterogeneous mass with fat intensity areas in fat-suppressed T1 images. The peri-tumoral and the peri-renal haematoma had higher intensity in comparison with the tumor mass and the right kidney which confirmed that the mass was a right haemorrhagic myelolipoma. He was treated conservatively for 22 days. During the period of watchful waiting his symptoms had reduced. His haemoglobin level did not drop significantly. He had a another follow-up CT-scan which showed a larger and non-enhanced mass that measured (12 × 10 × 9) cm in comparison with the size of the mass shown in his preceding CT-scan of abdomen in the right supra-renal region. The mass had increased in size as a result of peri-renal hemorrhage. He underwent open radical excision of the adrenal mass of which histological examination showed that the lesion was a non-malignant MLOA. Matsumoto et al. [33] iterated the following:
• Their case was the 22nd reported case of spontaneous hemorrhage from MLOA with bleeding into the retroperitoneum. The characteristics of these reported cases include male dominance in that 20 out of the 22 cases involved the male and the mean age at presentation was 44 years but the ages had ranged between 20 years and 69 years; the mean tumor size of the MLOAs was 11.7 cm but the sizes had ranged between 4 cm and 205 cm; all known cases of spontaneous rupture of MLOAs were associated with symptomatic individuals; in MLOA sudden onset of acute pain tends to be associated with intra-tumoral hemorrhage; extra-tumoral hemorrhage had been rarely described [10]
• Pre-operative embolization of a ruptured myelolipoma could be useful in stabilizing patients prior to definitive surgery [34-36]
This case has demonstrated the association of abdominal pain and abdominal mass with MLOA. The case has also illustrated the usefulness of CT scan, MRI scan and selective renal artery angiography in the investigation of MLOA.
Yang et al. [37] summated two case reports of bilateral MLOA as follows: The use of pre-operative diagnostic radiological imaging including B mode ultrasound scan, CT-scans and MRI-scans were useful in helping them predict the diagnoses of bilateral MLOAs. They stated that they had used a two-stage surgery to successfully excise bilateral MLOAs in the two reported patients. They used conventional open adrenalectomy to remove the MLOAs that were greater than 6 cm, but they did use laparoscopic adrenalectomy to remove the MLOAs that were less than 6 cm. Post-operative histological examination of all the four excised adrenal glands confirmed the diagnosis of bilateral adrenal MLOA. Yang et al. [37] intimated that surgical removal of bilateral MLOA is safe, curative, as well as beneficial. Yang et al. [37] additionally stated that the two stage surgery of adrenalectomies would appear to be the best option of treatment for the patients with bilateral MLOAs because the approach to treatment does achieve optimal treatment effectiveness with minimal sequels. This article had illustrated that bilateral MLOAs can be surgically excised on at a time and a tumor that is greater than 6 cm would be best treated by means of open surgical excision and MLOA that is less than 6 cm can be treated by the laparoscopy approach.
Cody O’Dell et al. [38] reported a 71-year-old man who presented with right-sided chest pain. He had had congestive heart failure, coronary artery disease, and chronic atrial fibrillation for which was on rivaroxaban. He had a CT angiogram to exclude pulmonary embolism which showed an incidental low-density right adrenal mass with an associated adjacent fluid. He had contrast CT scan of abdomen and pelvis which showed a retroperitoneal hemorrhage which had arisen from a fat containing right adrenal mass that was consistent with spontaneous hemorrhagic right MLOA. His rivaroxaban medication was stopped. He underwent a transfemoral right renal artery angiography that showed a supernumerary right renal artery supplying the adrenal gland with the myelolipoma and this was successfully treated by trans-catheter super-selective embolization of the arterial supply to the bleeding MLOA thus avoiding the morbidity of open or laparoscopic adrenalectomy as well as General anaesthesia. This case report has re-affirmed that MLOA could be diagnosed as an incidental finding on radiology imaging (CT scan in this case). The case has also confirmed spontaneous hemorrhage in association with MLOA and in this case, there was an additional link with utilization of rivaroxaban. Furthermore, the case report has iterated the usefulness of renal artery angiography in the investigation of MLOA.
Ansari et al. [39] reported a 40-year-old man who presented with breathing difficulties and right upper abdominal pain. He had CT- scan which revealed a large right adrenal mass that had encompassed the inferior vena cava. His blood haemoglobin level was 7.8 g/d L due to internal hemorrhage into the adrenal mass. He underwent selective angiography and super-selective embolization of the arterial flow to the right adrenal mass. A hypertensive emergency pursued the embolization procedure. His plasma and urine normetanephrine levels were elevated; nevertheless, the corresponding metanephrine levels were within normal range. It was adjudged that surgical operation to remove the adrenal mass was necessitated and a clonidine suppression test in the surgical intensive care unit was undertaken which resulted in 60% suppression of the serum norepinephrine concentration concentrations and hence it was concluded that there was very low probability that the patient had pheochromocytoma. He underwent open-resection of 3.07 kilogram mass in multiple pieces. The largest portion of the mass which did measure (32 × 25 × 13.5) cm was observed to have a well-circumscribed tan-green and a partially necrotic area that measured (5.5 × 4 × 3) cm which was completely surrounded by adipose tissue, with many haemorrhagic and necrotic areas which constituted majority of the specimen. Histology of the mass showed extensively necrotic areas of about 80% with focal viable areas of that were typified by tri-lineage haematopoietic elements, mature adipose tissue, and thick fibrous bands. Only small areas of normal adrenal gland were observed. Immunohistochemistry stains for chromogranin were negative for negative in thetumoras well as in the normal adrenal gland. The patient’s post-operative blood pressure remained normal and he did not require any anti-hypertension medication. Ansari et al. [39] made the ensuing conclusions:
• A giant myelolipoma with compressive effects could mimic pheochromocytoma
• The clonidine suppression test proved to be a simple supplementary test to differentiate pheochromocytoma and hyper-adrenergic state of critical illness
This case report has illustrated that even though more commonly MLOAs tend to be confined to the adrenal glands, occasionally MLOAs could be large enough to encompass the inferior vena cava and they could also bleed. The role of selective renal arteriogram and super-selective embolization of the MLOA as an initial step was documented as wells as the possibility of the development of hypertensive crisis linked with such embolization procedures therefore clinicians need to watch out for such a scenario and to treat any hypertensive crisis that may emanate.
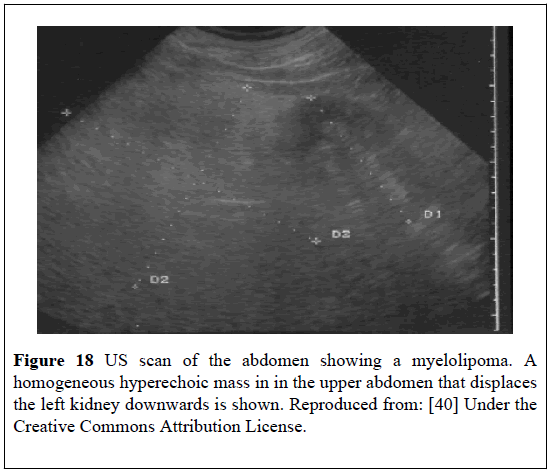
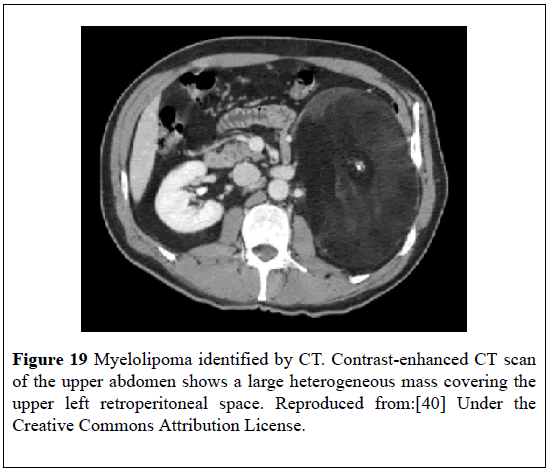
Brogna et al. [40] reported a 52-year-old man with hypertension who had ultra-sound scan that showed a large hyper-echoic mass, interposed between the spleen and the left kidney which was diagnosed as left MLOA based upon its structural features and position (Figure 18). He had CT-scan of abdomen which confirmed the diagnosis of the left MLOA (Figure 19). All his pre-operative biochemistry tests were normal with the exception of high serum cortisol level, which was adjudged to be caused by overproduction by the adrenal lesion and this was also conjectured to be responsible for the patient’s hypertension. He underwent a successful surgical left adrenalectomy following which his blood pressure returned to normal. Histological examination of the specimen confirmed MLOA.
Figure 18: US scan of the abdomen showing a myelolipoma. A homogeneous hyperechoic mass in in the upper abdomen that displaces the left kidney downwards is shown. Reproduced from: [40] Under the Creative Commons Attribution License.
Figure 19: Myelolipoma identified by CT. Contrast-enhanced CT scan of the upper abdomen shows a large heterogeneous mass covering the upper left retroperitoneal space. Reproduced from:[40] Under the Creative Commons Attribution License.
Brogna et al. [40] made the following conclusions:
• The “incidental” finding of an adrenal mass requires careful diagnostic study to plan adequate treatment
• Both ultra-sound scan and blood tests for adrenal hormones had been helpful in establishing the diagnosis which enabled them to undertake the appropriate treatment after taking into consideration the size of the tumor and the probable hormonal production of the adrenal lesion
It would be argued that this case is important in that it has documented an association between hypertension, high serum cortisol level and MLOA.
Al-Thani et al. [41] reported a 48-year-old woman who had right hypochondrium pain. She had microcytic iron deficiency anemia with beta thalassemia trait. She also had right MLOA with histopathological evidence of haematopoietic cells (EMH). She underwent open adrenalectomy with good post-operative recovery. Al-Thani et al. [41] made the ensuing conclusions: EMH could manifest with many clinical haematological disorders; surgical management would be inevitable in certain adrenal EMH cases especially when there is a large adrenal mass.
Kumar et al. [42] reported two cases of MLOA as follows:
Case 1
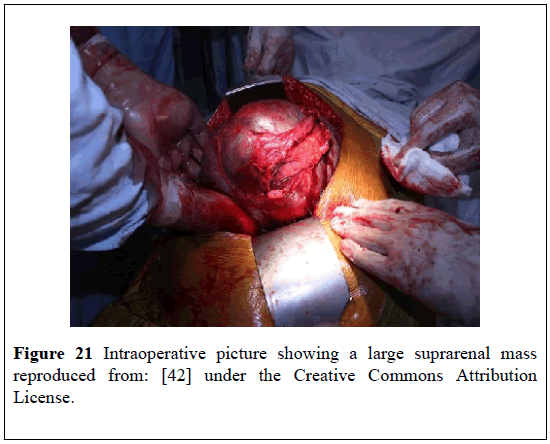
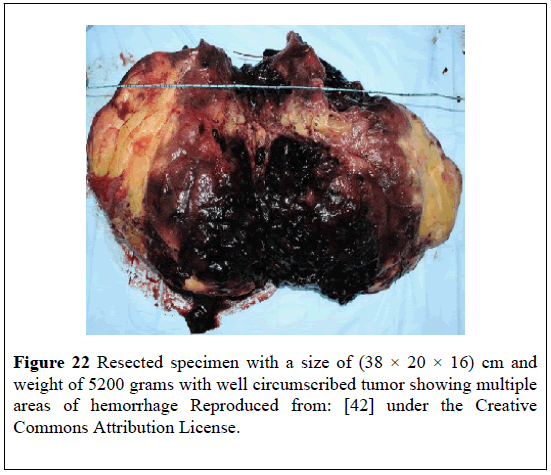
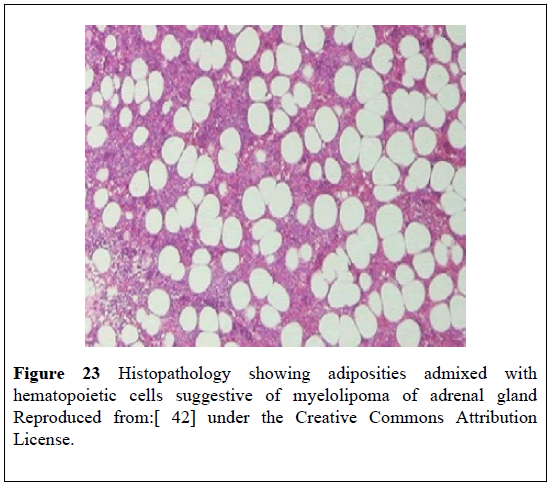
A 40-year-old man presented with: dizziness, difficulty in breathing, and upper abdominal pain, large palpable abdominal mass, anaemia which required blood transfusion. He had ultrasound scan of abdomen which revealed a large hyper-echoic supra-renal mass that measured (30 × 20) cm and displaced the right kidney downwards. He subsequently had CT scan of abdomen which showed a (35 × 19) cm supra-renal mass which had pushed the kidney downwards. The supra-renal mass was hypo-dense, non-contrast-enhancing and had an attenuation value that was suggestive of fat of -19 Hounsfield Units (HU) in many areas that had hemorrhages into the lesion (Figure 20). He had biochemistry for cortisol, normetanephrine, and metanephrine which were normal. He underwent open right adrenalectomy and the specimen measured (38 × 20 × 16) cm and weighed 5200 grams. The excised mass had a wellcircumscribedtumorthat had multiple areas of hemorrhage (Figures 21 and 22); Its histological examination showed mature adipose tissue together with tri-lineage haematopoietic elements which did not have any evidence of dysplasia and the features were consistent with MLOA (Figure 23). At his 6-months follow-up he had ultrasound scan of abdomen which did not reveal any recurrence. It would be argued that this case report had firstly demonstrated that patients with myelolipoma of the adrenal gland could present with non-specific symptoms and also that if fine needle aspiration of the adrenal mass was undertaken there would be histology confirmation of the diagnosis of myelolipoma of the adrenal gland pre-operatively. Nevertheless, it would be argued that when myelolipoma of the adrenal gland is associated with non-specific symptoms, surgical operation in the form of adrenalectomy would be required to eradicate the symptoms.
Figure 20: CECT abdomen showing a 35 × 19 cm suprarenal mass hounsfield density (HU -19): Reproduced from: [42] under the creative Commons Attribution License.
Figure 21: Intraoperative picture showing a large suprarenal mass reproduced from: [42] under the Creative Commons Attribution License.
Figure 23: Histopathology showing adiposities admixed with hematopoietic cells suggestive of myelolipoma of adrenal gland Reproduced from: [42] under the Creative Commons Attribution
License.
Case 2
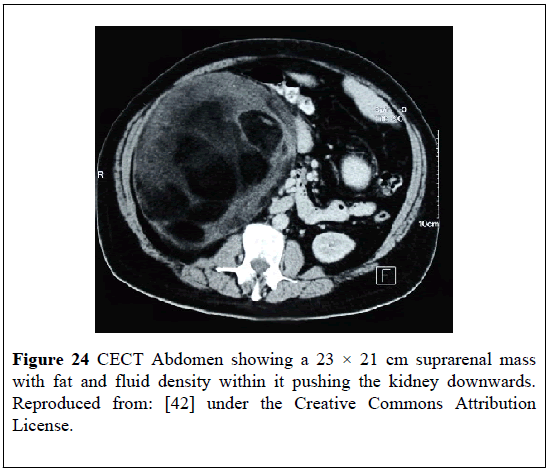
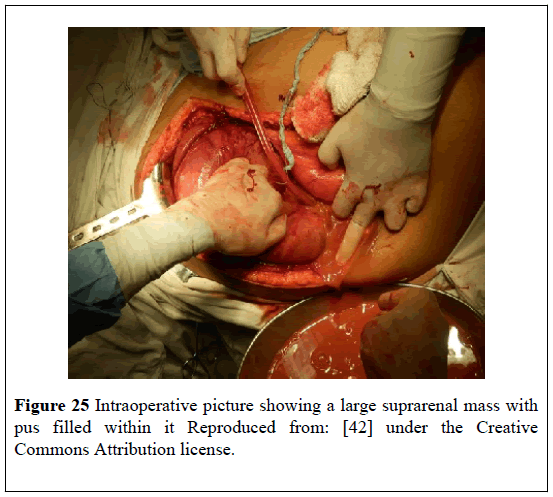
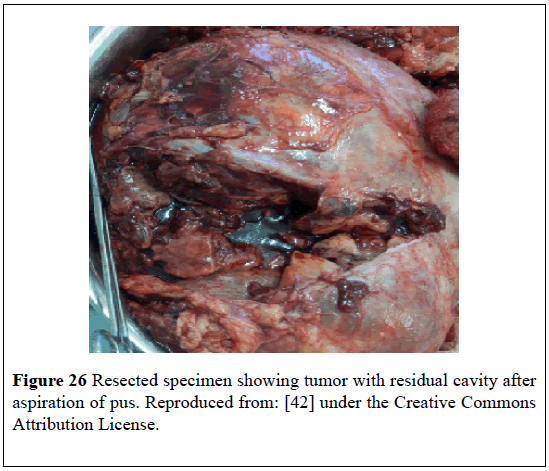
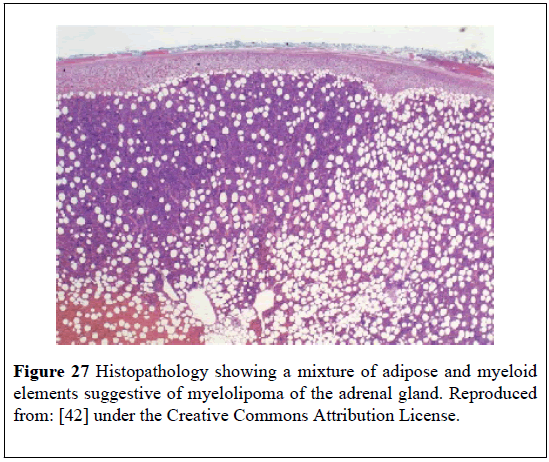
A 50-year-old diabetic man presented with: fever, chills, vomiting, upper abdominal pain, tachycardia, hypotension, anemia, visible lump in his abdomen. He had ultrasound scan of abdomen which showed a large hypo-echoic area that measured (22 × 17) cm within his sub-hepatic region. He had CT-scan which showed a (23 × 21) cm right supra-renal mass with fat and fluid density within it and which had pushed the kidney downwards (Figure 24). He underwent laparotomy and drainage of an abscess and excision of the mass (Figures 25 and 26). Histological examination of the specimen confirmed presence of MLOA. Microscopic examination showed that thetumorhad included: mature adipose tissue which did not have any nuclear atypia within the adipocytes; some fibroblasts; focally haematopoietic cells; areas of hemorrhage; necrosis; and inflammation. Culture of the drained pus grew pseudomonas which was sensitive to piperacillin and tazobactam (Figure 27). He had ultrasound scan 6 months later which did not show any recurrence. This case report is important in that it had illustrated that myelolipoma of the adrenal gland could present with non-specific symptoms.
Figure 24: CECT Abdomen showing a 23 × 21 cm suprarenal mass with fat and fluid density within it pushing the kidney downwards. Reproduced from: [42] under the Creative Commons Attribution License.
Figure 25: Intraoperative picture showing a large suprarenal mass with pus filled within it Reproduced from: [42] under the Creative Commons Attribution license.
Figure 27: Histopathology showing a mixture of adipose and myeloid elements suggestive of myelolipoma of the adrenal gland. Reproduced from: [42] under the Creative Commons Attribution License.
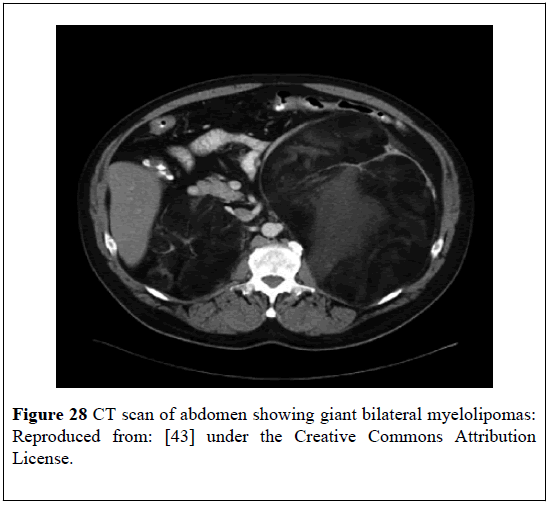
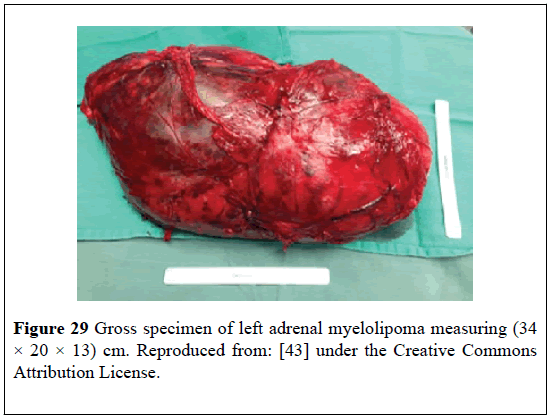
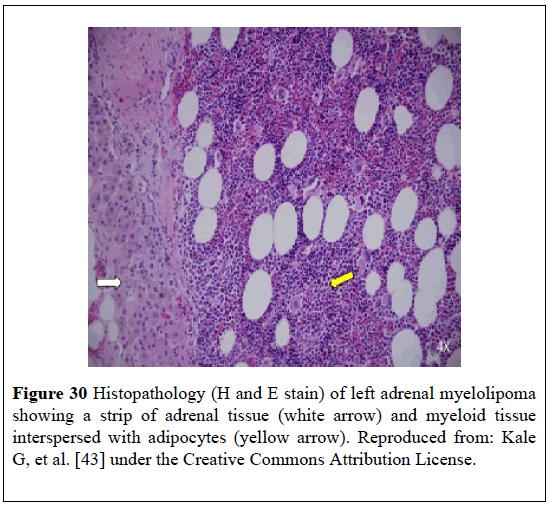
Kale et al. [43] stated that myelolipomas had been reported in individuals who had Congenital Adrenal Hyperplasia (CAH) and that Adrenocorticotrophic Hormone (ACTH) excess as is encountered in nonadherence to glucocorticoid therapy could be responsible for the development of tumor. Kale et al. [43] reported a 51-year-old man who had classic salt-wasting CAH that had been managed on prednisolone and fludrocortisone, who had presented with chronic back pain and was found to have giant bilateral retroperitoneal masses. He had CT- scan of abdomen which showed that the masses were heterogeneous, but they did contain predominantly low-density fat attenuation (Figure 28). He underwent bilateral resection of the masses. Histopathological examination of the masses revealed features consistent with MLOAs. The left adrenal mass measured (34 × 20 × 13) cm and had weighed 4.7 kilograms (Figure 29). The right tumor measured 20 cm in its largest diameter. Adrenal tissue was present within the specimen (Figure 30).
Figure 28: CT scan of abdomen showing giant bilateral myelolipomas: Reproduced from: [43] under the Creative Commons Attribution License.
Figure 29: Gross specimen of left adrenal myelolipoma measuring (34 × 20 × 13) cm. Reproduced from: [43] under the Creative Commons Attribution License.
Figure 30: Histopathology (H and E stain) of left adrenal myelolipoma showing a strip of adrenal tissue (white arrow) and myeloid tissue interspersed with adipocytes (yellow arrow). Reproduced from: Kale G, et al. [43] under the Creative Commons Attribution License.
Kale et al. [43] reported that the patient had stated that he had been compliant on long-term basis with regard to his glucocorticoid treatment; nevertheless, he had not had any biochemical monitoring of ACTH level. In view of this Kale et al. [43] intimated that it was not clear if ACTH excess had contributed to the development of the large tumors in their patient. Kale et al. [43] stated that they had presumed that both adrenal glands had been inadvertently removed during the operation and the patient had been treated with physiological replacement doses of hydrocortisone and fludrocortisone pursuant to the operation.
Nevertheless, adrenalectomy could be considered as an option of treatment in patients who have classical CAH under certain circumstances, in order to avoid complications of glucocorticoid excess. Kale et al. [43] summarized the learning points from their case report as follows:
• Myelolipomas should be considered in the differential diagnosis of adrenal or retroperitoneal masses in patients who have CAH
• CT-scans of myelolipomas tend to show heterogeneous masses that have low-density mature fat interspersed with more dense myeloid tissue
• Myelolipomas tend to be unilateral and they tend to less than 4 cm; nevertheless, very large and bilateral tumors had been reported
• Treatment of CAH generally entails the use of supra-physiological doses of glucocorticoid to suppress adrenal hyperandrogenism. Bilateral adrenalectomy would constitute an alternative option of treatment in patients who have CAH
• There is an association between ACTH excess and increased incidence of MLOA; nevertheless, the direct causal link has not been established yet
Based upon this case report it would argued that there is the need for clinicians to investigate or undertake research to establish whether or not ACTH excess does lead to the development of myelolipoma of the adrenal gland. It would also be argued that if fine needle aspiration of the adrenal was undertaken prior to the adrenalectomies histological diagnosis of myelolipoma of the adrenal gland would have been established preoperatively.
Chakrabarti et al. [44] reported a 40-year-old woman who had presented with right flank pain. She had ultrasound scan of abdomen which revealed a large hyper-echoic mass that had irregular margins under the liver and had pushed the right kidney down. A provisional diagnosis of retroperitoneal sarcoma with an intra-lesional hemorrhage was made. Her serum cortisol, catechol amines, serum dopamine, serum dopamine, urinary vanillylmandelic acid, 17-keto steroids, serum testosterone, and her routine blood tests were normal. Because of worsening pain she underwent surgical excision of the mass. The outer surface of the excised mass looked congested and the cut section of the mass did show hemorrhage and some preserved yellowish areas with greyish areas at the periphery of the mass. Histological examination of the specimen showed hematopoietic elements which had consisted of erythroid, myeloid cells, and megakaryocytes which had been admixed with mature adipose tissue. The normal histology of adrenal gland was noticed to have been preserved in the periphery. A diagnosis of large MLOA with hemorrhage was made. It would be argued that this paper had illustrated or confirmed that spontaneous hemorrhage could occur in large myelolipomas of the adrenal gland, hence large myelolipomas of the adrenal gland should be considered for elective adrenalectomy by the laparoscopy or open surgical approach in oder to avoid sudden spontaneous hemorrhage. It would also be argued that perhaps if a computed tomography (CT) scan had been undertaken pre-operatively a diagnosis of myelolipoma of the adrenal gland would have been made pre-operatively.
Destouni et al. [45] reported a 72-year-old man who presented with lower urinary tract obstructive symptoms. His rectal examination revealed an enlarged benign feeling prostate. He had ultrasound scan of abdomen and renal tract and CT-scan which showed a mass in the right adrenal gland The CT-scan also showed a second mass in the left adrenal gland. The differential diagnosis initially was either metastases from carcinoma of the prostate gland or primary adrenal tumor. His serum PSA was within normal range. He underwent surgical excision of the prostate gland and histological examination of the prostate showed features of benign prostatic hyperplasia and chronic prostatitis. A CT-guided fine needle aspiration of the right adrenal mass was undertaken. Microscopic examination of the aspirate showed cellular material which contained mature adipose tissue fragments and numerous tri-lineage haematopoietic cells against a bloody background. The appearance was described as mimicking red bone-marrow. The bone-marrow elements were observed to be normal in various stages of maturation. The cytological features of the fine needle aspirate, was adjudged to be consistent with the diagnosis of MLOA. Destouni et al. [45] stated that Fine Needle Aspiration (FNA) has become a diagnostic method which is accepted globally and it is reliable and simple for the diagnosis of myelolipoma. It would be argued that the lesson learnt from this article is that FNA of an adrenal mass that is adjudged to have radiology imaging features of myelolipoma could be undertaken to confirm histology diagnosis of myelolipoma and if the diagnosis is confirmed then conservative management could be adopted rather than subject the patient to adrenalectomy.
Castillo et al. [46] reported on 226 laparoscopic adrenalectomies undertaken in their institution and of these 19 (8%) of the cases corresponded to laparoscopic adrenalectomy for myelolipoma. The mean age of individuals who had undergone laparoscopic adrenalectomy for myelolipoma was 53.8 years but the ages ranged between 35 years and 75 years and the male to female ratio was 2:1. Castillo et al. [46] reported that 19 laparoscopic adrenalectomies were performed on 18 individuals. !6 of the myelolipoma lesions (84%) were in the right adrenal gland and 2 of the lesions (16%) were in the left adrenal gland. The surgical time ranged between 45 minutes and 150 minutes and the mean surgical time was 84.7 minutes. The volume of bleeding did range from 0 millilitres to 300 millilitres and the mean volume of bleeding was 28.5 millilitres. One of the patients did require blood transfusion. None of the laparoscopic adrenalectomies required to be converted into open adrenalectomy and no intra-operative complication developed during the procedures. The duration of hospital stay did range from 1 day to 4 days and the average duration of stay in hospital was 2.1 days. During the immediate postoperative period no complications were encountered. The maximum diameter of thetumorranged between 4.5 cm and 14 cm. Pathology examinations of all the tumors showed features that confirmed the diagnosis of myelolipoma of the adrenal gland. Castillo et al. [46] made the following conclusions:
• MLOA is an infrequent, benign entity which could rarely become symptomatic due to spontaneous hemorrhage
• Typical radiological imaging features of MLOA do allow conservative management of the lesion in small asymptomatic cases
• With regard to cases of MLOA laparoscopic surgery would be a safe and feasible technique which is associated with reasonable operating time, limited blood loss, short hospital and short convalescence
It would be argued that even though the authors had shown that laparoscopic adrenalectomy is a safe procedure as an option of treatment, perhaps the option of conservative management could have been adopted for some of the myelolipomas especially small ones and this would avoid the morbidity of a surgical operation due to the fact that myelolipoma is a benign lesion.
Yamashita et al. [47] reported six cases of which 3 patients underwent laparoscopic right adrenalectomy and 3 patients underwent open right adrenalectomy all for MLOA. They reported the following: The maximum diameter of the adrenaltumorwith regard to tumors removed laparoscopically had ranged between 3.0 cm to 4.4 cm and the mean maximum diameter of the tumors was 3.5 cm. The maximum diameter of the adrenaltumorwith regard to tumors removed by open laparotomy technique had ranged between 7.0 cm and 9.5 cm and the mean maximum diameter was 7.1 cm. The duration of the operation with regard to the laparoscopic adrenalectomies had ranged between 117 minutes and 188 minutes and the median duration of the procedure was 152 minutes. The duration of the operation with regard to the open adrenalectomies had ranged between 153 minutes and 230 minutes and the median duration of the procedure was 218 minutes. The blood loss related to the laparoscopic adrenalectomies had ranged between 20 millilitres to 120 millilitres with a mean blood loss of 50 millilitres. The blood loss related to the open adrenalectomies had ranged between 62 millilitres to 1237 millilitres with a mean blood loss of 290 millilitres. The post-operative length of hospital stay with regard to the laparoscopic adrenalectomies had ranged between 4 days and 4 days and the mean length of post-operative hospital stay was 4 days. The post-operative length of hospital stay with regard to the open adrenalectomies had ranged between 11 days and 13 days and the mean length of post-operative hospital stay was 11days. There was no case of conversion from laparoscopic surgery to open surgery. There was no case of post-operative morbidity or mortality with regard to both the laparoscopic procedures and the open procedures. They concluded that laparoscopic adrenalectomy is a safe, feasible, and effective approach to the surgical management of MLOA and this has been assisted by advances in pre-operative radiological imaging diagnostic techniques. It would be argued that since the blood loss is less with regards to laparoscopic and the post-operative in hospital is less with regards to open surgery, in areas of the world where laparoscopic surgery is well developed, patients who are diagnosed as having myelolipoma of the adrenal gland should be offered both options of surgical treatment and they should be allowed to decide which surgical option they would prefer.
Campos Arbulu et al. [48] reported a 33-year-old woman who was diagnosed as having 14 cm diameter non-functioning right adrenal incidentaloma, in which the imaging features were suggestive of myelolipoma. Considering the benign nature of the tumor, laparoscopic resection of thetumorwas undertaken. Histopathology of the tumor showed features consistent with the diagnosis of myelolipoma and the specimen did weigh 444 grams. The patient had an uneventful postoperative recovery. They iterated that laparoscopic adrenalectomy for a giant myelolipoma is feasible and successful. It would be argued that the pre-operative diagnosis of myelolipoma was re-assuring to the patient prior to the operation in that she was aware that her large adrenal lesion was not a malignant tumor.
Conclusion
Myelolipomas (MLOAs) are rare benign tumors that tend to more commonly affect the right adrenal gland and tend to exhibit benign biological behaviour but 10% tend to be associated with endocrine disorders. Diagnosis of MLOA can be made based upon CT scan evidence of fat density well circumscribed localized lesion in the adrenal gland and histological confirmation of diagnosis can be achieved by examination of radiological imaging guided aspiration/biopsy of the lesion or from the surgically excised lesion. Considering the fact that MLOAs are benign small MLOAS should be treated conservatively and surgical management should be reserved for lesions that show evidence of increase in size with time, hemorrhage into the MLOA, symptomatic MLOAs, large MLOAs 6cm or larger, cases of uncertain diagnosis when malignancy cannot be confirmed.
REFERENCES
- Gellert LL. Adrenal gland and paraganglia other benign cortical lesions. Myelolipoma PathologyOutlines.com 2017 Jan 27.
- Weerakkody Yuranga et al. Adrenal myelolipoma ! Radiology Reference Article.
- Meyer A, Behrend M. Presentation and therapy of myelolipoma. Int J Urol. 2005;12:239-43.
- Gierke E. Uber knochenmarksgewebe in den nebenniene. Beitn Pathol Anat. 1905;7:311-25.
- Obenling C. Les formations myelolipomatouses. Bull Cancer. 1929;18:234-46.
- Lee J K. Computed body tomography with MRI correlation. Lippincott Williams and Wilkins. 2006; ISBN: 0781745268.
- Kenney PJ, Wagner BJ, Rao P, et al. Myelolipoma: CT and pathologic features. Radiology. 1998;208:87-95.
- Cyran KM, Kenney PJ, Memel DS, et al. Adrenal myelolipoma: AJR Am J Roentgenol. 1996;166:395-400.
- Barman S, Chandra MK, Mukhopadhyay M. Adrenal mylolipoma: An incidental and rare benign tumor in children. J Indian Pediatr Surg. 2014;19:236-8.
- Doddi S, Singhai T, Leake T, et al. Management of an incidentally found large adrenal myelolipoma: a case report. Case Journal. 20092:8414.
- Craig WD, Farnburg-Smith JC, Henry LR, et al. Fat containing lesions of the retroperitoneum: radiologic-pathologic correlation. Radiographics. 2009;29:261-90.
- Routhier JR, Wordfield CA, Mayo-smith WW. AJR teaching site: fat containing retroperitoneal mass presenting with acute flank pain. AJR Am J Roentgenol. 2009;192:5122-4.
- Brant WE, Helms CA. Fundamentals of diagnostic Radiology Lippincott. Williams and Wilkins. 2007: ISBN: 0781761352.
- Merchant SH, Herman CM, Amin MB, et al. Myelolipoma associated with adrenal ganglioneuroma. Archives of Pathology and Laboratory Medicine 2002;126:736-7.
- Mathews K, Sasson A, Cohen S. Pathologic quiz case: A woman with abdominal fullness. Archives of Pathology and Laboratory Medicine. 2004; 128:703-4.
- Ishikawa H, Tachibana M, Hata M, et al. Myelolipoma of the adrenal gland. J Urol. 1981;126:777-79.
- Tulcinsky DB, Deutsch V, Bubis JJ. Myelolipoma of the adrenal gland. British Journal of Surgery. 1970;57:10.
- Pagana TJ, Karasick SJ, Karasick D, et al. Myelolipoma of the adrenal gland. The American Journal of Surgery. 1981;141:282-5.
- Ramirez M, Misra S. Adrenal myelolipoma: To operate or not? A case report and review of the literature. Int. J Case Reports. 2014; 5:494-6.
- Ioannidis O, Papaemmanonil S, Chatzopoulos S, et al. Giant bilateral symptomatic adrenal myelolipomas associated with congenital adrenal hyperplasia. Pathol Oncol Res. 2011.
- Wani N, Kosar T, Rawa I, et al. Giant adrenal myelolipoma: incidentaloma with a rare incidental association. Urol Ann. 2010;2:130.
- HSU SW, Shu K, Lee WC, et al. Adrenal myelolipoma: a 10 year single center experience and literature review Kaohsiung J Med Sci 2012;377-82.
- Al Harthi B, Riaz MM, Al Khallaf AH, et al. Adrenal myelolipoma a rare benigntumormanaged laparoscopically: Report of two cases. J Minim Access Surg. 2009;5:118-20.
- Nabi J, Rafiq D, Authoy FN, et al. Incidental detection of adrenal myelolipoma: A case report and review of literature. Case Reports in Urology Volume. 2013(2013);ID789481:3.
- Hisamatsu H, Sakai H, Tsuda S, et al. Combined adrenal adenoma and myelolipoma in a patient with Cushings syndrome: Case report and review of the literature. Int J Urol. 2004;11:416-8.
- Meteoglu I, Kacar F, Culhaci N, et al. Adrenal myelolipoma: A case report. The Internet Journal of Urology. 2004;2.
- Bhansali A, Dash RJ, Singh SK, et al. Adrenal myelolipoma: Profile of six patients with a brief of literature. Int J Endocrinol Metab. 2003;1:33-40.
- Rao P, Kenney P J, Wagner B J, et al. Imaging and pathologic features of adrenal myelolipoma. Radiographics. 1999;17:1373-85.
- Puneet, Tiwary S K, Singh S, et al. Adrenal myelolipoma: A case report. The Internet Journal of Third World Medicine. 2006;3.
- Civrilli K, Damry N, Steppe R, et al. Bilateral adrenal myelolipoma. JBR-BTR. 2008;91:90-91.
- Wani NA, Kosar T, Rawa IA, et al. Giant adrenal myelolipoma: incidentaloma with a rare jncidental association. Urol Ann. 2010;2:130-33.
- Chung HM, Luo FJ, Wu TM, et al. Adrenal myelolipoma with spontaneous hemorrhage. Urol Sci. 2010;21:152-54.
- Matsumoto M, Shigemura K, Fujisawa M. Spontaneous rupture of adrenal myelolipoma. Uro today Int J. 2011;4:55.
- Catalano O. Retroperitoneal hemorrhage due to a ruptured adrenal myelolipoma:A case report. Acta Radiol. 1996;37:688-90.
- Hofmockel G, Dammrich J, Garcia HM, et al. Myelolipoma of the adrenal gland associated with contralateral renal cell carcinoma: case report and review of the literature. J Urol. 1995;153:129-32.
- Chng SM, Lin MB, Ng FC, et al. Adrenal myelolipoma presenting with spontaneous retroperitoneal hemorrhage demonstrated on computed tomography and angiogram-A case report. Ann Acad Med Singapore. 2002;31:228-30.
- Yang Y, Ye LY, Yu B, et al. Two case reports of bilateral adrenal myelolipomas. World J Clin Cases. 2015;3:853-60.
- Cody O’Dell M, Liu B, Fursevitch D, et al. Embolization of spontaneous haemorrhagic adrenal myelolipoma with variant adrenal arteries. J Vasc Interv Radiol. 2015;26:1086-88.
- Ansari MZ, De La Garza MM, Deavers M, et al. Hypertensive emergency following embolization of a large adrenal myelolipoma-adrenal medullary infarction, pheochromocytoma, or acute sympathetic discharge? a case report and literature review. AACE Clinical Case Rep. 2015;1:e216-e220.
- Brogna A, Scalisi G, Ferrara R, et al. Giant secreting adrenal myelolipoma: A case report. J Med Case Reports. 2011;5:298.
- Al-Thani H, Al-Sulaiti M, El-Mabrok G, et al. Adrenal extramedullary hematopoiesis associated with beta-thalassemia trait in an adult woman: A case report and review of literature. Int J Surg Case Rep. 2016;24:83-87.
- Kumar S, Javant K, Prasad S, et al. Rare adrenal gland emergencies: A case series of giant myelolipoma presenting with massive hemorrhage and abscess. Nephrourol Mon. 2015;7:e22671.
- Kale G, Pelley GM, Davis DB. Giant myelolipomas and inadvertent bilateral adrenalectomy in classic congenital adrenal hyperplasia Endocrinol Diabetes. Metab Case Rep. 2015;2015:150079.
- Chakrabarti I, Ghosh N, Das V. Giant adrenal myelolipoma with hemorrhage masquerading as retroperitoneal sarcoma. J Midlife Health. 2012;3:42-44.
- Destouni C, Karasavvidou F, Pazaitou K,et al. Adrenal myelolipoma diagnosed by fine needle aspiration biopsy. Archive of Oncology. 2001;9:185-187.
- Castillo OA, Vitagliano G, Cortes O, et al. Laparoscopic adrenalectomy for adrenal myelolipoma. Arch Esp Urol. 2007;60:217-21.
- Yamashita S, Kaoru Furushima KI, Fukushima J, et al. Laparoscopic versus open adrenalectomy for adrenal myelolipoma. Annals Medicine Surgery. 2014;3:34-6.
- Campos AAL, Sadava EE, Kerman J, et al. Giant adrenal myelolipoma. Right laparoscopic adrenalectomy. Medicina (B Aires). 2016;76:249-50.