Myopathy with rods and cores
Received: 13-Dec-2017 Accepted Date: Jan 15, 2018; Published: 22-Jan-2018
Citation: Tiwana H, Elangovan C, Ahmed A. Myopathy with rods and cores. J Nueropathol. 2018;1(1):1-2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objectives: Congenital myopathies are muscle disorders with variable clinical presentation. We present a case with characteristic history who was diagnosed late in the life, with typical findings on pathologic specimen.
Methods: Case report.
Results: The 65-year-old female presents with worsening weakness, restricting daily activities. Weakness is described as proximal muscle weakness which has been slowly progressive. Duration of symptom is since birth and patient has a history of delayed motor development. Patient also has strong family history of similar symptoms with her mother having scoliosis, weakness and high arch feet. Patient has a daughter who also suffers from proximal muscle weakness. The patient’s daughter has 5 kids and 3 of them have similar weakness. Proximal muscle weakness, scoliosis and high arched feet were evident on examination. EMG/Nerve conduction studies revealed findings consistent with “mild myopathy process”. Right deltoid muscle biopsy confirmed myofiber atrophy and myopathy with cores and rods.
Conclusions: Core-rod myopathy is a relatively rare form of congenital myopathy. It is known by the presence of cores and rods in separate regions of same or different muscle fibers. This case highlights the need to obtain neuromuscular evaluation for patients who present early in life with minimal weakness pattern, which is also slowly progressive. Timely evaluation and diagnosis will allow patients to make informed decision regarding their career choices as well as starting a family.
Keywords
Congenital myopathy; Myopathy with cores and rods
Introduction
Congenital myopathies are muscle disorders with variable clinical presentation. We present a case with characteristic history that was diagnosed late in the life, with typical findings on pathologic specimen.
Case Report
The 65-year-old female presents with worsening weakness restricting daily activities. Weakness is described as proximal muscle weakness which has been slowly progressive. Duration of symptom is since birth and patient had a history of delayed motor development. She began walking at 2 years of age and was unable to climb stairs till 7 years of age. Patient described occasions where she was not able to stand up and had to use her hands to climb up. In school, she lagged behind her peers in physical activities like running and sports. She also has strong family history of similar symptoms with her mother having scoliosis, weakness and high arch feet. Patient has a daughter who also suffers from proximal muscle weakness. The patient’s daughter has 5 kids and 3 of them have similar weakness. Pertinent positives on examination findings include MRC strength grading in upper extremities as follows (right/left): Deltoids 4+/4+, biceps 5-/5, triceps 5-/5, wrist extension 5/5, neck flexion 5/5 and interossei 5/5. In the lower extremities, strength is graded as follows (right/left): Hip flexion 4/4+, knee flexion 5/5 and extension 5/5, foot dorsiflexion 5/5 and plantar flexion 5/5. She gets up with difficulty and uses her hands to push against the side of the chair. Her casual gait is wide based. Scoliosis and high arched feet noted.
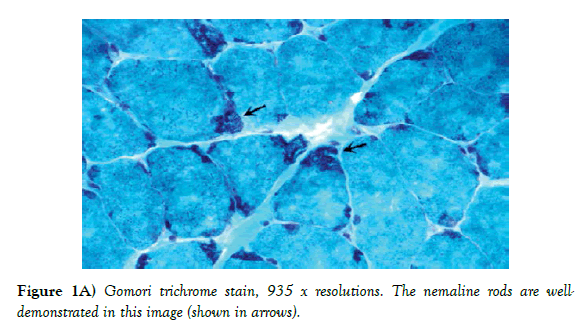
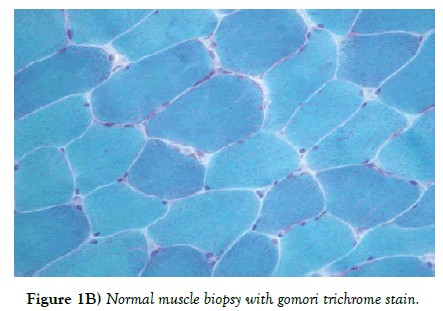
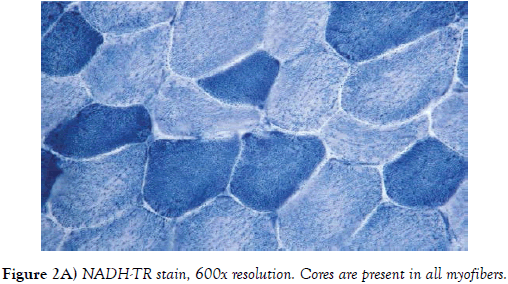
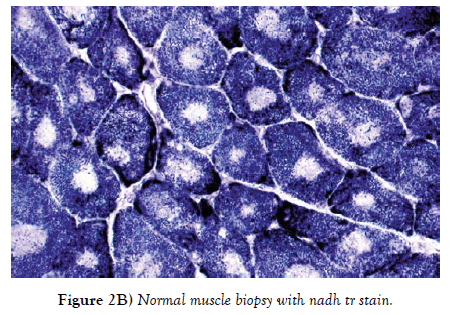
She underwent basic workup which was unremarkable. Creatine Kinase was 71. EMG/Nerve conduction studies revealed findings consistent with “mild myopathy process”. Right deltoid muscle biopsy confirmed myofiber atrophy and myopathy with cores and rods (Figures 1A-B and 2A-B).
Figure 1B) Normal muscle biopsy with gomori trichrome stain.
Figure 2B) Normal muscle biopsy with nadh tr stain.
Discussion
Congenital myopathies are a heterogeneous group of primary muscle disorders [1]. Clinical presentation is variable and common symptoms include weakness, muscle cramps and gait dysfunction. There are many types of congenital myopathies which are divided into broad categories as follows:
Congenital myopathy with cores
Cores are well-demarcated, round areas in the cytoplasm of muscle fibers, which lack oxidative staining. The cores have decreased adenosine triphosphatase (ATPase) activity but in many cases the ATPase activity is preserved [2]. It has further types:
➢ Central core disease: This is an autosomal inherited muscle disorder, characterized by the presence of cores in muscle fibers. Presentation is early in life, usually in infancy or early childhood, with mild proximal weakness that persists throughout life [3]. This variety of myopathy is found to be associated with malignant hyperthermia, which is a life-threatening anesthetic reaction. It causes a rise in body temperature, muscular rigidity and muscular breakdown, grossly elevated creatine kinase, and acidosis [4].
➢ Multiminicore disease : This is an autosomal recessive congenital myopathy which is characterized by reduced numbers of mitochondria in skeletal muscle fibers. Muscle biopsy reveals fibers with small, poorly defined zones of reduced oxidative enzyme activity; which differentiates it from central core disease where these zones are big and well demarcated [5].
➢ Core-rod myopathy: Presence of cores and rods in separate regions of same or different muscle fibers.
➢ Congenital myopathy: With prominent nuclear internalization, and large and diffused areas of structural disorganization
Congenital myopathies with protein aggregates
This type occurs due to muscle protein aggregation and accumulation in sarcoplasm that eventually leads to muscle dysfunction.
➢ Nemaline myopathy: It is the most common congenital myopathy. It is characterized by generalized muscle weakness and low muscle tone. It gets its name from thread like appearance of rods in the muscle biopsy [6].
➢ Actin filament aggregate myopathy (AFAM) and cap disease: This disease is a variant of nemaline myopathy both in pathogenesis and in clinical features. Muscle biopsy reveals actin filament aggregation in myofibers.
Congenital myopathies with central nuclei
These are inherited disorders characterized by a high incidence of internally placed nuclei in rows in muscle fibers. Its various types are:
➢ Myotubular myopathy: Muscle biopsy shows a characteristic high number of muscle fibers with central nuclei, with a predominance of type 1 fibers. Myotubular myopathy is very rare. It can be either autosomal dominant or autosomal recessive. When caused by a mutation in the DNM2 gene, the disorder is autosomal dominant. When the mutation takes place in the BIN1 gene, the disease is autosomal recessive [7].
➢ Autosomal centronuclear myopathies: It is characterized by triad of morphological features which are characteristic of DNM2-related CNM: [1] radiating sarcoplasmic strands (RSS); [2] increased numbers of central and internal nuclei; [3] type 1 muscle fiber predominance and hypotrophy [8].
➢ “Necklace” fiber myopathy: Necklace fibers are characterized by a cytoplasmic basophilic ring deposit, a few micrometers under the sarcolemma membrane that follows the contour of the cell, in which myonuclei are aligned.
Congenital myopathies with abnormal fiber ratios or sizes
Skeletal muscle is made up of two types of fiber, type 1 and type 2. In this myopathy, patients have abnormal number of type 1 fibers. As a result, they have normal daily functioning but reduced stamina [9].
➢ Congenital fiber type disproportion (CFTD) and congenital neuromuscular disease with uniform type 1 fibers (CNMDU1).
We have described the above case with rare form of myopathy – The Corerod myopathy. This relatively rare form of congenital myopathy is known by the presence of cores and rods in separate regions of same or different muscle fibers. Clinical onset can range from mild presentation (as in our patient) to fetal akinesia. Most of these myopathies are due to mutations in skeletal muscle Ryanodine receptor (RYR1).
No specific treatment is available for these disorders. Management mostly consists of physical therapy, nutritional support, assisted ventilation (if indicated), and genetic counseling.
This case highlights the need to obtain neuromuscular evaluation for patients who present early in life, with minimal weakness pattern which is also slowly progressive. Timely evaluation and diagnosis will allow patients to make informed decision regarding their career choices as well as starting a family.
REFERENCES
- Engel AG, Franzini-Armstrong C. Myology (2nd edn.), MacGraw Hill, New York. 1994:1500-04.
- Romero NB, Clarke NF. Congenital myopathies. Handb Clin Neurol. 2013;113:1321-36.
- Romero NB, Monnier N, Viollet L, et al. Dominant and recessive central core disease associated with RYR1 mutations and fetal akinesia. Brain. 2003;126:2341-49.
- Denborough M A, Dennett X, Anderson RM. (1973). Central-core disease and malignant hyperpyrexia. BMJ. 1973;1(5848):272-3.
- Engel A, Gomez MR, Groover RV. Multicore disease: a recently recognized congenital myopathy associated with multifocal degeneration of muscle fibres. Mayo Clin Proc.1981;46:666-81.
- North KN, Laing NG, Wallgren-Pettersson C. Nemaline myopathy: current concepts: The ENMC International Consortium and Nemaline Myopathy. J Med Genet. 1997;34(9):705-13.
- Centronuclear myopathy. Genetics Home Reference. Lister Hill National Center for Biomedical Communications, U.S. National Library of Medicine, National Institutes of Health, U.S. Department of Health & Human Services. 2012.
- Wilmshurst JM, Lillis S, Zhou H, et al. RYR1 mutations are a common cause of congenital myopathies with central nuclei. Ann Neurol. 2010;68:717-26.
- Jeannet PY, Bassez G, Eymard B, et al. Clinical and histologic findings in autosomal centronuclear myopathy. Neurol. 2004;62:1484-90.