NAFLD and insulin resistance: Cause or results
Received: 23-Oct-2017 Accepted Date: Oct 23, 2017; Published: 25-Oct-2017
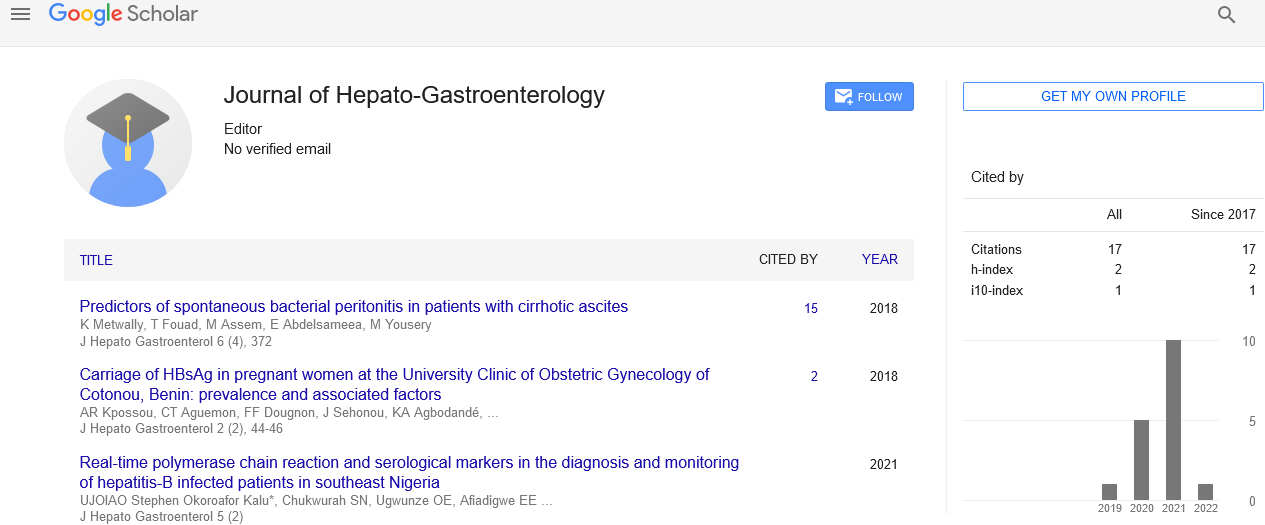
Citation: Hegazy M. NAFLD and insulin resistance: Cause or results. J Hepato Gastroenterol. 2017;1(1):2
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Editorial
Non-alcoholic Fatty Liver Disease (NAFLD) is the most common form of chronic liver disease in adult and children. Liver steatosis is graded based on the percentage of fat within the hepatocytes: grade 0 (healthy, <5%), grade I (mild, 5-33%), grade II (moderate, 34-66%), and grade III (severe, >66%).
NAFLD ranges from simple steatosis, to non-alcoholic steatohepatitis “NASH” that can have different degrees of fibrosis and progress to liver cirrhosis and end-stage liver disease, with its associated complications, including hepatocellular carcinoma.
NAFLD arises in association with one or more features of the metabolic syndrome, namely insulin resistance “IR”, glucose intolerance or diabetes, central obesity, dyslipidemia, and hypertension, so it is now recognized to be the hepatic component of the metabolic syndrome.
The relationships between obesity, diabetes, hyperlipi daemia and NAFLD are influenced by ethnicity. People of African-American descent have significantly less hepatic steatosis in spite of a relatively high prevalence of obesity and diabetes. In contrast, people of Hispanic-American descent have a higher prevalence, while those of primarily Northern European and Asian-American descent have an intermediate prevalence of steatosis. Although there is a constant relation ship between liver triglyceride content and intraperitoneal fat (visceral adiposity) within ethnic groups, there is a substantial degree of dissociation between insulin resistance and both steatosis and visceral adiposity in some ethnic groups. A possible genetic basis for ethnic variation has been identified.
Theoretically fat in the liver cells could accumulate through: Increase delivery of dietary fat or fatty acids “FA” to the liver, increase mitochondrial synthesis of fatty acids or reduced oxidation (electron transport chain activity is reduced to 40-70% of normal in human NASH), impaired export of triglyceride out of the liver cell, and excess carbohydrate delivered to the liver may be converted to fatty acids. Oxidative stress and endotoxin cytokine-mediated injury follow this fat accumulation, leading to hepatic inflammation and fibrosis “multiple hits theory”.
Resistance to the action of insulin results in peripheral lipolysis, increased triglyceride synthesis and increased hepatic uptake of fatty acids Insulin resistance is primarily mediated by excessive FFAs and occur in multiple insulin end-organs including: liver, muscle and adipose tissue. The increased lipolysis associated with obesity provides an increased amount of FFA presented to the muscle. The Randle hypothesis (glucose-fatty acids cycle) was originally proposed to account for the ability of FFAs to inhibit muscle glucose utilization. And because, Insulin itself can up-regulate mitochondrial biogenesis, muscle insulin resistance could provide a mechanism for the reduction in mitochondria.
Insulin resistance is a consistent finding in patients with IGT, and T2DM, and resistance is present years before the onset of diabetes. Elevated FFAs predict the progression from impaired glucose tolerance to diabetes. IR is influenced by a number of factors including age, weight, ethnicity, body fat (especially abdominal), physical activity, and medications. IR is often diagnosed by measuring both the homeostasis model assessment-insulin resistance (HOMA-IR), and the Quantitative Insulin Sensitivity Check Index.
NAFLD as a component of the metabolic syndrome has often been identified with insulin resistance, but only limited studies have carried out actual measurements of insulin sensitivity among this group of individuals. For inter-population comparisons, it is necessary to know normal values of HOMA-IR for each population. Although HOMA-IR has been widely used, there is hardly any consensus on the cut-off points for classification of insulin resistance.
Till now no clear answer for this question; does the liver disease play a primary role in the development of hyper-insulinemia and insulin resistance or it is just a consequence of it? Hope future researches can be able to clarify.